Heat stroke is the most severe pathology related to heat. It is defined as an increase in core body temperature accompanied by signs of neurological dysfunction. In the absence of an early treatment, it has a very high mortality rate.
Topiramate is a well-known drug widely used in epilepsy treatment and migraine prevention. Oligohydrosis has been described amongst topiramate side effects, favouring the risk of hyperthermia and heatstroke.
We present the case of a patient who developed heat stroke due to physical exercise while under topiramate treatment.
Entre las entidades patológicas relacionadas con el calor, el golpe de calor es el más grave. Se define como una elevación de la temperatura corporal central acompañada de signos de disfunción neurológica, presentando una elevada tasa de mortalidad si no se establece un tratamiento precoz.
El topiramato es uno de los fármacos más utilizados en el tratamiento de la epilepsia y en la prevención de las migrañas. Entre sus efectos secundarios, se ha descrito la hipohidrosis, produciendo riesgo de hipertermia y favoreciendo la aparición del golpe de calor.
Presentamos el caso de una paciente que presentó un golpe de calor por ejercicio potenciado por el uso de topiramato.
Heat stroke is the most severe form of heat-related illnesses. It is a medical emergency and is potentially fatal. Heat stroke is characterised by a core body heat of more than 40°C, accompanied by signs of neurological dysfunction caused by failure of the body's thermoregulatory mechanisms.1
It develops most commonly in the first 24–48h following sun exposure because the body-heat regulating mechanisms fail to initiate. Heat stroke can be classified into classical heat stroke, which affects elderly or chronically illindividuals with impaired thermoregulation, and exertional heat stroke, typically found in young individuals doing strenuous activity at high temperatures whose thermoregulatory mechanisms are intact.1–3
Since heat stroke has a high mortality rate, early diagnosis and treatment are crucial.
On the other hand, topiramate, an antiepileptic drug widely prescribed due to its favourable safety profile, is being used increasingly to prevent migraines. Hypohidrosis is one of the described side effects of topiramate, and it can contribute to the development of heat stroke in patients taking this drug.
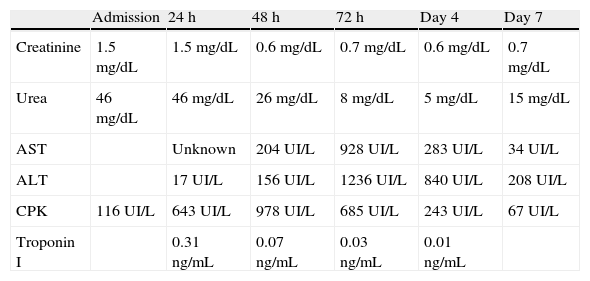
Clinical caseGirl aged 11 years suffering from migraine headaches that had been receiving prophylactic topiramate treatment for 1 year. She cycles regularly and has good exercise tolerance. Following 90min of strenuous exercise during the hottest time of day in the summer, she presented with elevated body temperature, loss of postural tone with no associated movements, and progressive loss of consciousness. Measures of external cooling were initiated in the referring hospital, including removal of clothing, application of cold pads, and hydration by intravenous administration of cooled physiological saline solution (PSS). She was admitted to the Paediatric Intensive Care Unit (PICU) of our hospital in a state of stupor and nearly unresponsive to external stimuli (Glasgow Coma Scale 12/15), with a measured core body temperature of 40.8°C, blood pressure of 70/30mmHg, and heart rate of 170 beats per minute. The main laboratory results were: creatinine 1.5mg/dL, urea 45mg/dL, creatinine kinase (CK) 116U/L, with normal complete blood count, liver function, and levels of glucose and electrolytes. Cranial computed tomography showed no abnormalities. After the patient was diagnosed with heat stroke, external cooling measures and supportive and symptomatic treatment continued, and the patient's temperature was reduced to 38.2°C in the first hour. She presented initially with bradypsychia, incoherent speech, lack of motor coordination, and symmetrical weakness in all 4 limbs. The patient improved progressively and her symptoms had resolved after 12h in the PICU. She did not require inotropic therapy or respiratory support after initial stabilisation. In the first 24h of admission she showed signs of low cardiac output and mild prerenal kidney failure that resolved completely with intravenous fluid therapy. In the second and third day, laboratory tests revealed hypertransaminasaemia and increased CK and troponin levels (maximum values: AST 928IU/L, ALT 1236U/L, CK 978U/L, troponin I 0.31ng/mL). These levels normalised in the course of 3–4 days, so the patient was discharged a week after admission with full resolution of her symptoms and after complete laboratory analysis (Table 1).
Evolution of laboratory results.
| Admission | 24h | 48h | 72h | Day 4 | Day 7 | |
| Creatinine | 1.5mg/dL | 1.5mg/dL | 0.6mg/dL | 0.7mg/dL | 0.6mg/dL | 0.7mg/dL |
| Urea | 46mg/dL | 46mg/dL | 26mg/dL | 8mg/dL | 5mg/dL | 15mg/dL |
| AST | Unknown | 204UI/L | 928UI/L | 283UI/L | 34UI/L | |
| ALT | 17UI/L | 156UI/L | 1236UI/L | 840UI/L | 208UI/L | |
| CPK | 116UI/L | 643UI/L | 978UI/L | 685UI/L | 243UI/L | 67UI/L |
| Troponin I | 0.31ng/mL | 0.07ng/mL | 0.03ng/mL | 0.01ng/mL |
Heat stroke is the most severe form of illness associated to excessive heat. It is a medical emergency most prevalent in July and August. Our patient was seen during the summer after exercising during the hottest part of the day. High heat and strenuous exercise are the two main factors that cause heat stroke in young individuals, with other possible factors including low intake of fluids, the use of drugs that interfere with sweat production, or pre-existing illness.3
The case we present here is one of exertional heat stroke related to the use of topiramate. The latter is a very safe drug used to treat seizures and more recently to prevent migraines. Some of its adverse effects are weight loss (15%), anorexia (8%), paresthesias (38%) orsomnolence (8%). Another side effect has been described since 2000: hypohidrosis, associated to skin dryness, facial flushing, and elevated body temperature.4–6 This new side effect could be attributed to inhibition by topiramate of carbonic anhydrases, enzymes located in the sweat glands that are involved in perspiration.6–9
The characteristic signs of heat stroke are due both to the direct cytotoxic effects of hyperthermia, and to coagulopathy and the systemic inflammatory response syndrome, which can culminate in multi-organ failure and death.10
The main symptoms involve dysfunction of the central nervous system, and range from behavioural changes to a deep stupor or even coma. Mild symptoms can resolve gradually, as happened in the case we are presenting here.
At the cardiovascular level, the hyperdynamic response of the body results in increased cardiac output, decreased peripheral resistance, and arterial hypotension, all of which were observed in our patient.2,3
Kidney damage is one of the earliest clinical manifestations of hyperthermia, brought on by hypotension, dehydration, and rhabdomyolysis. Our patient showed a slight decrease of diuresis with a mild alteration of kidney function, which improved with administration of intravenous fluids.1,2
Muscle injury is more severe in exertional heat stroke due to the local elevation of temperature, hypoxia, and metabolic acidosis associated with exercise. Creatinine kinase is a highly sensitive marker of skeletal muscle injury and its levels appear elevated in 100% of patients with this pathology.2
The liver is the most affected organ in the digestive system, with signs of liver necrosis and elevated AST and ALT levels that can lead to death in up to 10% of cases appearing from the second or third day of heat illness.
Other abnormalities possibly found in these patients include respiratory distress, hypoglycaemia (more common in exertional heat stroke), haematological abnormalities (leukocytosis, bleeding diathesis, anaemia, and even disseminated intravascular coagulation [DIC] in fatal forms of the disease), and electrolyte abnormalities associated to kidney disease and rhabdomyolysis (hyperkalemia, hyperphosphoraemia, and hypocalcaemia).1,8,11
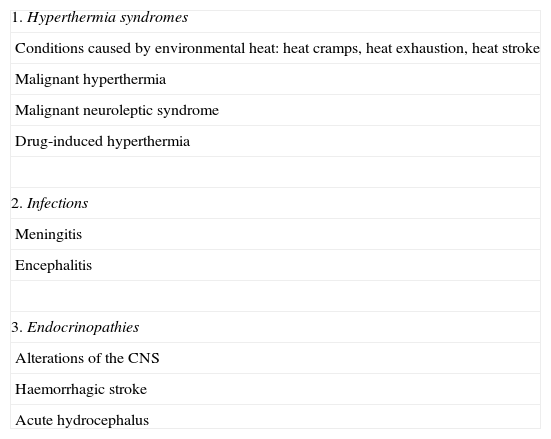
Heat stroke must be diagnosed promptly, as it is a medical emergency and a treatable cause of multi-organ failure. The diagnosis is usually suggested by the medical history, on account of environmental heat and/or performance of strenuous exercise, and by the physical examination, characterised by an elevated body temperature and dysfunction of the central nervous system.2 It must be taken into account that a temperature of less than 40°C can fulfil the temperature criterion if cooling measures have been implemented prior to assessment. The differential diagnosis includes all possible causes of hyperthermia (Table 2).
Differential diagnosis of heat stroke.
| 1. Hyperthermia syndromes |
| Conditions caused by environmental heat: heat cramps, heat exhaustion, heat stroke |
| Malignant hyperthermia |
| Malignant neuroleptic syndrome |
| Drug-induced hyperthermia |
| 2. Infections |
| Meningitis |
| Encephalitis |
| 3. Endocrinopathies |
| Alterations of the CNS |
| Haemorrhagic stroke |
| Acute hydrocephalus |
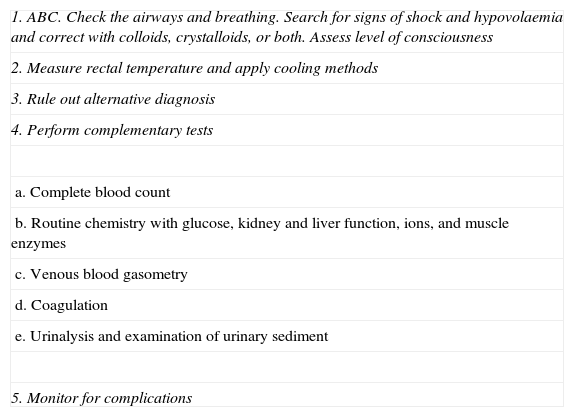
The two main therapeutic objectives are immediate cooling and support of organ–system function (Table 3). The body temperature must be reduced to less than 39°C. This can be achieved by means of external cooling methods (wetting skin by application of cold pads, moving the patient to a shaded area, and removal of clothing) or of internal cooling methods, which are more controversial (administration of chilled intravenous solution, and in rare instances peritoneal lavage with PSS cooled to 20°C, gastric lavage with PSS cooled to 9°, or haemodialysis or cardiopulmonary bypass with external cooling of the blood). Antipyretics are ineffective, as their action requires the proper functioning of the hypothalamic thermoregulation centre, which is abnormal in these patients.3,12,13 The efficacy of sodium dantrolene in the treatment of malignant hyperthermia or malignant neuroleptic syndrome is still under debate.
Initial management of heat stroke.
| 1. ABC. Check the airways and breathing. Search for signs of shock and hypovolaemia and correct with colloids, crystalloids, or both. Assess level of consciousness |
| 2. Measure rectal temperature and apply cooling methods |
| 3. Rule out alternative diagnosis |
| 4. Perform complementary tests |
| a. Complete blood count |
| b. Routine chemistry with glucose, kidney and liver function, ions, and muscle enzymes |
| c. Venous blood gasometry |
| d. Coagulation |
| e. Urinalysis and examination of urinary sediment |
| 5. Monitor for complications |
The prognosis depends on how early treatment is begun. A delay of just 2h in starting treatment can raise the probability of death to up to 70%.2 Prognosis is also associated to the temperature reached, and is poorer in patients with temperatures higher than 46.5°C. It is also associated to the presence of complications, such as DIC or the persistence of severe neurological abnormalities 8h or more after the onset of symptoms.1
Most patients usually recover from kidney and liver symptoms and neurological abnormalities, which generally resolve when the body temperature returns to normal. Muscle weakness can last months in patients who have had extensive muscle damage with deleterious effects.11,14
To conclude, heat stroke, whether classic or exertional, is a severe condition and its prognosis depends on how early treatment starts. It has been observed that some drugs, such as topiramate, may favour its development, and only one other case similar to the one we present here has been described in the literature.11 Therefore, we would underscore the importance of prevention in patients being treated with topiramate, who should be warned of their increased risk for heat stroke.
Conflict of interestThe authors have not conflicts of interest to declare.
Please cite this article as: Rosich del Cacho M, Pareja Grande J, Martínez Jiménez MD, Latorre Latorre JF, Bejarano Ramírez N, López-Menchero Oliva C. Golpe de calor relacionado con el uso de topiramato. La importancia de la prevención. An Pediatr (Barc). 2014;81:181–184.