Hand eczema is a frequent disease in adults. Diagnosing the cause of hand eczema is difficult due to different classifications. There is lack of evidence on hand eczema and its causes in children.
Material and methodA total of 389 children between 0 and 16 years were identified between 1996 and 2016, from whom 42 (10.8%) with exclusively hand eczema were selected. In all cases a standard battery of epicutaneous patch tests was performed, as well as additional batteries depending on the clinical suspicion. The clinical and epidemiological features of these children were recorded and compared against children with eczema in other locations.
ResultsThe 42 children with hand eczema included 25 (59.5%) girls, and 17 (40.5%) boys, with a mean age of 10.6±3.9 years, and did not differ from that of children with eczema in other locations. The definitive diagnosis after patch-testing was Atopic Dermatitis in 15 cases, Allergic Contact Dermatitis in 14 patients, Endogenous Vesiculous Eczema in 6 cases, Endogenous Hyperkeratotic Eczema in 5 cases, and Irritant Contact Dermatitis in 2 cases. The most frequent allergens detected were thiomersal (9 cases), nickel (5 cases), mercury (5 cases), and cobalt (4 cases).
ConclusionHand eczema is a common condition in children. The most common cause is atopic dermatitis, although cases of allergic contact dermatitis manifesting as hand eczema are not uncommon. Any child with eczema of hands in whom an allergic cause is suspected should be referred for patch- testing.
El eccema de manos es una forma frecuente de eccema en adultos. Su diagnóstico en ocasiones es complejo debido a la existencia de diferentes clasificaciones diagnósticas. Existen pocos trabajos que estudien el eccema de manos y su clasificación en niños.
Material y métodoSe ha identificado a 389 niños entre 0 y 16 años remitidos a la Unidad de Alergia Cutánea de nuestro servicio para estudio con pruebas epicutáneas en el periodo 1996-2016. De entre todos los casos se han seleccionado 42 casos con dermatitis localizada exclusivamente en la mano (10,8% de todos los niños remitidos). En todos los casos se realizaron pruebas epicutáneas parchando la batería estándar, así como baterías adicionales en función de la sospecha clínica. Se recogieron datos epidemiológicos (edad, sexo, antecedentes de dermatitis atópica…), así como clínicos (localización de las lesiones).
ResultadosDe los 42 niños remitidos con dermatitis de la mano, 25 (59,5%) eran niñas y 17 (40,5%) niños. La edad media de los pacientes con dermatitis de la mano fue de 10,6 ± 3,9 años. El diagnóstico definitivo tras la realización de pruebas epicutáneas fue dermatitis atópica en 15 casos, dermatitis alérgica de contacto en 14 pacientes, eccema endógeno vesiculoso en 6 casos, eccema endógeno hiperqueratósico en 5 casos y dermatitis irritativa de contacto en 2 casos. Los alérgenos detectados más frecuentes fueron tiomersal (9 casos), niíquel (5 casos), mercurio (5 casos) y cobalto (4 casos).
ConclusiónEl eccema de manos es una entidad frecuente en niños. La causa más frecuente es la dermatitis atoípica, aunque no son infrecuentes los casos de dermatitis alérgica de contacto que se manifiestan como eccema de manos. Todo niño con eccema de manos en el que se sospeche una causa alérgica debe ser remitido para realización de pruebas epicutáneas.
Hand eczema is a frequent form of eczema. It is characterized by erythema, vesicles and pustules in acute forms and desquamation and fissures in chronic forms.1 The criteria for its diagnosis are vaguely defined, and there are multiple clinical classifications of hand eczema.2
There is also disagreement regarding the role played by allergic contact dermatitis (ACD) and atopic dermatitis in paediatric hand eczema. Some authors recommend performance of epicutaneous tests in all children presenting with hand eczema,3 while others believe that the underlying cause is atopic dermatitis and no further testing is required.4–6
The aim of our study was to establish the prevalence of hand eczema in the paediatric population referred to the skin allergy unit of our hospital, and to identify the most frequent clinical forms of hand eczema and the allergens involved in exogenous allergic forms.
Materials and methodsWe conducted a single-centre, retrospective observational study in which we reviewed the cases of all patients aged 0–16 years referred to the skin allergy unit of the Hospital General Universitario de Valencia for evaluation of hand eczema by means of patch testing between 1996 and 2016. We excluded patients with hand eczema that had eczema in other locations. All patients included in the study had been evaluated with the standard patch test series of the Grupo Español de Investigación en Dermatitis de Contacto y Alergia Cutánea (Spanish Working Group on Contact Dermatitis and Skin Allergy [GEIDAC]) provided by Marti Tor® (Barcelona, Spain), as well as the products provided by the patient and additional tests on a case-by-case basis depending on the clinical suspicion. The allergens were applied on the back of the patient on healthy-appearing skin and covered for 48h with AllergEAZE® Finn chambers (Hamburg, Germany). Patch reactions were evaluated at 48 and 96h, and scored according to the criteria of the International Contact Dermatitis Research Group (ICDRG).
The definitive diagnosis was based on the results of epicutaneous testing and epidemiological and clinical parameters, applying the hand eczema classification proposed by Agner et al.2 (Table 1).
Classification of hand eczema.
| Definition | |
|---|---|
| Atopic hand eczema | Hand eczema in a patient with atopic dermatitis diagnosed according to the modified Hanikin and Rajka criteria. Absence of exposure with irritants or of relevant contact allergy |
| Allergic contact dermatitis | Sensitization to one or more allergens and relevant exposure to this allergen on the hands |
| Irritant contact dermatitis | Documented prolonged or regular exposure to a known irritant and absence of relevant contact allergy |
| Hyperkeratotic endogenous eczema | Chronic eczema with fissures, hyperkeratosis or pulpitis and no vesicles in a patient that does not meet the criteria for atopic dermatitis. Absence of exposure to an irritant or relevant contact allergy |
| Vesicular endogenous hand eczema | Recurrent eczema with vesicular eruptions in patient that does not meet the criteria for atopic dermatitis. Absence of exposure to an irritant or relevant contact allergy |
We compared the frequency of different forms of hand eczema in the paediatric and adult population. We compared the age, sex, prevalence of allergy and prevalence of ACD in children with hand eczema and children with eczema in other locations. We used the Fisher exact test to compare qualitative variables, and the Wilcoxon sum-rank test to compare age between groups.
ResultsBetween January 1996 and December 2015, 5985 patients were referred to the skin allergy unit, of who 389 (6.5%) were children aged 0–16 years; 1153 patients (19.3%) had eczema localized exclusively in the hands, and 42 of them (3.6%) were children.
Table 2 shows the epidemiological characteristics of children with hand eczema and children with eczema in other locations. Of the 42 children with hand eczema referred to our unit, 25 (59.5%) were female and 17 (40.5%) male. The sex distribution of children with hand eczema was similar to the sex distribution in children with eczema in other locations (P=.87).
Epidemiological characteristics of paediatric patients with hand eczema and paediatric patients with eczema in other locations.
| Children with hand eczema n=42 | Children with eczema in other locations n=347 | P | |
|---|---|---|---|
| Age, mean±SD (years) | 10.5±3.5 | 10.6±3.9 | .85 |
| Male sex, n (%) | 17 (40.5) | 146 (42) | .76 |
| ACD diagnosis, n (%) | 14 (33.3) | 137 (39.5) | .38 |
| Positive for > 1 allergen, n (%) | 16 (38.1) | 179 (51.6) | .09 |
The mean and standard deviation of the age of patients with hand eczema was 10.6±3.9 years, with ages ranging between 3 and 16 years. There were no statistically significant differences in age between children with hand eczema and children with eczema in other locations (P=.66).
The final diagnosis made after performance of epicutaneous tests was atopic dermatitis in 15 patients (35.7%), ACD in 14 patients (33.3%), vesicular endogenous eczema in 6 patients (14.3%), hyperkeratotic endogenous eczema in 5 patients (11.9%) and irritant contact dermatitis in 2 patients (4.8%). The prevalence of ACD in children with hand eczema was lower compared to children with eczema in other locations (39.5%), although the difference was not statistically significant (P=.5). Two patients that received a diagnosis of ACD also met the criteria for atopic dermatitis, which had not been diagnosed. Table 3 shows the distribution of the paediatric and adult patients included in the analysis by type of hand eczema.
Final diagnosis in paediatric and adult patients with hand eczema following epicutaneous testing.
| Children with hand eczema n=42 | Adults with hand eczema n=1111 | |
|---|---|---|
| Atopic hand eczema | 15 (35.7%) | 70 (6.3%) |
| Allergic contact dermatitis | 14 (33.3%) | 505 (45.5%) |
| Irritant contact dermatitis | 2 (4.8%) | 203 (18.3%) |
| Hyperkeratotic endogenous eczema | 5 (11.9%) | 103 (9.3%) |
| Vesicular endogenous eczema | 6 (14.3%) | 230 (20.7%) |
The results of patch testing were positive in a total of 16 children (38.1%). The prevalence of contact allergy was lower compared to the other children referred to our unit (51.6%), a difference that was not statistically significant (P=.09).
The allergens detected most frequently where thimerosal (9 cases), nickel (5 cases), mercury (5 cases) and cobalt (4 cases). Table 4 shows a complete list of the identified allergens and their relevance.
Allergens identified most frequently in our case series and percentage of cases in which the allergen was relevant to the eczema.
| Allergen | Total, n=67 | Relevant, n (%) n=19 |
|---|---|---|
| Thimerosal | 9 | 4 (44.5) |
| Nickel | 5 | 0 (0) |
| Mercury | 5 | 3 (60) |
| Cobalt | 4 | 0 (0) |
| Palladium | 2 | 0 (0) |
| Abitol | 2 | 2 (100) |
| Rosin | 2 | 2 (100) |
| Kathon CG® (methylisothiazolinone+methylchloroisothiazolinone) | 2 | 2 (100) |
| Mercapto mix | 1 | 1 (100) |
| Cyanoacrylate | 1 | 0 (100) |
| Citronella | 1 | 1 (100) |
| Formaldehyde | 1 | 1 (100) |
| Combination of fragrances | 1 | 1 (100) |
| Piroxicam | 1 | 1 (100) |
| Diaminodiphenylmethane | 1 | 1 (100) |
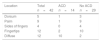
The areas of the hand involved most frequently (Table 5) were the fingertips (12 cases, 28.6%), palms (9 cases, 21.4%), dorsum (5 cases, 11.9%) and sides (4 cases, 9.5%). In 12 cases (28.6%) involvement was diffuse, without a primary site. In patients with ACD, the most frequent type of involvement was diffuse (10 cases, 71.4%), followed by involvement of fingertips (2 cases, 14.3%), dorsum (1case, 7.1%) and palm (1 case, 7.1%) (Table 5).
The sensitization mechanism in patients with ACD was iatrogenic in 8 cases, cosmetic in 2 cases, use of gloves in 2 cases, use of toys (playdough) in 1 case, and use of costume jewellery in 1 case.
DiscussionThe prevalence of hand eczema in the paediatric population referred for epicutaneous testing was 10%. This figure is slightly lower compared to the prevalence reported in other studies conducted in Spain,7 which was probably due to our selection of patients with exclusive involvement of the hands. In studies in adults that selected patients in who eczema was restricted to the hands, the reported prevalence was similar to the one found in our study, ranging between 7% and 15%.1,3–6,8
The mean age of children with eczema was similar to the age of the rest of children referred for testing, with a similar range and comprehending every age group under study. Similarly, we did not find differences in the distribution of eczema by sex between the two groups. This was consistent with other studies that showed that hand eczema manifests in children as well as adults.6,7,9
Overall, endogenous eczema accounted for 62% of cases. However, only half of patients with endogenous hand eczema met the criteria for diagnosis of atopic dermatitis. This finding was consistent with or clinical experience, as we often have patients with hand eczema that cannot be explained by an external cause and who do not meet the criteria for atopic dermatitis. Other studies have found a higher incidence of atopic dermatitis,7–9 which may be due to those studies not including specific classifications of vesicular and hyperkeratotic endogenous eczema.
The second most frequent diagnosis was ACD, which was given to 1 out of 3 children with hand eczema. The fact that some patients with ACD also met the criteria for atopic dermatitis highlights the importance of ruling out a superimposed allergy in patients with hand eczema and atopic dermatitis, as recommended in European clinical practice guidelines.3,10
The main difference in comparison to adult patients was the low prevalence of irritant contact dermatitis in children, which is one of the most frequent causes of hand eczema in adults.2 This may be due to the fact that most cases of hand eczema due to irritant contact result from a regular use of irritants in the home or workplace, something that is uncommon among children. Frequent handwashing or prolonged contact with liquids is also much more prevalent in adults.2 Another difference was the low prevalence of atopic hand eczema in the adult population compared to other endogenous forms of hand eczema. This is consistent with the findings of other studies in adults.2
The allergens involved in cases of ACD in the hands were similar to those found in other studies in adults.4,9 As reported in other publications on skin allergy,11,12 metals were the type of allergen identified most frequently in our study.
Thimerosal was the most frequently identified allergen. However, fewer than half of the reactions to thimerosal seemed relevant to the hand eczema. The reason is that thimerosal is a preservative that is no longer in use. In our study, all cases related to hypersensitivity reactions to thimerosal and mercury involved the use of mercury-based antiseptic solutions that are no longer distributed. At present, allergies to mercury or thimerosal that play a significant role in hand eczema are extremely rare, despite them being the allergens identified most frequently through patch testing in children and adults. This is the reason why the GEIDAC has decided to remove thimerosal from the allergens included in the standard patch test series.13
Nickel and cobalt are very frequent allergens in the paediatric population.10,12,14,15 As is the case with thimerosal, the relevance of sensitization to these substances is frequently dubious.16
The new regulation of the European Commission substantially limiting the amount of nickel and other potentially allergenic metals that can be present in costume jewellery was enacted in 2015.17
Therefore, it is expected that the incidence of cases involving a relevant sensitivity to nickel will decline in upcoming years.12
Rosin and abitol are adhesives used in various products, such as footwear, gloves, or dressings, and in our study they were only detected in cases involving the use of dressings for medical care.18 Sensitization to rosin is also a marker of fragrance allergy, so allergy to fragrances should be ruled out in patients with a positive patch test result for rosin.19 Diaminodiphenylmethane is used as a curing agent in epoxy resins and in the manufacturing of lycra fibres. In our study, hypersensitivity to this substance was associated with the use of plastic gloves.
Following metals and adhesives, preservatives were the third most frequent type of allergen found in children with ACD with hand involvement. The most relevant preservatives are methylchloroisothiazolinone and methylisothiazolinone (MCI/MI). At present, they are the allergens most frequently involved in allergic reactions to cosmetics in adults20–22 and some studies have also reported a high prevalence of sensitization in children.23,24 The reason is that MCI/MI are ubiquitous substances, found in every type of skin care product for children (wet wipes, moisturizing lotions, fragrances) or even craft materials,24,25 and call for a high level of diagnostic suspicion (Fig. 1).
Girl aged 8 years with hand eczema. Epicutaneous tests were positive for Kathon (methylchloromethylisothiazolinone) and formaldehyde, which were considered relevant to the eczema. The allergens were present in craft materials that the patient used regularly. Note the involvement of multiple anatomical subunits.
In our study, the area of the hand that was involved most frequently was the fingertips, unlike other studies conducted in adults where the fingertips were involved less frequently than the palm or the fingers.1,9,26 It is worth highlighting that most cases of ACD manifested in several areas of the hand, without a clear demarcation of lesions. Boonstra et al.9 found similar results, with a much higher incidence of ACD in cases that could not be clearly classified based on the primary site of involvement. This can be explained by the allergen (cosmetics, dressings, antiseptics, …) being in contact with different anatomical parts of the hand at the same time, resulting in the absence of a clear primary site. Thus, ACD is a more likely diagnosis when the lesions are found in multiple areas of the hand as opposed to a single isolated location (palm, dorsum, fingertips).9
In conclusion, hand eczema is a prevalent problem in children. Overall, endogenous eczema is the most frequent type, although only half of patients meet the criteria for atopic dermatitis. It is not rare for cases of ACD to manifest as hand eczema. There are classical allergens (thimerosal, mercury, nickel, …) whose presence is decreasing and whose relevance in allergy is now doubtful. On the other hand, there are emergent allergens (fragrances, isothiazolinones) whose presence is increasing and which call for a high level of suspicion in the diagnosis of allergy. Every child with hand eczema of a suspected allergic aetiology should be referred for performance of epicutaneous patch testing.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Ortiz-Salvador JM, Subiabre-Ferrer D, Rabasco AG, Esteve-Martínez A, Zaragoza-Ninet V, de Miquel VA. Eccema de manos en niños. Estudio clínico-epidemiológico de la población remitida a un hospital terciario. An Pediatr (Barc). 2018;88:309–314.