Hypothalamic hamartomas (HHs) are benign tumours composed of ectopic neural and glial tissue. The prevalence is of 1–2 cases per 100000 inhabitants. HHs can be pedunculated, usually associated to central precocious puberty,1–3 or sessile, associated with epilepsy with gelastic seizures that are commonly refractory to treatment.1–3
We present four cases of HH, which started as precocious puberty in three children and as complex partial seizures and gelastic seizures in one other child.
Of the three patients that presented precocious puberty as the initial symptom, two were female and one male. The girls sought care at ages 2 years (patient 1) and 4 years (patient 2) due to thelarche and accelerated growth rate. Physical examination revealed the patients were at the Tanner II stage. Hormone testing was performed. The results in patient 1 revealed: estradiol, 31.5pg/mL (normal value [NV], 5–10pg/mL); follicle-stimulating hormone (FSH), 3.58IU/mL (NV, 0.50–2.41IU/L); luteinizing hormone (LH), 0.66IU/mL (NV, 0.01–0.21IU/L). The results in patient 2 were: estradiol, 33ng/L (NV, 5–10pg/mL) and a maximum peak level of LH after stimulation with gonadotropin-releasing hormone (GnRH) of 29mIU/mL (NV, <7IU/L). In both cases, bone age was advanced and pelvic ultrasound showed pubertal morphology of the uterus and adnexa.
The third case corresponded to a male 3 years and 10 months of age (patient 3) that sought care for premature pubarche. Physical examination revealed a Prader testicular volume of 5mL. Hormone testing showed a maximum peak level of LH after stimulation with GnRH of 13mIU/mL and a testosterone level of 1.6ng/mL (NV, 0.02–0.23ng/mL). Bone age was advanced compared to chronological age.
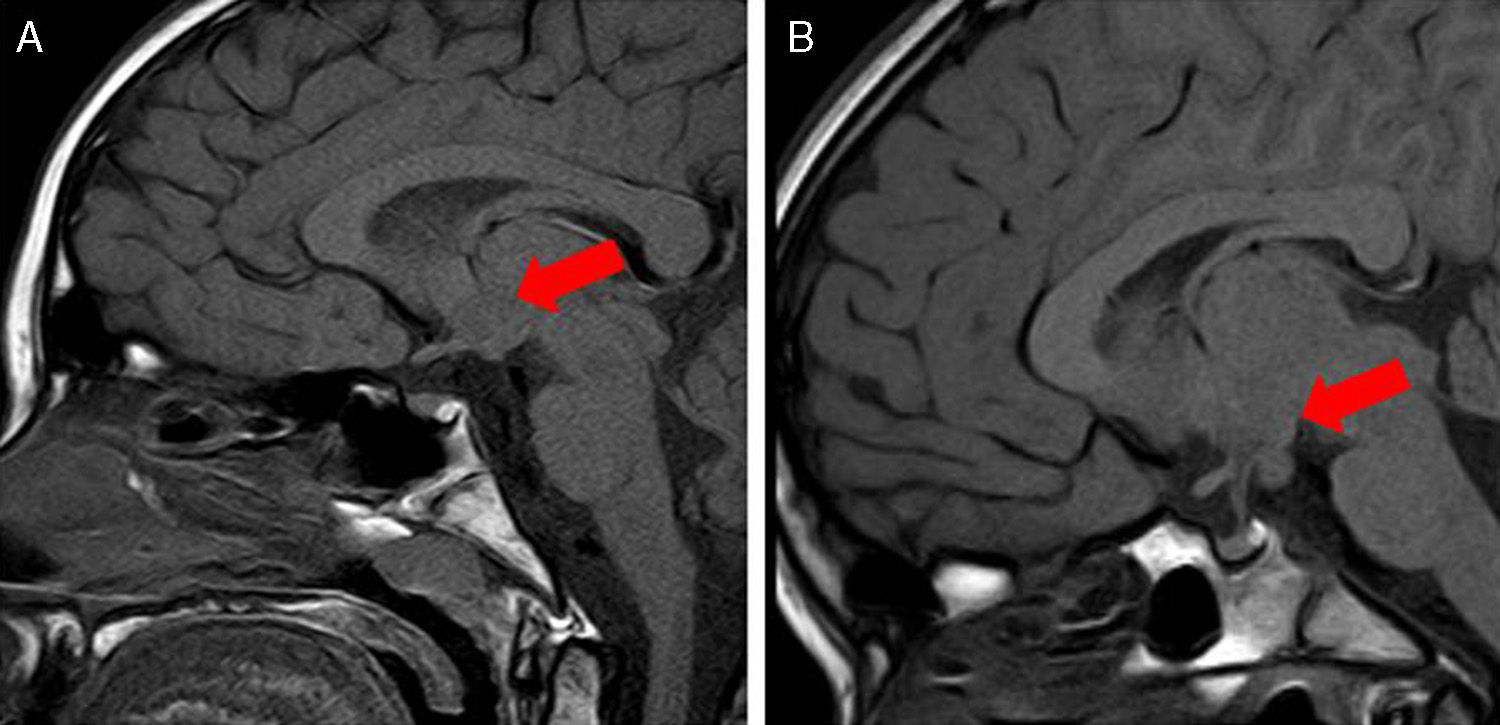
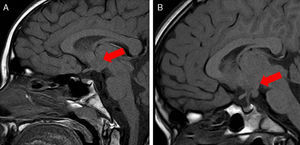
Brain magnetic resonance imaging (MRI) revealed a pedunculated HH, the size of which was 11mm in patient 1, 8mm in patient 2, and 17mm in patient 3, with all three of them located in the tuber cinereum (Fig. 1). All three cases responded well to treatment with a GnRH analogue.
The last case corresponded to a 6-year-old male (patient 4) that sought care for abnormal movements consisting of sucking, chewing and a fixed gaze, occasionally accompanied by deviations of the corner of the mouth, hypertonia, eye rolling and uncoordinated movements of the four limbs. These movements occurred during sleep, with no particular time pattern, and were interpreted as complex partial seizures. Episodes of unprovoked laughter since infancy compatible with gelastic seizures were reported. Treatment with levetiracetam was initiated, with behaviours worsening and poor seizure control despite administration of optimal dosage, so it was switched to valproate.
The patient had disruptive behaviour both at home and in the school, which led to initiation of treatment with risperidone and methylphenidate.
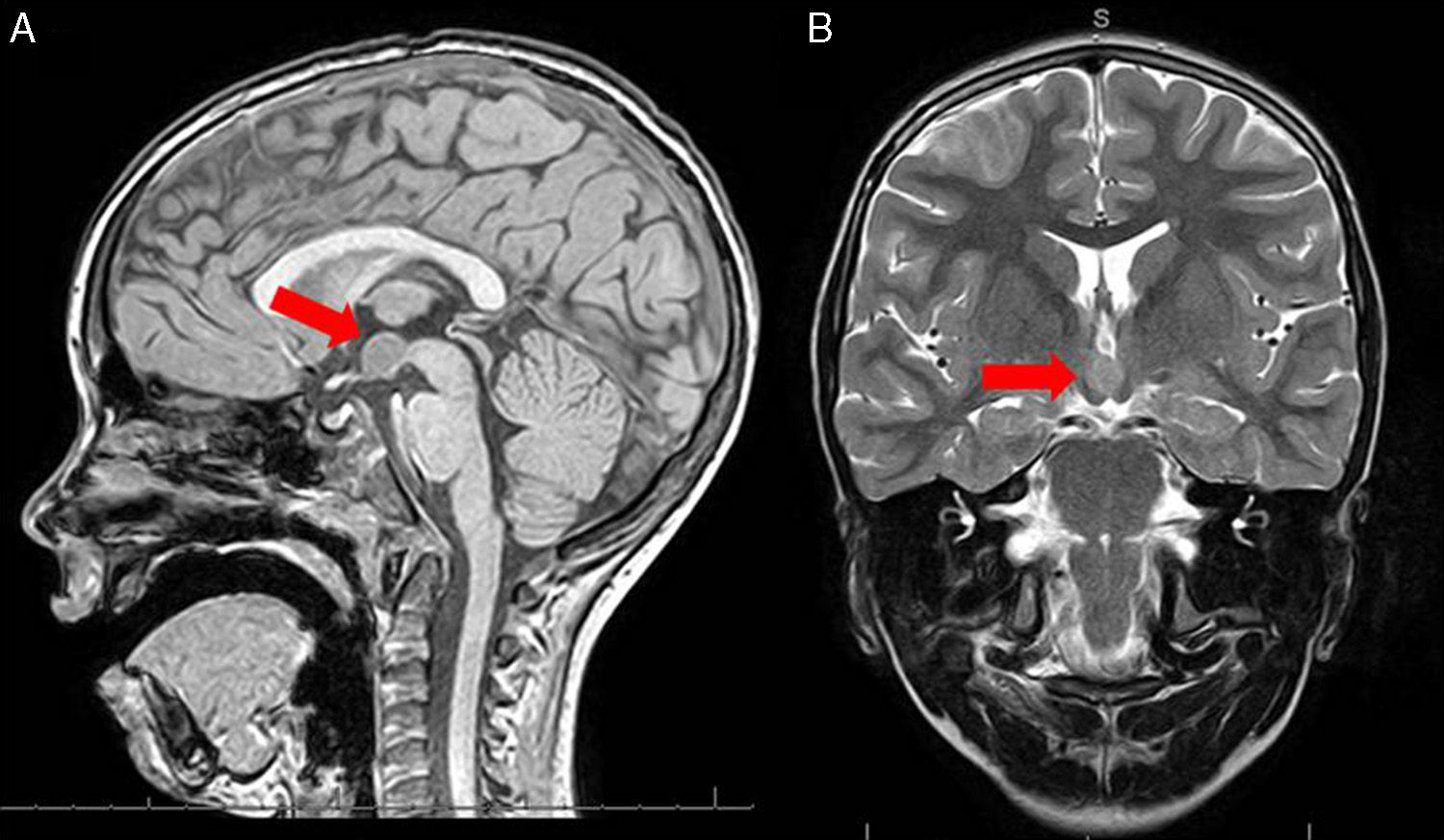
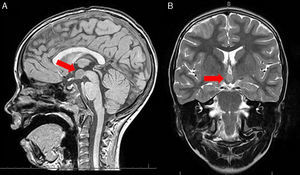
Brain MRI showed a HH 1.3cm in size located between the mamillary bodies (Fig. 2). The screening for precocious puberty was negative.
During followup, the patient showed poor seizure control and a worsening of behaviour despite high-dose treatment with a combination of antiepileptic drugs (levetiracetam, valproate, oxcarbazepine and zonisamide), in addition to methylphenidate and risperidone. Due to the poor response to treatment, we decided to perform gamma-knife radiosurgery.
At present, the patient is receiving antiepileptic treatment with valproate and oxcarbazepine, with good seizure control and an improvement in behaviour, so that treatment with risperidone and methylphenidate could be discontinued. He also requires thyroid hormone replacement therapy for central hypothyroidism secondary to radiosurgery.
Most HHs are sporadic, but sometimes they are associated with Pallister–Hall syndrome.1,2,4 The diagnosis is made by MRI, which shows an isointense lesion with no contrast uptake in the hypothalamic region.
HH has an intrinsic epileptogenic potential, characteristically presenting with gelastic and dacrystic seizures that usually manifest in the early years of life. Other types of seizures difficult to control with pharmacological treatment are also frequent.1,2 It can also manifest as precocious puberty due to GnRH-releasing neurons in the HH. Treatment with GnRH analogues has shown a high efficacy.4
HH is associated with a broad range of neuropsychological symptoms that may include cognitive decline, language delays and learning disabilities, behavioural problems, attention deficit hyperactivity disorder and mood disorders.1 Epilepsy in the context of HH is typically refractory to pharmacological treatment.
Surgical resection of the mass is associated with a high rate of complications. It is indicated in cases of epilepsy refractory to pharmacological treatment, progressive cognitive decline or severe behavioural problems. It is estimated that it achieves seizure control in 50% of cases, with improvement in behaviour and cognition.1,5 Several studies have demonstrated the efficacy of stereotactic radiosurgery (gamma-knife surgery), with outcomes similar to those of conventional surgery and decreased morbidity and mortality,1,6 with the downside that its effects show later (6 months post-surgery) and that sometimes several interventions are required to achieve adequate symptom control.
Please cite this article as: Jiménez de Domingo A, Haro Diaz AM, Miranda Herrero MC, Sanz Fernández M, Aguado del Hoyo A. Formas de presentación clínica del hamartoma hipotalámico. An Pediatr (Barc). 2015;83:60–62