There is currently no unified policy on either breastfeeding support or enteral nutrition practices, as regards human milk (HM) in pre-term newborns. The aim of this study was to describe breastfeeding support measures, as well as the use of HM in very preterm infants in Spanish public hospitals.
MethodA questionnaire on enteral feeding practices was distributed. Data were analysed from units caring for newborns less than 32 weeks or 1500g. A univariate analysis was performed comparing level II and III care units.
ResultsThere was a 91% response rate. A total of 93 units cared for infants less than 32 weeks or 1500g (17 level II and 76 level III), and 49% of the units recorded the breastfeeding rate on discharge. Around 75% (70/93) had a guideline on managing HM (level III 81 vs. level II 47%, P=.002), and 25% had access to donor human milk. Just under half (46%) started trophic feeding in the first 6h. Target enteral feeding volume in stable preterm infants was ≥180ml/kg/day in 89% of the units (level III 93% vs. level II 70%, P=.017). HM fortifier was used in 96% of the units. In 92%, it was added when the required enteral volume was tolerated. In 59% of the units, adjustments in the quantity of fortifier were made according to weight, and in 36%, it depended on analytical criteria. Some units (9%) used pure protein fortifier.
ConclusionsThere is a marked variability in breastfeeding support measures and in feeding practices of preterm infants in Spanish neonatal units.
Actualmente no existe una política unificada de cómo promocionar la lactancia materna en la unidad neonatal ni sobre la práctica de nutrición enteral con leche materna (LM) en los prematuros. Nuestro objetivo fue describir las medidas de apoyo a la lactancia y la utilización de LM en grandes prematuros de los hospitales públicos españoles.
MétodoSe distribuyó un cuestionario sobre prácticas de alimentación enteral. Se analizaron los datos de las unidades que atendían a menores de 32 semanas o 1.500g. Se realizó un análisis univariante comparando las unidades de nivel ii y iii.
ResultadosLa tasa de respuesta fue del 91%. Un total de 93 unidades atienden a menores de 32 semanas o de 1.500g (17 de nivel ii y 76 de nivel iii). El 49% registra la tasa de lactancia al alta. En el 75% (70/93) existe una guía de manejo de LM (nivel iii 81 vs. nivel ii 47%; p=0,002). El 25% dispone de leche donada. El 46% inicia alimentación trófica en las primeras 6h. En el 89% el volumen máximo de LM administrado es ≥180ml/kg/día (nivel iii 93 vs. nivel ii70%; p=0,017). Se fortifica en el 96% de las unidades y el 92% la inicia a partir de un volumen determinado de leche. Para modificar la cantidad de fortificante, el 59% utiliza la curva de peso y el 36% criterios analíticos. El 9% emplea fortificante proteico puro.
ConclusionesExiste una gran variabilidad en las medidas de apoyo a la lactancia y en las prácticas de alimentación enteral de los grandes prematuros en las unidades españolas.
Some authors have reported that the most frequent cause of acquired immunodeficiency is currently exposure to artificial formulas.1 Being aware of this and of the additional advantages of feeding with human milk (HM) for preterm infants, the professionals working in neonatal units seek to foster practices that support breastfeeding. There is currently no unified policy for promoting breastfeeding in neonatal units. Many strategies have been analysed, but in a systematic review in 20092 the most effective measures were kangaroo care, mother-to-mother support, milk expression by double pumping, training of healthcare professionals and accreditation of the associated maternity unit under the Baby-Friendly Hospital Initiative (BFHI), known in Spain as the Iniciativa para la Humanización de la Asistencia al Nacimiento y la Lactancia (IHAN). In spite of all this, preterm infants commence breastfeeding less frequently and for a shorter duration than those born to term.3
On the other hand, there is increasing evidence that proper growth of preterm infants is related to better neurological development.4 However, HM does not cover all the nutritional needs of infants born at less than 32 weeks’ gestation or with a birth weight of less than 1500g. To try to ensure that these infants grow properly, the European Society for Paediatric Gastroenterology, Hepatology and Nutrition, the American Academy of Pediatrics and the World Health Organization recommend that HM should be fortified.5–7 In a Cochrane review in 20048 it was found that preterm infants fed with fortified HM showed greater weight gain and linear and head circumference growth than those that were not fortified. In any case, despite these recommendations, there is no unified policy on enteral feeding practices and HM supplementation in preterm infants.
The objective of this study was therefore to describe the measures supporting breastfeeding and enteral feeding practices with HM in newborns with a birth weight of less than 1500g or a gestational age of less than 32 weeks in Spanish public hospitals. In addition, practices in level II neonatal units were compared with those in level III units.
MethodBetween November 2013 and March 2014 we distributed a questionnaire on breastfeeding support measures among level II and III neonatal units in Spanish public hospitals.
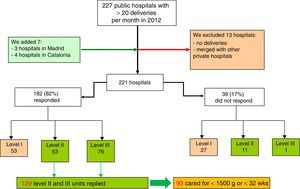
PopulationThere is no official register of the level of healthcare of neonatal units in Spain or of the type of patients they can treat. What are available are the standards of the Spanish Neonatology Society (SENeo in Spanish), with criteria indicating the level of healthcare of each unit. To ascertain our study population, we started from a Ministry of Health list for 2012 which includes hospitals attending more than 20 deliveries per month. Having reviewed the initial list, we added 7 hospitals and excluded 13 (Fig. 1). In total, 221 public hospitals attending more than 20 deliveries per month were detected. The physician in charge of the neonatal unit in these hospitals was sent the questionnaire, in which he or she had to indicate its level of healthcare according to SENeo criteria9 and whether it cared for patients with a birth weight of less than 1500g or a gestational age of less than 32 weeks. The hospitals that did not respond to the questionnaire were contacted by telephone to ascertain their level of healthcare.
Selection of hospitals with level II and III neonatal units according to Spanish Neonatology Society criteria.9
The units were informed of the study in advance in writing. Subsequently the coded questionnaire was sent by email to the physician in charge of each unit. They could respond to it jointly with their team or delegate answering it to another doctor in their unit. We sent email reminders at 15, 30 and 60 days. All data were handled confidentially.
QuestionnaireTo formulate part of our questionnaire we used a questionnaire compiled in Denmark in 2012.10 We contacted the author of the study beforehand to request her permission.
A working group was established consisting of 5 doctors and a neonatal nurse. Four of them were International Board Certified Lactation Consultants. From the Danish questionnaire we selected 51 of the 56 questions it contained, discarding 5 questions because they did not fit the Spanish healthcare system. After a literature review, a first version of the questionnaire with 82 questions was compiled. Subsequently a new group was created with 12 professionals, doctors and nurses, who analysed and answered the questionnaire. The objective was to confirm that the questionnaire we had produced covered all the important issues related to support for breastfeeding in neonatal units and that the questions were clearly formulated. Following this process, 3 questions were added and 2 were removed because they seemed confusing. Finally a consensus was reached and a final questionnaire with 83 questions was obtained. It contained several sections: characteristics of the unit, support measures for families, written protocols and breastfeeding practices, kangaroo care and nutrition of preterm infants with HM. Apart from one open question, the rest were closed, with a series of options to choose from. Generally only one option could be selected, although some questions allowed multiple answers.
This paper presents the results for the units that reported that they provided care to neonates of less than 1500g or less than 32 weeks. It includes 33 questions related to the feeding of these infants specifically and those concerning kangaroo care and milk expression as breastfeeding support measures.
Analysis of the dataThe categorical variables are presented with their absolute and relative frequencies. We compared practices in the level II and level III neonatal units. The statistical significance of the comparison of proportions between the study groups was determined by means of the chi-square test or Fisher's exact test if more than 25% of the cells in the contingency table had expected frequencies of less than 5. A P-value of less than 0.05 was considered statistically significant.
ResultsWe identified 141 level II or level III units in Spain (Fig. 1). The overall response rate was 91% (129/141). Of the units that answered the questionnaire, 76 were level III and 53 were level II. Of the 12 units that did not respond, 11 were level II and 1 was level III. Of those that did answer, 72% (93/129) reported that they cared for newborns with a birth weight of less than 1500g or a gestational age of less than 32 weeks. These 93 units constituted our study population. Of these, 18.3% (17/93) reported that they were level II and 81.7% (76/93) that they were level III. Table 1 shows the distribution of these units by autonomous community.
Distribution of the hospitals that responded to the questionnaire and that care for neonates with a birth weight of less than 1500g and a gestational age of less than 32 weeks.
| Autonomous community | Level II | Level III | Total |
|---|---|---|---|
| Community of Madrid | 4 | 11 | 15 |
| Andalusia | 2 | 12 | 14 |
| Aragon | 0 | 2 | 2 |
| Principality of Asturias | 0 | 2 | 2 |
| Balearic Islands | 0 | 2 | 2 |
| Canary Islands | 0 | 3 | 3 |
| Cantabria | 0 | 1 | 1 |
| Castilla y León | 4 | 5 | 9 |
| Castilla-La Mancha | 1 | 4 | 5 |
| Catalonia | 2 | 12 | 14 |
| Valencian Community | 3 | 5 | 8 |
| Extremadura | 0 | 3 | 3 |
| Galicia | 1 | 6 | 7 |
| Region of Murcia | 0 | 2 | 2 |
| Navarra | 0 | 1 | 1 |
| Basque Country | 0 | 4 | 4 |
| La Rioja | 0 | 1 | 1 |
| Autonomous Cities of Ceuta and Melilla | 0 | 0 | 0 |
| Total | 17 | 76 | 93 |
Table 2 shows the frequency of implementation of recognised measures to support and promote breastfeeding in neonatal units. Here we can see that 49% of the units recorded the rate of breastfeeding on discharge, 60% recommended milk expression within the first 6h after birth and 20% recommended expressing colostrum more than 8 times per day. On the other hand, 27% of the units advocated breastfeeding on demand and 78% used the bottle before feeding at the breast was well established.
Frequency of implementation of recognised measures to support and promote breastfeeding in level II and III neonatal units caring for infants with a birth weight of less than 1500g or less than 32 weeks of gestational age.
| Units | All (N=93) n (%) | Level II (N=17) n (%) | Level III (N=76) n (%) | P |
|---|---|---|---|---|
| Restriction on the presence of parents | 27 (29) | 4 (23) | 23 (30) | NS |
| Written breastfeeding policy at the hospital | 75 (69) | 10 (58) | 55 (72) | NS |
| Breastfeeding rates at discharge recorded | 46 (49) | 10 (58) | 36 (47) | NS |
| Written information on breastfeeding given to parents | 75 (80) | 11 (64) | 64 (84) | NS |
| Mothers advised to begin expression within 6h after delivery | 56 (60) | 7 (41) | 49 (64) | NS |
| Mothers advised to express colostrum more than 8 times per day | 19 (20) | 3 (17) | 16 (21) | NS |
| Mothers advised to express milk at night | 67 (72) | 11 (64) | 56 (73) | NS |
| Breast pumps available for all mothers in the unit | 83 (89) | 17 (100) | 66 (86) | NS |
| Milk expressed in the neonatal unit preferably near the infant | 27 (30) (n=89)a | 4 (23) (n=17)a | 23 (31) (n=72)a | NS |
| Mothers advised to express milk with double pump | 23 (24) | 4 (23) | 19 (25) | NS |
| Freezers available in neonatal units | 76 (81) | 12 (70) | 64 (84) | NS |
| Written guide for storing and handling breast milk at the neonatal unit | 70 (75) | 8 (47) | 62 (81) | 0.002 |
| Unit has a breastfeeding support group | 65 (69) | 9 (52) | 56 (73) | NS |
| Breastfeeding workshops for parents | 26 (27) | 1 (5) | 25 (32) | 0.03 |
| Non-nutritive sucking in kangaroo care in stable neonates | 44 (47) | 4 (23) | 40 (52) | 0.02 |
| Non-nutritive sucking in stable neonates with nasal CPAP | 39 (41) | 5 (29) | 34 (44) | NS |
| Bottle used before breastfeeding is well established | 73 (78) | 13 (76) | 70 (78) | NS |
| Breastfeeding on demand encouraged in the neonatal unit | 26 (27) | 6 (35) | 20 (26) | NS |
| Semi-demand feeding encouraged in the transition period from tube to breast | 33 (35) | 4 (23) | 29 (38) | NS |
| Weight loss accepted in the transition stage from tube to breast | 62 (77) | 11 (64) | 61 (80) | NS |
| Use of pacifier changed in the transition stage from tube to breast | 30 (32) | 8 (47) | 22 (28) | NS |
| Kangaroo method encouraged | 91 (97) | 16 (94) | 75 (98) | NS |
| Early kangaroo care in stable infants (in the first 24h or when the parents first come) | 47 (61) (n=77)a | 10 (76) (n=13)a | 37 (57) (n=64)a | NS |
| More than 2h per day of kangaroo care in stable infants | 64 (82) (n=90)a | 14 (87) (n=16)a | 60 (81) (n=74)a | NS |
NS: difference not significant.
Table 3 shows the responses on enteral feeding practices with HM and the use of fortifiers. It reveals that 46% of the units began trophic feeding in the first 6h of life, that 25% had donor milk available and 96% routinely fortified HM.
Enteral feeding practices and the use of fortifiers in preterm infants with a birth weight of less than 1500g or a gestational age of less than 32 weeks.
| Units | All (N=93) n (%) | Level II (N=17) n (%) | Level III (N=76) n (%) | P |
|---|---|---|---|---|
| Commencement of enteral feeding | ||||
| <6h of life | 43 (46) | 10 (58.9) | 33 (43) | |
| <12h of life | 19 (20) | 3 (17.6) | 16 (21) | NS |
| <24h of life | 24 (25) | 4 (23.5) | 20 (26) | |
| <48h of life | 7 (7) | 0 | 7 (10) | |
| Maximum amount of breast milk in stable preterm infant≥180ml/kg/day | 82 (89) (n=92)a | 12 (70) (n=17)a | 70 (93) (n=75)a | 0.017 |
| Use of donor milk | 24 (25) | 1 (5) | 23 (30) | NS |
| Fortification normally used | 89 (96) (n=92)a | 15 (88) (n=17)a | 74 (98) (n=75)a | NS |
| Preterm infants that are candidates for fortification | ||||
| All | 17 (18) | 4 (25) | 13 (17.5) | |
| <1500g or <32 weeks | 70 (78) | 12 (75) | 58 (78.5) | NS |
| <1000g or <28 weeks | 3 (3) (n=90)a | 0 (n=16)a | 3 (4) (n=74)a | |
| Criterion for beginning fortification | ||||
| From a set quantity of enteral nutrition | 82 (92) | 15 (88) | 67 (93) | |
| The weight curve is poor | 7 (7) (n=89)a | 2 (11) (n=17)a | 5 (7) (n=72)a | NS |
| Criteria for adjusting fortification | ||||
| Analyses | 28 (36) | 5 (29) | 23 (38) | |
| Weight curve | 46 (59) | 10 (58) | 36 (60) | NS |
| Milk composition | 3 (3) (n=77)a | 2 (11) (n=17)a | 1 (1) (n=60)a | |
| Use of protein fortifier | 9 (9) (n=92)a | 0 (n=17)a | 9 (12) (n=75)a | NS |
| How are preterm infants with a poor weight curve on discharge and exclusive breastfeeding fortified? | ||||
| Preterm infant formula | 65 (69) | 14 (82) | 51 (67) | NS |
| Fortifier in breast milk | 26 (27) | 4 (23) | 22 (28) | |
| Hindmilk fraction of expressed breast milk | 12 (12) | 4 (23) | 8 (10) | |
NS: difference not significant.
Tables 2 and 3 show the overall results and the comparison by levels of healthcare. Significant differences were found in 4 of the 33 measures analysed, in that they were implemented in a higher proportion of level III units compared with level II (written guide for storing/handling HM, non-nutritive breast sucking in kangaroo care, breastfeeding workshops for parents and maximum quantity of HM greater than 180ml/kg/day).
DiscussionThis national survey, with a high response rate, showed great variability in policies for promoting and supporting breastfeeding in neonatal units caring for newborns with a birth weight of less than 1500g or a gestational age of less than 32 weeks. Nevertheless, there was room for improvement in the implementation of almost all the measures. Several of the practices studied were significantly more often implemented in level III units than in those of level II. Great diversity was also detected in enteral feeding practices with HM. The great majority of the units routinely used fortifiers, although it is very striking that there were 3 units that did not fortify HM.
It has been amply demonstrated that practices in neonatal units have a decisive influence on the frequency of initiating breastfeeding and on its duration. Just as practices differ, so do rates of breastfeeding on discharge.11,12 We did not include rates of breastfeeding on discharge in our study because only 49% of the units recorded it. In a recently published study13 where only 9 items are identified as healthcare quality indicators for neonatal units, breastfeeding on discharge is included in sixth place. It would therefore be desirable for units caring for newborns with a birth weight of less than 1500g to record this piece of information so as to identify which practices ought to be changed in order to increase the rate of breastfeeding on discharge.
Of the Spanish units that responded to the survey 29% still maintained restrictions on parents entering the neonatal unit. Cuttini14 detected a higher proportion of breastfeeding infants in units open to parents when they were compared with units with restrictive policies. The results support the possibility that having units open 24h a day could have a positive effect on the frequency of breastfeeding in neonatal units. In addition, having parents present in neonatal units without restriction of hours favours the practice of kangaroo care.
With regard to kangaroo care, one of the most efficient strategies for promoting breastfeeding,2 the results of our survey show that practically all the units encouraged parents to practise the kangaroo method. However, only 60% of the units performed it at an early stage and nearly 20% of the units reported that the mean daily amount of kangaroo care time was less than 2h. These 2 issues are important, because performing it early helps to establish breastfeeding and the amount of kangaroo care time has a dose–response effect on milk production: the more time is devoted to kangaroo care, the greater the milk production. Moreover, only half the units allowed non-nutritive sucking on the breast during kangaroo care in stable preterm infants, the proportion being significantly higher in level III units (52% vs 23%; P<0.02). This made the transition from tube to breast more difficult, as did the fact that only 27% of the units allowed breastfeeding on demand and 78% used the bottle before breastfeeding was well established.
Strategies to initiate milk expression early and frequently, recommending night-time expression, make it easier for breastfeeding to be maintained.15 In this respect many of the neonatal units should modify the recommendations they give to mothers, because approximately a third of the units did not recommend very early expression or night-time expression. It is very striking that only 20% of the units encouraged mothers to express colostrum more than 8 times a day and only 25% recommended expression with a double breast pump. Even if a very small volume of colostrum is obtained, increasing attention is being given to its early administration in the newborn's mouth.16 In our survey only 46% of the units began enteral feeding in the first 6h of life. In addition, it is also surprising that only 1 in every 4 units advised expressing milk near the infant. It has been demonstrated that the volume of milk obtained by expression is greater when it is expressed near the infant, especially if it is done immediately after performing kangaroo care.17
Another striking aspect of the survey is that 1 in 5 centres did not have freezers for HM in the neonatal unit and 1 in 4 had no written guide on HM handling routines.
These two issues are essential, because not only must we be concerned about the safety of milk, but our aim must be for the milk to maintain its quality throughout all the processing it undergoes in the units (freezing, thawing, refrigeration, administration, etc.). Some studies have described how during freezing and refrigeration milk is acidified and its quality therefore declines.18,19 Unless we can ensure that HM is properly stored at optimum temperatures, this loss of quality will increase.
Only 1 in 4 units had donor milk available to avoid infants of very low weight being exposed to artificial formulas at an early stage. Although the number of milk banks in Spain is increasing and there are currently 8 of them, an effort should be made to ensure that all neonatal units caring for infants with a birth weight of less than 1500g have access to donor milk.
Three units reported that they did not use fortifiers despite the fact that HM does not cover the nutritional needs of very low birth weight infants, especially as regards protein, calcium and phosphorus intake.8 The great majority of units initiated fortification when the intake of HM reached a specific quantity, but 7% only fortified if the weight curve was poor. To modify the amount of fortifier, approximately 60% of the units fortified in a standard manner and nearly 40% practised adjustable fortification based on analytical parameters. Only exceptionally (in 3 units) was targeted fortification implemented, based on the composition of the HM administered to the infant. There were also few units that used pure protein fortifier to be able to increase protein intake when the maximum concentration of normal fortifiers had been reached and urea levels still remained low. This practice of using an extra protein supplement has shown to produce an improvement in infant's growth.20
Of the 33 practices analysed, 4 were significantly more widely established in level III units than in those of level II. This result is consistent, because virtually all the other practices were more commonly implemented in level III units, even if the difference was not significant. It is surprising that the 17 level II units included in the study reported caring for infants with a birth weight of less than 1500g, since level II care by definition excludes care of these infants. This suggests that although SENeo9 has clearly established the tasks to be performed at each level of healthcare, this is not observed in practice.
The results obtained in this study have identified great diversity among units in the patterns of feeding of preterm infants. These results are comparable with those obtained in other surveys carried out in other countries,21–23 in which wide variability has also been detected. For example, in a survey of level III neonatal units in 8 countries conducted in 2010,21 48% had access to donor milk, but the figure varied between 7% and 100% depending on the country. As regards the maximum volume of HM in stable preterm infants, only 9% of the units exceeded 180ml/kg/day, and in the UK and Ireland, for example, only 68% of the units routinely fortified HM. Moreover, in a study performed in the UK and Ireland in 2007,23 differences were also detected between neonatal units of different levels of healthcare, in this case in respect of the frequency of fortification of HM.
One of the limitations of this study concerns the lack of information on the rate of breastfeeding on discharge from the neonatal unit. It would have been very interesting to know whether some relationship could be established between practices and breastfeeding rate. On the other hand, the results are those reported in the questionnaire and we cannot confirm that the practices really are as reported. This is a limitation common to all studies conducted by questionnaire.
The healthcare professionals and the atmosphere of the neonatal unit play a very important part in determining the start and continuation of breastfeeding in preterm infants. As the result of this survey shows, Spanish neonatal units still have a long way to go before the breastfeeding support and promotion practices that have proved effective are universally adopted, and before routines are incorporated to ensure the quality of HM and an adequate nutritional intake to improve the growth of infants with a birth weight of less than 1500g. Creating evidence-based protocols agreed among all the professionals involved could reduce the differences between units.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors wish to thank the Research Network for Child and Maternal Health and Development (Red SAMID in Spanish) (Ref. RD12/0026/0007) and the Neonatal Units that took part in the study for their support.
Please cite this article as: Alonso-Díaz C, Utrera-Torres I, de Alba-Romero C, Flores-Antón B, López-Maestro M, Lora-Pablos D, et al. Prácticas de alimentación con leche materna en recién nacidos menores de 1.500g o de menos de 32 semanas. An Pediatr (Barc). 2016;85:26–33.
VIII Spanish Congress of Breastfeeding held in Bilbao from 26 to 28 February 2015. XXV Congress of Neonatology and Perinatal Medicine held in Seville from 20 to 22 May 2015.