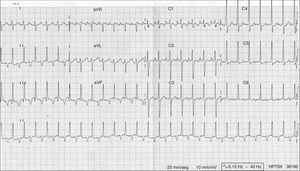
Permanent junctional reciprocating tachycardia, also known as Coumel's tachycardia, is a rare form of supraventricular tachycardia that is usually incessant, characterised by retrograde conduction via an accessory pathway usually located in the posteroseptal region with slow and decremental conduction.1 Its characteristic electrocardiographic features (Fig. 1) are regular tachycardia with a narrow QRS complex, a long RP interval (RP>PR) and an inverted P-wave in the inferior leads (II, III and aVF).2 It is usually diagnosed during childhood, or even prenatally, and may cause tachycardia-mediated cardiomyopathy, although it may be asymptomatic and diagnosed in the course of a routine examination.3 It is usually refractory to medical treatment, and ablation of the accessory pathway by means of radiofrequency is considered a safe and effective definitive treatment.1
We conducted a retrospective descriptive study of paediatric patients with a diagnosis of Coumel's tachycardia followed up at a tertiary level hospital in 2014 and 2015 to assess their outcomes.
Seven patients were followed up during these two years, of who 57.1% were boys and 42.9% girls. One patient received an early prenatal diagnosis and 2 received the diagnosis after tachycardia was detected in the foetus during monitoring before birth, requiring urgent caesarean delivery due to uncontrolled foetal tachycardia in all 3 cases. In the case with prenatal diagnosis of foetal tachycardia, the mother was treated during gestation with flecainide and digoxin, with no apparent response. The mean age of diagnosis in the remaining patients—excluding those 3—was 4.6 years (±3.7 years). In only one case, the patient was referred from the primary care centre for evaluation of palpitations, while the other 3 were chance findings during routine examinations. The newborn with a prenatal diagnosis had tachycardia-mediated cardiomyopathy and underwent ablation of the accessory pathway at 14 days post birth due to nonresponse to medical treatment. Pharmacological treatment was only effective in 2 patients (28.5%), while 5 patients (71.5%) underwent ablation of the accessory pathways, which had to be repeated in 2 (40%). There were no significant complications of any of the procedures.
Permanent junctional reciprocating tachycardia is an uncommon disease that may go unnoticed due to its limited manifestations. In our series, only one case was diagnosed after the patient presented with palpitations, while the others were chance findings (except in cases of prenatal diagnosis). The literature describes cases with different presenting symptoms: palpitations, syncope, congestive heart failure secondary to incessant tachycardia and in some cases sudden death due to ventricular fibrillation.2 In most patients, the tachycardia is well tolerated so the symptoms may go unnoticed.
We did not find any structural abnormalities in the patients in our series, which is consistent with the literature.4,5 Pharmacological treatment is effective in only half of the patients, and radiofrequency ablation of the accessory pathway may need to be performed, in some cases more than once. Antiarrhythmic drug therapy is reserved for cases with mild symptoms, without ventricular dysfunction and with occasional episodes of tachycardia,4 or for symptomatic patients before ablation. Although the natural history of this disease is not well known, it is believed that ablation should be contemplated at an early stage in these patients.1 Since the involved pathway is usually posteroseptal, there is a risk of damaging the coronary artery with the use of radiofrequency, but this complication has been rare in the case series that have been published recently. An alternative treatment is cryoablation of the accessory pathway, which carries practically no risk of coronary artery damage, but is associated with a higher recurrence rate.3
Please cite this article as: Cardiel Valiente L, Ayerza Casas A, López Ramón M, Jiménez Montañes L, Sarquella-Brugada G. Nuestra experiencia con la taquicardia reciprocante permanente de la unión aurículo-ventricular. An Pediatr (Barc). 2017;87:173–174.