The rate of premature births has significantly increased, and it is important to determine its effects. The objective of this study is to determine the psychomotor development profile of a group of children born prematurely, at the age of 4, 5 and 6, and to compare them with a group of full-term birth children, in order to detect any differences.
Patients and methodsThe sample consisted of 98 participants, evenly distributed into two groups, premature and full-term born children. A prospective longitudinal observational analytical study, with a design of cases and controls, was carried out. For some analyses, the separation into early pre-term, moderate pre-term, and late pre-term was considered. The evaluations were performed using the McCarthy Scale of Aptitudes and Psychomotor skills for children.
ResultsThe data show achievements within the middle intervals. However, there are more difficulties in development at 4 years in the group of premature children, according to gestational age. Early pre-term (gestational age less than 32 weeks) showed significantly lower scores compared to moderate and late pre-term, mainly at 6 years, and with those born at term, at 4 and 6 years.
ConclusionsDevelopment difficulties are greater at a lower gestational age, and may affect the Primary Education stage. The need to monitor all premature children in the preschool stage is suggested, as well as to evaluate more specific skills and continue with the care from specialist teams.
En las últimas décadas, el nacimiento de niños prematuros se ha incrementado notablemente, siendo importante conocer sus efectos. El objetivo del estudio es determinar el perfil de desarrollo psicomotor de niños con antecedentes de prematuridad, a los 4, 5 y 6 años, y compararlos con un grupo de niños nacidos a término para detectar posibles desajustes.
Pacientes y métodosLa muestra estaba constituida por 98 participantes, distribuidos uniformemente en dos grupos, prematuros y a término. Se realizó un estudio de cohorte prospectivo longitudinal analítico observacional con un diseño de casos y controles. Se ha considerado la división del grupo prematuro en muy prematuros y prematuros moderados y tardíos. Las evaluaciones se realizaron con las Escalas McCarthy de Aptitudes y Psicomotricidad para niños.
ResultadosLos datos muestran logros dentro de los intervalos medios. No obstante, se evidencian más dificultades en el desarrollo a los 4 años en el grupo de prematuros. Atendiendo a la edad gestacional, los muy prematuros (edad gestacional menor a 32 semanas) muestran puntuaciones significativamente más bajas con respecto a prematuros moderados y tardíos, fundamentalmente a los 6 años, y con los nacidos a término, a los 4 y 6 años.
ConclusionesA menor edad gestacional, son mayores las dificultades, pudiendo afectar en la etapa de Educación Primaria. Se considera la necesidad de efectuar un seguimiento a todos los prematuros en la etapa preescolar, así como evaluar habilidades más específicas y continuar con la atención desde equipos especializados.
Every year, approximately 15 million children are born preterm (PT), and this number continues to increase,1,2 resulting in one of the most important problems in child health due to its frequency and associated morbidity and mortality, on one hand, and its considerable social and economic costs on the other.3,4 Thus, it is essential that we are aware of the problems that may be associated with preterm birth to be able to intervene as soon as possible, as the existing evidence proves that preterm birth may affect the development of individuals throughout the lifespan.4,5
The degree of prematurity may have an impact on the development of the child depending on the gestational age (GA) at the time of birth, and the most widely used classification used at present establishes the categories of extremely preterm (< 28 weeks GA), very preterm (28–32 weeks GA) and moderate to late preterm (32–37 weeks GA).6,7
In the population of PT children, the most frequent problem is cognitive developmental delay.8 The literature reveals a higher frequency of problems between ages 4 and 6 years,9 with evidence of an association between the level of development and the GA at birth, with a negative correlation between the level of cognitive impairment and GA.10,11 Neuroimaging studies have yielded similar results,12 with evidence of decreased cerebral volumes in specific regions in children born before 33 weeks’ gestation in association with poorer cognitive outcomes.13 More recently, a study in a sample of 54 children aged 4–5 years, half of which had been born very PT, concluded that PT children exhibit neurocognitive impairment in every aspect of cognition under study.14 Although there is no consensus on the eventual outcomes of these differences,15 there is evidence suggesting that with increasing GA, differences in overall developmental outcomes narrow and even disappear.16,17
As regards specific areas of development, the evidence shows that verbal language and motor skills are most affected.18–20 Concerning verbal skills, Ment et al. evaluated 296 children born with weights ranging from 600 to 1250 g at ages 3, 4 ½, 6 and 8 years and found that most PT infants exhibited improvement in verbal skills with increasing age.21 Rodríguez et al. found that verbal performance was the most impaired area of development between ages 3 and 5 years,22 while Aarnoudse-Moens et al. found that children born before 30 weeks’ gestation had poorer verbal fluency compared to children born at term.23 In opposition, there have been studies that found normal development of verbal skills in children born PT.24,25
When it comes to motor skills, the evidence suggests that neurodevelopmental impairment may increase with decreasing GA.10 Fernández et al. described sequelae in the neurologic development of children with a history of preterm birth and extremely low birth weight, concluding that psychomotor retardation is one of the most significant complications in these children at age 2 years.26 In a sample of extremely and very preterm infants evaluated between ages 40 and 86 months, Millar et al. found mild neuromotor impairment.27 In contrast, Shapira et al. found that 68% of children born PT with a weight of 1500 g or lower had scores in the normal range at age 3 years.24
When it comes to the development of mathematical skills in PT infants, the works we reviewed that focused on early childhood did not provide data on the level of competence in numerical reasoning. However, we found that these children may exhibit difficulties with arithmetic at ages 5 and 10 years,28,29 with skills in this area improving over the years corresponding to primary education.28
On the other hand, there is evidence that children born PT have memory and attention deficits,30 which may have an impact on long-term memory.31
In short, preterm birth seems to have a significant impact on neurodevelopment,32 but the published evidence on developmental outcomes during early childhood is scarce, and follow-up of these children may be necessary for early detection and management of deficits that may manifest starting from age 2 years, as they pose a risk of significant delay once these children start compulsory education.33
Most research focuses on outcomes through age 24 months, and there is a dearth of data on the evolution of potential delays in the preschool years and early years of primary education,34 and the lack of conclusive results causes uncertainty. The aim of our study was to assess psychomotor development in a group of children born preterm (PT group) at ages 4, 5 and 6 years and compare it with development in a group of children born at term (T group), also taking into account the degree of prematurity (PT1 and PT2 groups). Our findings will help us understand developmental patterns in this at-risk group as they enter the educational system, which is necessary for the purpose of developing preventive interventions aimed at improving the skills of PT children at the time they start compulsory education.
Sample and methodsWe conducted a longitudinal prospective observational and analytical case-control study in a group of children with a history of preterm birth without severe sequelae at age 4 years and a group of children born at term, with both groups having similar distributions in terms of sex and chronological age.
The sample comprised 98 participants residing in a province in southern Spain, evenly distributed in 2 groups: preterm group (GA < 37 weeks) and term group (GA ≥ 37 weeks). We evaluated children in both groups at 3 time points (ages 4, 5 and 6 years).
The initial population of PT children (< 37 weeks) comprised 116 children residing in the same province admitted to the NICU of a tertiary care hospital, of who 14 experienced severe sequelae. A total of 102 PT children were eligible for inclusion, but 25 families could not be reached or refused to participate in the study, and 5 did not attend the initial evaluation. Thus, we obtained a representative sample of 72 children, with a margin of error of 0.05. The values applied for calculating the necessary sample size were an α of 0.05, a 95% confidence level (z = 1.96) and an assumed proportion of 0.2. We based our estimate of the proportion on the work of Gómez et al. (2019), who found a proportion of PT infants with temporary complications of 20%.35 During the study follow-up, we excluded another 23 cases from the study due to unavailable or incomplete data. The PT group in the final sample included 20 boys and 29 girls with a mean birth weight of 1555.05 g. The mean maternal age at birth was 33 years, 73.46% of children were product of a first pregnancy, and 71.5% were delivered by caesarean section (Table 1).
Demographic and clinical characteristics of the preterm group.
| χ (SD) | Range | n (%) | |
|---|---|---|---|
| GA (weeks) | 31.4 (2.2) | 23−35 | |
| Weight (g) | 1.559 (413) | 700−2.498 | |
| Length of ICU stay | 28.8 (24.5) | 2−123 | |
| Maternal age | 33 (5.5) | 19−44 | |
| [0,1–4]Type of delivery | |||
| Spontaneous vaginal | 9 (18.3) | ||
| Induced | 5 (10.2) | ||
| Caesarean | 35 (71.4) | ||
| [0,1–4]Sex | |||
| Female | 29 (59.18) | ||
| Male | 20 (40.81) | ||
| [0,1–4]Previous pregnancies | |||
| None | 36 (73.46) | ||
| 1 | 10 (20.40) | ||
| 2 | 3 (6.12) | ||
GA, gestational age; SD, standard deviation.
Range: minimum-maximum.
We selected the T group, which comprised 20 boys and 29 girls born at term without special health care or education needs, from the different schools attended by participants in the PT group. The T group was selected by convenience sampling, with participants matched for sex and date of birth to schoolmates in the PT group.
To assess the potential impact of the degree of prematurity, we took GA into account creating PT categories, with the PT1 group including 12 boys and 19 girls (n = 31) born at a GA of less than 32 weeks (very PT + extremely PT) and the PT2 group including 8 boys and 10 girls (n = 18) born at a GA of 32+0 to 36+6 weeks (moderately PT + late PT).
We assessed psychomotor development at ages 4, 5 and 6 years using the McCarthy Scales of Children's Abilities (MSCA),36 which include 18 independent subtests grouped into 6 scales (Verbal, Verbal, Perceptual-Performance, Quantitative, General Cognitive, Memory, and Motor) and also provide a composite score known as the general cognitive index (GCI). Scores in every scale have a mean value of 50 and a standard deviation of 10 (40–60) except for the GCI, with a mean of 100 and a standard deviation of 16 (84–116).
This test has sufficient psychometric power. The reported mean reliability coefficient for the GCI is 0.93, and the reliability coefficients for the other scales range between 0.79 and 0.88. As for stability, the reliability coefficients range from 0.75 to 0.90. The validity of the MSCA has been demonstrated by several studies that have found a correlation between the MSCA scores and the IQ scores of the Wechsler Preschool and Primary Scale of Intelligence (WPPSI) and the Stanford-Binet scales.37,38
We selected the PT group based on the criterion of PT birth out of the children born in the aforementioned hospital in 2 phases over a period of 2 years. We contacted parents to inform them about the study and requested the participation through an informed consent form developed for the purpose. We scheduled appointments to perform evaluations at ages 4, 5 and 6 years. The study was approved by the regional Biomedical Research Ethics Committee, and it adhered at all times to the ethical principles of the Declaration of Helsinki. To recruit the T group, we contacted the schools where the children were enrolled and requested their collaboration. After an initial selection based on age and sex, we contacted parents to inform them of the study and obtained signed informed consent.
We matched the assessments of both groups in age and time. We performed nonparametric tests (Mann-Whitney U test for intergroup comparisons, Wilcoxon test for longitudinal intragroup comparisons and Kruskal-Wallis test to compare the 3 groups under study once we subdivided the PT group) since the distributions did not meet the assumption of normality. We performed the analyses with the software SPSS version 24.0 for Windows and defined statistical significance as a p-value of less than 0.05. To calculate the effect size, since the tests used were nonparametric, we used the r(equivalent) proposed by Rosenthal to assess the association between the differences in 2 study variables, categorising the effect size into small (0.10), medium (0.30), large (0.50) or very large (0.70) based on the result.39
ResultsThe sample included 98 participants (50% born preterm and 50% born at term). To assess the impact of GA, we subdivided the PT group into the PT1 (63%) and PT2 (37%) groups.
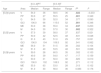
When we assessed the level of development in the PT and T groups, we found outcomes in the average range in all areas of development and at all time points (Table 2).
Areas of development in preterm and term groups at different ages.
| [0,3–4]PT | [0,5–6]T | ||||||
|---|---|---|---|---|---|---|---|
| Age | Area | Median | Range | Median | Range | Pa | rb |
| [5,0]4 years | V | 54.0 | 36 | 58.5 | 36 | .022 | −0.233 |
| PP | 50.0 | 27 | 55.5 | 25 | .001 | 0.349 | |
| Q | 54.0 | 39 | 52.0 | 34 | .377 | 0.090 | |
| GCI | 106.0 | 66 | 115.0 | 52 | .001 | 0.346 | |
| ME | 53.0 | 38 | 55.0 | 34 | .047 | 0.203 | |
| M | 54.0 | 30 | 57.0 | 30 | .002 | 0.322 | |
| [5,0]5 years | V | 57.0 | 39 | 58.0 | 37 | .837 | 0.021 |
| PP | 50.0 | 42 | 52.5 | 48 | .631 | 0.048 | |
| Q | 51.0 | 43 | 51.0 | 29 | .757 | 0.031 | |
| GCI | 106.0 | 104 | 109.5 | 92 | .541 | 0.062 | |
| ME | 56.0 | 51 | 51.5 | 38 | .302 | 0.104 | |
| M | 51.0 | 40 | 53.5 | 48 | .501 | 0.068 | |
| [5,0]6 years | V | 59.0 | 28 | 60.5 | 35 | .302 | 0.103 |
| PP | 49.0 | 39 | 54.0 | 47 | .117 | 0.159 | |
| Q | 50.0 | 31 | 50.0 | 30 | .925 | 0.010 | |
| GCI | 106.0 | 102 | 108.5 | 92 | .271 | 0.112 | |
| ME | 55.0 | 63 | 53.0 | 28 | .313 | 0.102 | |
| M | 51.0 | 33 | 56.0 | 36 | 0.083 | 0.176 | |
GCI, General Cognitive Index; M, Motor scale; ME, Memory scale; PP, Perceptual-Performance scale; PT, preterm group; Q, Quantitative scale; T, term group; V, Verbal scale.
Statistically significant results are presented in boldface.
When we compared the FT and T groups at different time points, we found lower scores in the PT group at age 4 years in all assessed areas save for numerical reasoning, and we found no differences at ages 5 and 6 years. We found a medium effect size in the Perceptual-Performance and Motor scales and the GCI (Table 2). The longitudinal intragroup comparisons revealed that verbal performance improved between ages 4 and 5 years in the PT group (r = 0.377; P = .008).
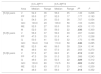
In the analysis based on the degree of prematurity, we found that scores in the PT1 and PT2 groups were within the normal range, although scores were higher in the PT2 group for every area of development at every time point (Table 3).
Areas of development in PT1 and PT2 groups at different ages.
| [0,3–4]PT1 | [0,5–6]PT2 | ||||||
|---|---|---|---|---|---|---|---|
| Area | Median | Range | Median | Range | Pa | rb | |
| [5,0]4 years | V | 54.0 | 36 | 56.0 | 35 | .149 | 0.206 |
| PP | 50.0 | 27 | 52.0 | 17 | .177 | 0.193 | |
| Q | 54.0 | 24 | 53.0 | 36 | .707 | 0.054 | |
| GCI | 103.0 | 49 | 109.0 | 58 | .103 | 0.233 | |
| ME | 52.0 | 27 | 53.0 | 30 | .429 | 0.113 | |
| M | 52.0 | 30 | 56.0 | 22 | .036 | 0.300 | |
| [5,0]5 years | V | 56.0 | 37 | 59.0 | 39 | .097 | 0.240 |
| PP | 47.0 | 33 | 51.5 | 41 | .071 | 0.258 | |
| Q | 50.0 | 41 | 52.0 | 32 | .170 | 0.196 | |
| GCI | 104.0 | 104 | 110.0 | 58 | .046 | 0.285 | |
| ME | 52.0 | 48 | 56.0 | 38 | .324 | 0.141 | |
| M | 49.0 | 40 | 57.0 | 25 | .059 | 0.270 | |
| [5,0]6 years | V | 57.0 | 27 | 62.0 | 21 | .012 | 0.361 |
| PP | 47.0 | 39 | 51.0 | 25 | .088 | 0.243 | |
| Q | 49.0 | 24 | 52.5 | 22 | .029 | 0.312 | |
| GCI | 103.0 | 80 | 112.5 | 53 | .002 | 0.452 | |
| ME | 52.0 | 63 | 57.0 | 33 | .143 | 0.209 | |
| M | 46.0 | 33 | 56.0 | 27 | .014 | 0.352 | |
GCI, General Cognitive Index; M, Motor scale; ME, Memory scale; PP, Perceptual-Performance scale; PT1, preterm 1 group (gestational age < 32 weeks); PT2, preterm 2 group (gestational age 32–37 weeks); Q, Quantitative scale; V, Verbal scale.
Statistically significant results are presented in boldface.
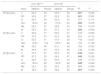
To determine the impact of the degree of prematurity in the subsequent development of the child, we performed Mann-Whitney U tests to compare 2 groups at a time (PT1 vs T, PT1 vs PT2 and PT2 vs T). We found significant differences between children born very/extremely preterm (PT1) and children born moderately/late preterm (PT2), with impairment increasing in severity with decreasing GA and increasing chronological age (Table 3). We also found significantly lower scores in the PT1 group compared to the T group in the Verbal, Perceptual-Performance and Motor scales and the GCI at ages 4 and 6 years (Table 4). In contrast, we did not find statistically significant differences between the PT2 group and the T group. The effect size in all the aforementioned associations was medium, except for the GCI at 5 years in the comparison of the PT1 and PT2 groups, with a small effect size.
Areas of development in PT1 and T groups at different ages.
| [0,3–4]PT1 | [0,5–6]T | ||||||
|---|---|---|---|---|---|---|---|
| Area | Median | Range | Median | Range | Pa | rb | |
| [5,0]4 years | V | 54.0 | 36 | 58.5 | 36 | .007 | 0.306 |
| PP | 50.0 | 27 | 55.5 | 25 | .001 | 0.393 | |
| Q | 54.0 | 24 | 52.0 | 34 | .327 | 0.111 | |
| GCI | 103.0 | 49 | 115.0 | 52 | .000 | 0.418 | |
| ME | 52.0 | 27 | 55.0 | 34 | .056 | 0.216 | |
| M | 52.0 | 30 | 57.0 | 30 | .000 | 0.400 | |
| [5,0]5 years | V | 56.0 | 37 | 58.0 | 37 | .376 | 0.099 |
| PP | 47.0 | 33 | 52.5 | 48 | .304 | 0.115 | |
| Q | 50.0 | 41 | 51.0 | 29 | .744 | 0.037 | |
| GCI | 104.0 | 104 | 109.5 | 92 | .155 | 0.159 | |
| ME | 52.0 | 48 | 51.5 | 38 | .729 | 0.039 | |
| M | 49.0 | 40 | 53.5 | 48 | .138 | 0.166 | |
| [5,0]6 years | V | 57.0 | 27 | 60.5 | 35 | .049 | 0.221 |
| PP | 47.0 | 39 | 54.0 | 47 | .045 | 0.226 | |
| Q | 49.0 | 24 | 50.0 | 30 | .326 | 0.110 | |
| GCI | 103.0 | 80 | 108.5 | 92 | .028 | 0.248 | |
| ME | 52.0 | 63 | 53.0 | 28 | .960 | 0.006 | |
| M | 46.0 | 33 | 56.0 | 36 | .007 | 0.302 | |
GCI, General Cognitive Index; M, Motor scale; ME, Memory scale; PP, Perceptual-Performance scale; PT1, preterm 1 group (gestational age < 32 weeks); Q, Quantitative scale; T, term group; V, Verbal scale.
Last of all, the longitudinal intragroup analysis revealed significant differences in the PT1 group in the Verbal scale (r = 0.459; P = .011) and the Perceptual-Performance scale (r = 0.389; P = .030) between ages 4 and 5 years, with a medium size effect in both cases. When it came to the Verbal scale, the scores improved at age 5 years, whereas scores for the Perceptual-Performance scale exhibited the opposite trend. There were no relevant findings in other areas of development, save for a decreasing trend in the scores of the PT1 group at age 6 years. We did not detect any intragroup differences in the PT2 group.
DiscussionSome studies present evidence that children with a history of preterm birth may experience developmental problems.13,15 The findings of our study are partially consistent with the previous evidence, as preterm children obtained scores in the middle range. However, on comparing them to their peers we found significant differences that were more apparent the lower the gestational age. We found the greatest differences between children born preterm and their full-term peers at age 4 years.
When it came to language developments, our findings supported those of Ment et al.,21 who reported that the differences between children born preterm and at term at age 4 years were not maintained in time.
As for motor skills, our findings were partly consistent with those of other studies,20,26,29 as we detected differences between children born preterm and children born at term, although only at age 4 years. It is possible that mild impairments in motor skills27 or visual perception29 found at similar ages are related to the differences found in the perceptual motor skills area.
Our analysis of memory only revealed differences at age 4 years, but it is only from age 6 years that memory function is essential for more demanding learning. Thus, these children may experience greater challenges at later ages.28,30 These data support the need of evaluation including specific testing of memory starting from age 6 years.
In children born before 32 weeks GA, the level of development was lower compared to children born at term, but we found no differences in development between moderate or late preterm children and term children. These outcomes are consistent with the findings of other studies carried out in children in the same stage of development,9,14 which have evinced cognitive and neurodevelopmental impairments of increasing degree the greater the prematurity.11,12 In other words, a very preterm birth is associated with poorer cognitive and motor skills in early childhood, impairments that are not as evident in moderate or late preterm children.16,17 Based on these data, children born very preterm are likely to need additional support once they start their primary education, as they exhibit significantly lower skills at this age in most of the evaluated areas of development.
In the analysis of different areas of development, the language outcomes corroborated the findings of Rodríguez et al22 and Sánchez-Joya et al.,14 who found poorer outcomes in preterm children, or those of Aarnoudse-Moens et al.,23 who observed impaired verbal fluency in these children compared to their term counterparts. We also found similarities between our findings and those of other authors in regard to motor skills development.10,27
We ought to highlight the very small number of studies in very preterm children analysing memory and mathematical skills. Thus, the differences found in our study, which were considerable in the memory domain at both ages 4 and 6 years, ought to be taken into account, as they could affect future performance. In regard to mathematical skills, differences have been found between children born very preterm and children born at term,29 and visual perception could be a factor contributing to this impaired performance during the school years.28 In this instance, we also identified difficulties with numerical reasoning in relation to GA.
The intragroup analysis did not yield conclusive results. Nevertheless, we did observe that scores declined with increasing age and level of difficulty of tasks in the very preterm group. In opposition, we found that in moderate and late preterm children, scores tended to improve, eventually reaching the level of term children.
At the beginning of the study, we aimed to assess the impact of preterm birth throughout the preschool years, which is a strength given the few opportunities that arise to study this entire period. We may conclude that psychomotor development in children born preterm is influenced by GA at birth. Thus, studies that do not take this variable in to account may not provide an accurate representation of functioning in children born preterm during this stage of development. Analysing outcomes based on the degree of prematurity may yield more accurate information on the pattern of psychomotor development. Thus, at age 6 years children born very or extremely preterm perform poorly compared not only to term children but also to moderate or late PT children. These outcomes may have an impact when children start primary school and academic demands increase, and those with the highest degree of prematurity may experience greater difficulties. For these reasons, we consider that the health care follow-up of this population should extend beyond age 6 years, when children enter a key stage in skill development and learning that may impact future academic performance.
Last of all, we ought to highlight some of the limitations of our study, such as the reduced number of cases in each group once we divided the preterm group into categories based on GA. In future studies, it would be convenient to have a larger initial sample to ensure maintenance of adequate statistical power despite losses to follow-up. It would also be important to take into account the impact of other medical and/or sociodemographic variables, make a thorough analysis of the different scales in the MSCA, complete the psychometric assessment with more specific tests for each area of development, particularly language, memory and executive functioning, and use neuroimaging tests, which could provide more detailed conclusions on the neurologic functions that are most affected.
FundingDepartment of Health. Government of Andalusia. Project code: PI-0397/2007. Government of Andalusia. Code: 1999/07.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank all the children born preterm and at term that participated in this study and their families. We also thank our families, our children, and everyone that has made this study possible.
Please cite this article as: Pereira-Cerro AV, Lanzarote-Fernández MD, Barbancho-Morant MM, Padilla-Muñoz EM. Evolución del desarrollo psicomotor en preescolares con antecedentes de prematuridad. An Pediatr (Barc). 2020;93:228–235.