Suicide attempt in adolescents is a major global health problem. In order to prevent them, the risk factors need to be identified. The present study evaluates the clinical and epidemiological aspects of adolescent patients after attempted suicide, who were seen in an emergency department.
Materials and methodsDescription of retrospective study of patients younger than 18 years who visited emergency department unit after a suicide attempt, during the period from 2008 to 2012.
ResultsA total of 241 patients were included, of whom 203 were female. The median age of the patients was 15.6 years. Psiquiatric history was present in 65.1% of the patients. The most frequent suicide mechanism was drug overdose (94.2%). Attempted suicide ideation was more common in males and in patients with previous attempts, and were also more related to sequels. Moreover, patients with an overdose were associated with psychiatric history and clinical toxicity.
ConclusionsPatients with any of the following characteristics; male, psychiatric history, a history of previous suicide attempts and/or clinical toxicity at the time of the visit in the emergency centre, were more associated suicidal ideation before the attempt. Therefore, they had greater severity and risk repeating the attempt. They require a careful psychiatric evaluation and close monitoring.
La tentativa de suicidio en adolescentes es un grave problema de salud a nivel mundial. Para desarrollar medidas preventivas es necesario identificar factores de riesgo. El objetivo del estudio es describir y analizar las características epidemiológicas y clínicas de los pacientes que acuden al Servicio de Urgencias Pediátrico (SUP) tras presentar una tentativa de suicidio.
Materiales y métodosEstudio retrospectivo de los pacientes menores de 18 años visitados en un SUP tras tentativa de suicidio entre 2008 y 2012.
ResultadosSe obtuvo una muestra de 241 pacientes, 84,2% mujeres, con una mediana de edad de 15,6 años. El 65,1% de los pacientes presentaba antecedentes psiquiátricos, siendo el más frecuente el trastorno depresivo (61 pacientes). El mecanismo suicida más frecuente fue la intoxicación medicamentosa con 94,2% de los casos.
La presencia de ideación suicida estable previamente a la tentativa fue más frecuente en los varones y en pacientes con tentativas previas, y se relacionó con la aparición de secuelas en mayor proporción. Además, en los pacientes con intoxicación se relacionó también con presentar antecedentes psiquiátricos y con la aparición de clínica de toxicidad.
ConclusionesLos pacientes varones, con antecedentes psiquiátricos, con antecedentes de tentativas suicidas previas y/o con clínica de toxicidad en el momento de atención en el SUP presentan con más frecuencia ideación suicida estable previa a la realización de la tentativa y, por tanto, mayor gravedad y riesgo de repetirla. Requieren, por tanto, una valoración psiquiátrica cuidadosa y un seguimiento estrecho.
The incidence of attempted suicide in adolescents is difficult to determine. According to the Instituto Nacional de Estadística (National Institute of Statistics), the rate of suicide in youth (15–19 years) in 2012 was 2.38 per 100,000 inhabitants.1 It is estimated that for every completed suicide, there are between 10 and 40 suicide attempts.2 Suicide attempts in youth are associated with impulsivity, the pessimistic perspective of introverted adolescents, the onset of psychiatric disorders and the start of substance use.3,4 The most frequent method used for attempting suicide in Spain is medication overdose, and differs from other types of paediatric pharmaceutical poisoning in the longer time elapsed until medical care is sought, a higher proportion of combined drug intoxication, and the clinical manifestations.4 The management of these patients in Paediatric Emergency Departments (PEDs) must be interdisciplinary and include a thorough psychiatric evaluation. This evaluation will assess the current risk of suicide, the presence of psychiatric comorbidities, and the type of treatment and followup that patients will require after emergency care. The aim of our study was to describe the epidemiological and clinical characteristics of suicide attempts and to differentiate patients that attempted suicide on impulse from those in whom suicidal ideation preceded the attempt. We also analysed patients that attempted suicide by self-poisoning.
Materials and methodsWe conducted a retrospective analytical and observational study in the PED of a tertiary women's and children's hospital that serves a population of 1,300,000 inhabitants and receives 100,000 paediatric visits per year. A psychiatrist is available around the clock to see patients that have been referred specifically for psychiatric assessment. The study included adolescents (12–18 years) that attempted suicide between 2008 and 2012. We collected data for the following variables: age, sex, previous psychiatric history, previous attempts, suicide method, referral for psychiatric assessment, sustained suicidal ideation prior to the attempt, and outcome of the attempt. For patients with poisoning that received care at the PED (excluding those referred for psychiatric assessment), we also collected data pertaining to: ambulance transport, time elapsed between exposure to the toxic substance and PED care, presenting symptoms, management of the poisoning and need for admission. We analysed whether there were clinical or epidemiological differences between patients that attempted suicide on impulse and patients that had prior sustained suicidal ideation. We assessed the impulsivity of the attempt based on the judgement of the psychiatrist that provided emergency care. The study was approved by the research ethics committee of the hospital. We performed the statistical analysis with the application SPSS v 20.0 for Windows (IBM Corporation; Armonk, USA).
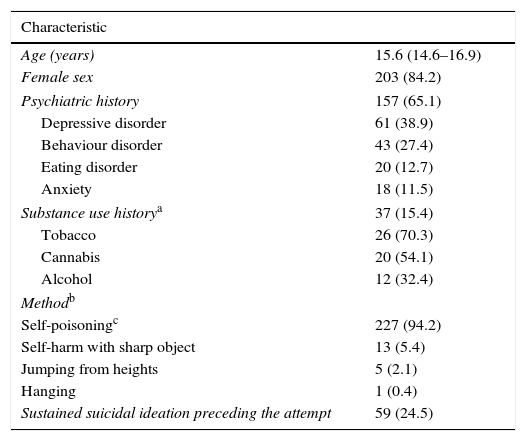
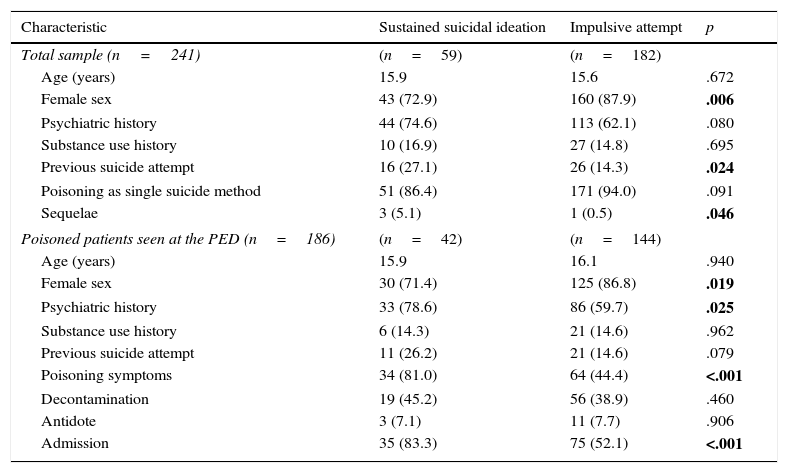
ResultsWe included 241 patients that attempted suicide. The yearly rate of suicide attempts per 1000 adolescents served in the emergency department was 4.2‰ (IQR, 3.7–4.8‰). Table 1 shows the epidemiologic characteristics of the patients. Forty-two patients (17.4%) had attempted suicide before. The time elapsed between the last prior attempt and the attempt analysed in the study was documented for 25 patients (59.5%), and was less than one year in 19 patients (76%). Forty-four patients (18.3%) were referred from other health care facilities. The most frequently used suicide method was poisoning (227; 94.2% of cases), mostly with pharmaceutical agents (215; 94.7%). The predominant drug class was psychotropic drugs (involved in 72.1% of intentional medication overdoses): benzodiazepines (81; 37.7%), antidepressants (34; 15.8%) and antipsychotics (20; 9.3%). The second most commonly involved drug class was analgesics (68; 31.6%), most often paracetamol (35; 16.3%). Of all cases, 33.6% (72) corresponded to combined drug intoxication. All patients survived, four of them (1.7%) with sequelae: three had multiple lesions due to jumping from heights and one had caustic oesophagitis. Of the 227 patients that attempted suicide by self-poisoning, 186 (81.9%) went directly to the PED (Table 1). The time elapsed between exposure to the toxic substance and the PED visit, documented in 137 of the patients (73.7%), was 3h (IQR, 2–7h). Digestive tract decontamination was performed in 75 patients (33%), and in 35.5% (27) of these patients, decontamination included gastric lavage. Of the 110 patients admitted to hospital, 7 (6.4%) were admitted to the Intensive Care Unit. The psychiatric evaluation determined that 24.5% (59) of the patients had sustained suicidal ideation prior to the attempt. When we compared this group to the group of patients that attempted suicide on impulse, we observed that suicidal ideation was more common in males and in patients that had made previous attempts, and was associated with a higher incidence of sequelae. In the subset of patients that attempted suicide by poisoning, sustained suicidal ideation was more frequent in patients that were male, had a history of psychiatric illness, presented with clinical manifestations of poisoning and required admission. Table 2 shows the association between the clinical and epidemiological characteristics of the patients and the presence of suicidal ideation prior to the attempt.
Epidemiological characteristics of patients that attempted suicide (n=241).
| Characteristic | |
|---|---|
| Age (years) | 15.6 (14.6–16.9) |
| Female sex | 203 (84.2) |
| Psychiatric history | 157 (65.1) |
| Depressive disorder | 61 (38.9) |
| Behaviour disorder | 43 (27.4) |
| Eating disorder | 20 (12.7) |
| Anxiety | 18 (11.5) |
| Substance use historya | 37 (15.4) |
| Tobacco | 26 (70.3) |
| Cannabis | 20 (54.1) |
| Alcohol | 12 (32.4) |
| Methodb | |
| Self-poisoningc | 227 (94.2) |
| Self-harm with sharp object | 13 (5.4) |
| Jumping from heights | 5 (2.1) |
| Hanging | 1 (0.4) |
| Sustained suicidal ideation preceding the attempt | 59 (24.5) |
| Characteristics of patients that received care for poisoning at the PED (n=186) | |
|---|---|
| Age in years and female sex | 16.0 (14.7–17.0); 155 (83.3) |
| Psychiatric history | 119 (64.0) |
| Ambulance transport | 113 (60.8) |
| Number of toxic substances involved | |
| 1 | 117 (62.9) |
| 2 | 44 (23.7) |
| ≥3 | 25 (13.4) |
| Poisoning with prescribed medications | 50 (26.9) |
| Presenting symptomsd | 98 (52.7) |
| Neurologic | 76 (77.6) |
| Psychiatric | 28 (28.6) |
| Digestive | 24 (24.5) |
| Poisoning management | |
| Decontamination | 75 (40.3) |
| Activated charcoal | 69 (92.0) |
| Gastric lavage | 26 (34.7) |
| Antidote | 14 (7.5) |
| Discharge destination | |
| Admission to hospital | 110 (59.1) |
| Psychiatric outpatient clinic/CSMIJ | 76 (40.9) |
Categorical variables are expressed as absolute frequency and percentage, continuous variables as median and interquartile range.
CSMIJ, Centro Salud Mental Infanto-Juvenil (Child and Adolescent Mental Health Centre).
Association between the presence of sustained suicidal ideation and clinical and epidemiological characteristics of the patients.
| Characteristic | Sustained suicidal ideation | Impulsive attempt | p |
|---|---|---|---|
| Total sample (n=241) | (n=59) | (n=182) | |
| Age (years) | 15.9 | 15.6 | .672 |
| Female sex | 43 (72.9) | 160 (87.9) | .006 |
| Psychiatric history | 44 (74.6) | 113 (62.1) | .080 |
| Substance use history | 10 (16.9) | 27 (14.8) | .695 |
| Previous suicide attempt | 16 (27.1) | 26 (14.3) | .024 |
| Poisoning as single suicide method | 51 (86.4) | 171 (94.0) | .091 |
| Sequelae | 3 (5.1) | 1 (0.5) | .046 |
| Poisoned patients seen at the PED (n=186) | (n=42) | (n=144) | |
| Age (years) | 15.9 | 16.1 | .940 |
| Female sex | 30 (71.4) | 125 (86.8) | .019 |
| Psychiatric history | 33 (78.6) | 86 (59.7) | .025 |
| Substance use history | 6 (14.3) | 21 (14.6) | .962 |
| Previous suicide attempt | 11 (26.2) | 21 (14.6) | .079 |
| Poisoning symptoms | 34 (81.0) | 64 (44.4) | <.001 |
| Decontamination | 19 (45.2) | 56 (38.9) | .460 |
| Antidote | 3 (7.1) | 11 (7.7) | .906 |
| Admission | 35 (83.3) | 75 (52.1) | <.001 |
Categorical variables are expressed as absolute frequency and percentage, continuous variables as median.
Data were considered statistically significant for p-values less than 0.05 (presented in boldface).
This study shows that suicide attempts among adolescents are more frequent in female individuals and are most commonly an impulsive act. Consistent with our findings, there is evidence that up to 90% of patients that attempt suicide have a psychiatric disorder, most frequently major depression.2 Between 20% and 47% of adolescent psychiatric patients have attempted suicide by age 18 years.5 A family history of suicide6 and having attempted suicide before7 are other known risk factors. In adolescents, the recurrent suicide attempt rate in the first year of followup ranges between 6% and 14%.7 In our study, 7.9% of patients reported having attempted suicide at least once before in the preceding year. The method used most frequently in Spain is intentional medication overdose and, consistent with previous studies,7 benzodiazepines were the most commonly involved drug. In case series in the United Kingdom, paracetamol is the most frequently ingested substance,8 and in countries where there is access to firearms, they are the most common method.9 Availability is a significant factor in the choice of method; and in this regard, we ought to note the widespread availability, based on our data, of psychopharmaceuticals in the Spanish population. In the subset of patients that attempted suicide by self-poisoning, a high percentage underwent digestive decontamination despite the long time elapsed since ingestion of the substance. The percentage that underwent gastric lavage was also considerable (35.5%) and far above the standard proposed by quality indicators for paediatric poisoning cases (<10%).10 The complexity of the situation may motivate a more aggressive management that is not always justified. Our study showed that sustained suicidal ideation was more frequent in patients that were male, had a psychiatric illness and/or had previously attempted suicide. The literature has described that male attempters complete suicide more frequently and using more violent means, and are more likely to have antisocial and substance use disorders.6 Patients with sustained suicidal ideation prior to the attempt presented with clinical manifestations of poisoning more frequently, which suggests that they may achieve more severe levels of intoxication than patients who attempt suicide on impulse.
The limitations of the study are those characteristic of a retrospective design. Due to the absence of objective indicators for measuring the impulsivity of the attempt and the duration of suicidal ideation prior to the attempt, we estimated these variables based on the subjective criteria of the psychiatrist on call, and thus our results must be interpreted with caution. Since we did not have access to clinical toxicological data on patients that received care at other facilities and were referred solely for psychiatric evaluation, we were not able to analyse the entire subset of patients that had attempted suicide by self-poisoning. Our study showed that patients that are male, have a history of psychiatric illness, have made a previous attempt and/or present with symptoms of poisoning in the emergency room are more likely to have had sustained suicidal ideation before the attempt and are at higher risk of attempting suicide again. These patients require thorough psychiatric evaluation and close monitoring.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Margarit Soler A, Martínez Sanchez L, Martínez Monseny A, Trenchs Sainz de la Maza V, Picouto González MD, Villar Cabeza F, et al. Características epidemiológicas de las tentativas de suicidio en adolescentes atendidos en Urgencias. An Pediatr (Barc). 2016;85:13–17.
Previous presentation: This study was presented at the XVIII Reunión Anual de la Sociedad Española de Urgencias de Pediatría; 2003; Granada, Spain.