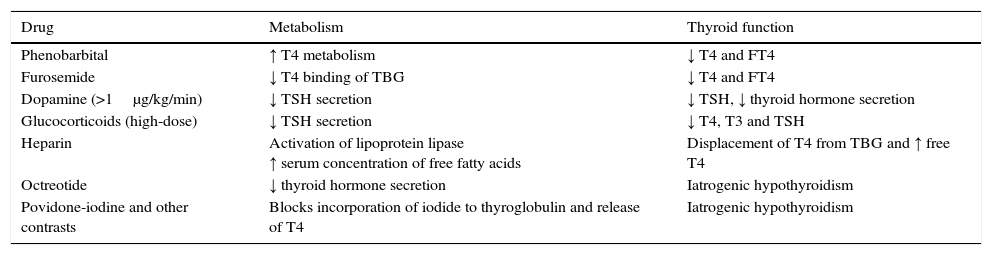
In the presence of elevated serum levels of thyroid hormones combined with normal levels of thyroid stimulating hormone (TSH) in the absence of signs or symptoms compatible with hyperthyroidism, clinicians need to consider the possibility of an error or interference in the interpretation of laboratory test results.1 Thyroid test results may be altered by the presence of heterophile antibodies or rheumatoid factor, or from the use of various pharmaceuticals (Table 1).
Drugs that can alter thyroid function in euthyroid patients.
| Drug | Metabolism | Thyroid function |
|---|---|---|
| Phenobarbital | ↑ T4 metabolism | ↓ T4 and FT4 |
| Furosemide | ↓ T4 binding of TBG | ↓ T4 and FT4 |
| Dopamine (>1μg/kg/min) | ↓ TSH secretion | ↓ TSH, ↓ thyroid hormone secretion |
| Glucocorticoids (high-dose) | ↓ TSH secretion | ↓ T4, T3 and TSH |
| Heparin | Activation of lipoprotein lipase ↑ serum concentration of free fatty acids | Displacement of T4 from TBG and ↑ free T4 |
| Octreotide | ↓ thyroid hormone secretion | Iatrogenic hypothyroidism |
| Povidone-iodine and other contrasts | Blocks incorporation of iodide to thyroglobulin and release of T4 | Iatrogenic hypothyroidism |
We proceed to describe a case of artefactual alteration of thyroid hormone levels due to the administration of heparin. Subsequently, we will describe the underlying pharmacological mechanism.
Male infant aged 8 months with a history of early neonatal epileptic encephalopathy secondary to a mutation in the KCNQ2 potassium channel gene and severe psychomotor retardation admitted to the paediatric intensive care unit (PICU) due to irritability and suspected sepsis. The family history was unremarkable. The patient was currently being treated with phenytoin, carbamazepine, vigabatrin and ketogenic diet. Past thyroid function tests found levels of free thyroxine (fT4) and thyroid stimulating hormone (TSH) within normal ranges. During his stay in the PICU, he experienced multiple episodes of deep and superficial vein thrombosis in the superior vena cava region associated with the presence of a central venous catheter. After removal of the catheter, treatment was initiated with low-molecular weight heparin (1mg/kg every 12h).
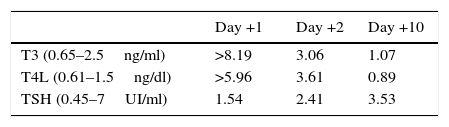
Twenty-four hours after the initial dose of heparin, routine tests showed overall fT4 and fT3 levels above those expected when the level of TSH is normal (Table 2). Since the patient exhibited no manifestations indicative of hyperthyroidism, this finding was attributed to the administration of heparin. For this reason, serial measurements of thyroid hormone levels were performed, which showed a gradual decrease with normalisation at day 10 despite the continued use of heparin. There were no changes in coagulation tests and the levels of anti-factor Xa (used to assess heparin activity against coagulation factor X) remained within the normal range. The patient did not have any more abnormal thyroid function test results.
Heparin, in both its fractionated and unfractionated forms, can interfere with the interpretation of thyroid function tests, producing an asymptomatic elevation of the free fraction of thyroid hormones.
Some authors have proposed mechanisms that could account for these findings.2 Although at present this is just speculation, the elevation may be due to a heparin-induced release of lipoprotein lipase from the vascular endothelium, which would result in an elevation in free fatty acids that would in turn inhibit the binding of thyroid hormones to their plasma transport proteins.
The potential interference of heparin with thyroid hormone levels has been described occasionally in adult patients.3 In 1996 Jain and Uy4 published the cases of four adult patients with asymptomatic elevation of thyroid hormones detected in samples collected 12h after heparin administration. A single patient underwent a subsequent thyroid function test, which showed that levels had normalised after discontinuation of heparin.
Only one case has been published in the paediatric literature.5 It concerned a preterm boy born at 35 weeks’ gestation admitted to the PICU due to thrombosis secondary to a peripheral venous access that was treated with heparin and exhibited an asymptomatic elevation of thyroid hormones that normalised after the treatment was discontinued.
In the case under study, the patient had an initial elevation of serum-free thyroid hormones that normalised spontaneously despite continuing treatment, something that has not been reported in the past. The interaction between the administration and dosage of heparin, the release of fatty acids and their association with thyroid hormone levels, of which we lack detailed knowledge, may account for the variability observed in patients and in a single patient at different times. On the other hand, phenytoin and carbamazepine may alter thyroid function, but the resulting changes would involve an asymptomatic decrease in serum-free levels of thyroid hormones rather than an elevation6 (Table 2) like the one observed in our patient.
In conclusion, we must remain aware of the potential of heparin to cause a spurious elevation in thyroid hormone levels in order to avoid unnecessary treatments or tests. Clinical observation, monitoring of laboratory test results and discontinuation of the involved drug, if necessary, should be the elements considered to guide the interpretation of this laboratory finding.
Please cite this article as: De Noriega Echevarría I, García-Salido A, Muñoz-Calvo MT, Argente J. Elevación de los niveles de hormonas tiroideas tras administración de heparina de bajo peso molecular. An Pediatr (Barc). 2017;87:50–51.