There are many initiatives aimed at eliminating health care interventions of limited utility in clinical practice. The Committee on Care Quality and Patient Safety of the Spanish Association of Pediatrics (AEP) has proposed the development of “DO NOT DO” recommendations (DNDRs) to establish a series of practices to be avoided in the care of paediatric patients in primary, emergency, inpatient and home-based care.
Material and methodsThe project was carried out in 2 phases: a first phase in which possible DNDRs were proposed, and a second in which the final recommendations were established by consensus using the Delphi method. Recommendations were proposed and evaluated by members of the professional groups and paediatrics societies invited to participate in the project under the coordination of members of the Committee on Care Quality and Patient Safety.
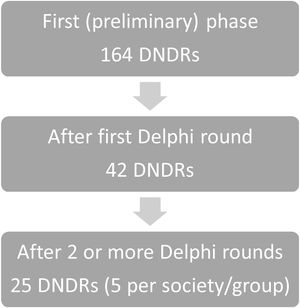
ResultsA total of 164 DNDRs were proposed by the Spanish Society of Neonatology, the Spanish Association of Primary Care Paediatrics, the Spanish Society of Paediatric Emergency Medicine, the Spanish Society of Internal Hospital Paediatrics and the Medicines Committee of the AEP and the Spanish Group of Paediatric Pharmacy of the Spanish Society of Hospital Pharmacy. The initial set was limited to 42 DNDRs, and the selection over successive rounds yielded a final set of 25 DNDRs, with 5 DNDRs for each paediatrics group or society.
ConclusionsThis project allowed the selection and establishment by consensus of a series of recommendations to avoid unsafe, inefficient or low-value practices in different areas of paediatric care, which may contribute to improving the safety and quality of paediatric clinical practice.
Muchas son las iniciativas encaminadas a eliminar intervenciones clínicas de poco valor en la asistencia sanitaria. Desde el Comité de Calidad Asistencial y Seguridad del Paciente de la AEP, se ha propuesto la elaboración de recomendaciones de “NO HACER” (RNH) con el objetivo de señalar una serie de prácticas a evitar en la atención del paciente pediátrico en atención primaria, urgencias, hospitalización y domicilio.
Material y métodosEste trabajo se desarrolló en dos fases: una primera en la que propusieron posibles RNH, y una segunda en la que se consensuaron las recomendaciones finales mediante método Delphi. Tanto las propuestas como las evaluaciones fueron realizadas por miembros de los grupos y sociedades pediátricas a los que se le realizó la propuesta, coordinados por miembros del Comité de Calidad Asistencial y Seguridad del paciente.
ResultadosFueron propuestas un total de 164 RNH por la Sociedad Española de Neonatología, la Asociación Española de Pediatría de Atención Primaria, la Sociedad Española de Urgencias de Pediatría, la Sociedad Española de Pediatría Interna Hospitalaria y el Comité de Medicamentos de la AEP con el Grupo Español de Farmacia Pediátrica de la Sociedad Española de Farmacia Hospitalaria. Se logró reducir el conjunto inicial a 42 RNH, y en sucesivas fases se llegó a la selección final de 25 RNH, 5 RNH por cada grupo o sociedad.
ConclusionesEste proyecto ha permitido seleccionar y consensuar una serie de recomendaciones para evitar prácticas inseguras, ineficientes o de escaso valor en distintos ámbitos de la atención pediátrica, lo que podría resultar útil para mejorar la seguridad y la calidad de nuestra actividad asistencial.
In recent years, there has been considerable concern regarding the overuse of health care interventions, which at times are implemented without sufficient evidence in support, can carry risks and result in an unwarranted increase in health care costs.1,2 Thus, it is estimated that between 20% and 30% of diagnostic tests and treatments in the United States are unnecessary, do not improve outcomes or cause harm to the patient,3 in addition to having an economic impact that amounts to more than 20% of the total health care expenditure.4
In light of this, different scientific societies and institutions, at both the national and international levels, have launched various strategies with the aim of reducing the use of unnecessary diagnostic procedures and treatments of little or dubious effectiveness, which are not cost-effective or that have iatrogenic effects.5
Among such strategies, we would like to highlight the Choosing wisely initiative in the United States, in which medical societies, including the American Academy of Pediatrics,6 identified the five services that they considered most important to avoid, with recommendations applicable to different fields of paediatrics.7,8 Similarly, the American Medical Association launched the Less is more campaign. At the same time, the National Institute for Health and Care Excellence (NICE) of the United Kingdom has been developing “do not do recommendations” (DNDRs),9 with more than 1500 issued to date. The European Academy of Paediatrics has also joined in these efforts10 and has issued lists of Choosing wisely recommendations for each paediatric speciality that can be consulted on its website.11
In this context, the Spanish Ministry of Health Care, Consumption and Social Welfare, on the initiative of the Sociedad Española de Medicina Interna (SEMI, Spanish Society of Internal Medicine), launched the Commitment to Quality of Scientific Societies in Spain project in 2013,12 similar to the Choosing wisely campaign of the United States, with the participation of numerous scientific societies, including the Asociación Española de Pediatría (AEP, Spanish Association of Pediatrics).13 The main objective of this project is to reduce the use of unnecessary health care services, understood as those of unproven efficacy, limited or dubious effectiveness, not cost-effective or not considered a priority.
Spanish paediatrics societies and their working groups have developed DNDRs addressing specific conditions (poisoning, infectious disease, etc),14,15 or care settings or delivery aspects,16,17 and have recently published DNDRs for the field of paediatric intensive care.18
Paediatric patients are more likely to experience adverse events and serious complications of these adverse events, which makes the implementation of strategies of this nature to improve patient safety in care delivery a pressing necessity. In consequence, the Committee on Care Quality and Patient Safety of AEP has proposed the development of DNDRs for different paediatric care settings. Several paediatric scientific societies contributed to the development of a series of DNDRs for paediatric care delivery in the primary care, emergency care, inpatient and home settings.
Material and methodsIn the initial phase of the study, a request for participation and a document explaining the objectives of the project, including examples of how to submit the necessary information, were submitted to representatives of the participating societies (Sociedad Española de Neonatología [SENeo, Spanish Society of Neonatology], Asociación Española de Pediatría de Atención Primaria [AEPap, Spanish Association of Primary Care Paediatrics], Sociedad Española de Urgencias de Pediatría [SEUP, Spanish Society of Paediatric Emergency Medicine], Sociedad Española de Pediatría Interna Hospitalaria [SEPIH, Spanish Society of Inpatient Paediatric Internal Medicine], Sociedad Española de Cuidados Intensivos Pediátricos [SECIP, Spanish Society of Intensive Paediatric Care], Comité de Medicamentos de la AEP [CM-AEP, Committee on Medicines of the AEP] and Grupo Español de Farmacia Pediátrica de la Sociedad Española de Farmacia Hospitalaria [GEFP-SEFH, Spanish Group of Paediatric Pharmacy of the Spanish Society of Hospital Pharmacy]. The document strongly recommended for each society to hold a brainstorming session to generate DNDRs and to select a final list prioritising frequent issues and taking into account the current scientific evidence. The project coordination group suggested that the recommendations focus, to the extent possible, on the dimensions of information/communication, safe patient transfer/safe medication, good practices and.
To unify the criteria, we asked the participating societies to choose the final list applying the Delphi method with the following directions: the expert panel members of each society were to rate all the DNDRs proposed in the initial brainstorming session on a Likert scale (from 1, completely disagree, to 9, completely agree). Proposals with a mean score of 8 or higher and given a rating of 7 or higher by at least two thirds of the participants would be selected. Proposals with a mean rating under 6 would be eliminated. Proposals for which the result was unclear were to be re-evaluated in a second round. After this structured selection process, each society had to submit a final list of 3–5 recommendations.
In the final phase, the group that coordinated compiled the final DNDR lists all the societies and reviewed the resulting set to ensure none were duplicated or overlapped. In the case that any were eliminated for that reason, that recommendation was replaced by the next most voted recommendation. In addition, the wording of the recommendations was revised to ensure consistency.
ResultsIn the first phase of the project, a total of 164 DNDRs were proposed by professionals of 5 paediatrics societies and groups: 12 by SENeo, 40 by AEPap, 65 by SEUP, 11 by the SEPIH, 36 by the CM-AEP and the GEFP-SEFH. Members of the SECIP did not actively participate in generating proposals, as they had already done so in a previous work completed in 2021.18
The distribution of proposed DNDRs by working group and society was very heterogeneous. After their evaluation, volunteers from the different groups and societies that had already participated in the first phase of the study reduced the initial set to 42 DNDRs in a first round, and after two or more rounds, to a final selection of 5 DNDRs per group or society (Diagram 1 and Table 1).
Number of DO NOT DO recommendations proposed by each paediatric society or working group in each phase.
| Paediatric society/group | Preliminary phase | After 1st Delphi round | After 2nd Delphi round |
|---|---|---|---|
| SENeo | 12 | 5 | – |
| AEPap | 40 | 7 | 5 |
| SEUP | 65 | 5 | – |
| SEPIH | 11 | 5 | – |
| CM-AEP and GEFP-SEFH | 36 | 20 | 12 |
AEPap, Asociación Española de Pediatría de Atención Primaria; CM-AEP, Committee on Medicines of the Asociación Española de Pediatría; GEFP-SEFH, Spanish Group on Paediatric Pharmacy of the Sociedad Española de Farmacia Hospitalaria; SENeo, Sociedad Española de Neonatología; SEPIH, Sociedad Española de Pediatría Interna Hospitalaria; SEUP, Sociedad Española de Urgencias de Pediatría.
Table 2 presents the final list of 5 DNDRs selected by each group or society after 2 or more Delphi rounds, and when 2 societies proposed the same recommendation, the duplicate was replaced by adding the next most voted recommendation to the list.
List of the five final DO NOT DO recommendations of each group or society.
| Paediatric society/group | DNDR statement | Rationale |
|---|---|---|
| SENeo | 1. DO NOT use invasive techniques in newborns without prior pain assessment and management with pharmacological and nonpharmacological methods. | Newborns experience pain, even the most premature ones. Current evidence-based knowledge demands a protocolised approach to pain management with routine pain assessment, reduction of the number of painful procedures and prevention of acute pain secondary to invasive procedures.21 |
| 2. DO NOT maintain empiric antibiotherapy without a clinical or microbiological justification. | The indiscriminate use of antibiotics for management of infections in newborns has resulted in an increase in antimicrobial resistance, which in turn has led to a higher rate of treatment failure with the use of empirical antibiotherapy.15,22 | |
| 3. DO NOT routinely change central line dressings every day. | Central line dressings should not be changed daily unless they are lose or dirty. Current recommendations call for changing gauze dressings every other day and transparent semipermeable dressings every 7 days, unless dirty or loose.23 | |
| 4. DO NOT separate the mother/infant dyad unless there is no other choice. | Current evidence suggests that skin-to-skin contact between mother and newborn within 24 h of birth has a beneficial effect on both.24 | |
| 5. DO NOT perform early cord clamping in term or late preterm newborns who do not require resuscitation. | Delayed cord clamping offers advantages, such as preventing neonatal anaemia, facilitating the transition from foetal to neonatal circulation, and decreasing the risk of late-onset sepsis, intraventricular haemorrhage and the need of transfusion.25 | |
| AEPap | 1. DO NOT eliminate gluten from the diet without justification. | A gluten-free diet should not be initiated before a diagnosis is made by a specialist, as it would interfere with the diagnosis.26 |
| 2. DO NOT provide antibiotherapy for pharyngitis without confirming a bacterial aetiology (by means of rapid antigen test or culture). | Most of these infections are caused by viruses. Antibiotics must not be made unless a streptococcal aetiology is confirmed.7,15 | |
| 3. DO NOT use drugs of low therapeutic value for treatment of acute rhinitis/pharyngitis (such as mucolytics, expectorants, antitussives, antihistamines decongestants, antibiotics or steroids). | Previous studies have shown that these drugs offer little benefit to children, while they may cause potentially severe adverse events. ) | |
| 4. DO NOT prescribe inhaled asthma medication without first educating the child and family on correct inhaler technique for age. | Educating patients and families is one of the cornerstones of asthma management. Any health care worker involved in the care of patients with asthma must engage in asthma education.27 | |
| 5. DO NOT delay administration of intramuscular adrenaline in case of anaphylaxis. | Adrenaline is a rapid-acting drug of demonstrated efficacy and very safe, so its administration should never be delayed when anaphylaxis is suspected.28 | |
| SEUP | 1. DO NOT start antibiotherapy in a patient with suspected urinary tract infection (UTI) without having first collected a sample for urine culture with sterile technique. | The diagnosis of UTI in paediatric patients always requires collection with sterile technique of a urine sample for culture before initiation of antibiotherapy to enable subsequent targeted therapy based on the results of antimicrobial susceptibility testing.15 |
| 2. DO NOT give antibiotics to a patient with uncomplicated respiratory infection (upper respiratory tract infection, laryngitis, bronchitis, bronchiolitis). | It is estimated that unnecessary antibiotherapy is prescribed in 50% of viral respiratory infections, which increases health care costs, the risk of adverse events and the emergence of antimicrobial resistance.7,15 | |
| 3. DO NOT delay initiation of empirical antibiotherapy to obtain samples for culture (blood and/or cerebrospinal fluid) in a patient with clinically suspected sepsis. | Sepsis is a time-dependent disease, and its outcomes depend on how early it is suspected and treatment initiated.17 | |
| 4. DO NOT fail to report any suspicion of mistreatment and/or abuse. | Child and sexual abuse do exist in our society. Health care professionals must report any suspected mistreatment and/or abuse.17 | |
| 5. DO NOT administer water, milk or inactivated charcoal following ingestion of household or industrial chemicals. In exceptional cases, after a careful evaluation, the recommendation not to use charcoal may be reconsidered. | The administration of any solid or liquid is generally contraindicated if the development of vomiting could increase the risk of aspiration (for instance, in the case of hydrocarbon ingestion) or in the case of potential gastrointestinal mucosal damage (ingestion of caustic substances).14 | |
| SEPIH | 1. DO NOT admit a patient to hospital without verifying the information on the ID bracelet, allergy history and treatment sheet. | It is estimated that communication errors are involved in 70% of serious medical errors, so having a standardised patient transfer protocol is essential.29 |
| 2. DO NOT use hypotonic fluids for maintenance fluid therapy. | Previous studies have concluded that, compared to hypotonic fluids, the use of isotonic fluids for maintenance fluid therapy decreases the risk of hyponatraemia without increasing the risk of complications such as hypernatremia, high blood pressure and/or oedema.30 | |
| 3. DO NOT administered medications that are not labelled correctly | Administration errors amount to 60% de of all medication errors. It is essential to implement protocols and strategies for the safe administration of medication.31 | |
| 4. DO NOT hide, cover up or punish hospital adverse events | A positive patient safety culture in health care institutions is a necessary condition to prevent and minimise incidents related to patient safety and to learn from errors to reduce the probability that they occur again.32 | |
| 5. DO NOT delegate any patient transfer to others without the presence of any of the care team members. | Transfer of care is a high-risk process that patients undergo numerous times in care delivery. Communication is a key element in this process and is involved in 70% of notified sentinel events.29 | |
| CM-AEP and GEFP-SEFH | 1. DO NOT keep medicines in plain sight and within reach of children or in any container other than the original packaging. | Each year, approximately 50 000 children aged less than 5 years present to the emergency department with drug poisoning. Medicines can produce severe adverse events, especially in children, so the prevention of drug poisoning is of the essence.33 |
| 2. DO NOT provide written information about medication to parents or caregivers without the pertinent verbal explanations and without verifying comprehension. | Lack of adequate information about medicines is a frequent cause of notified errors in paediatric patients. Therefore, it is very important for health care professionals to provide clear information to the parents or caregivers, explaining how devices must be used to deliver correct doses and verifying that they have understood the dose that needs to be administered.34 | |
| 3. DO NOT prescribe doses by the spoonful or exclusively in mL without using units of mass (eg mg) or concentration or specifying a particular formulation. | Paediatric patients are at higher risk of experiencing medication errors compared to adults, and of these errors being more serious. Most of these errors occur during prescribing and administration, and the problem is usually a dose error.34 | |
| 4. DO NOT prescribe without checking the current weight of the patient, allergies, contraindications and potential interactions. | Prescription errors are frequent in paediatric care, especially dosing errors. The prescription must include all necessary data for safe use: identification, clinical information (diagnosis, allergies, special conditions, etc), anthropometric values (weight, height, etc) and medication details, including the drug name, dose, route of administration, prescription date and administration order.34 | |
| 5. DO NOT store high-risk medication without distinctive identification with other medication in the medicine cabinets of health care facilities | The risk of medication errors causing adverse events in children is up to 3-fold that in adults, so it is essential to establish practices to prevent adverse events associated with high-risk medicines.35 | |
| SECIP18 | 1. DO NOT delay initiation of enteral nutrition unless it is contraindicated. | Previous studies support the recommendation of enteral nutrition as the preferred method for nutritional support in critically ill paediatric patients, demonstrating its feasibility and safety. Therefore, any interruptions or delays in enteral nutrition should be minimised to achieve minimum in an effort to achieve nutrient delivery goals by the enteral route.36 |
| 2. DO NOT prolong antibiotherapy beyond the recommended duration. | Some studies (such as the PISA study) found that the duration of antibiotherapy was inadequate in most cases.37 The efficacy of antibiotherapy tends to accumulate on the first days of treatment and does not improve with its prolongation. In addition, selective pressure and the selection of drug-resistant microbes increases with the duration of treatment.15 | |
| 3. DO NOT discharge without medical supervision any patient that has received procedural sedation before the patient is back to the baseline condition. | Certain drugs may interfere with the recovery of the baseline level of consciousness and require additional observation of the patient. This is particularly important in infants and toddlers transported in strollers or safety seats, in whom resedation leading to airway obstruction has been described in the past.38 | |
| 4. DO NOT put off placement of an intraosseous vascular catheter in patients in cardiac arrest or at imminent risk of cardiac arrest to insert a central venous catheter. | Intraosseous access is very useful in emergencies, when intravenous access is difficult, and it is quicker to establish than central access, so time should not be wasted on inserting a central line with ultrasound guidance.39 | |
| 5. DO NOT transport paediatric patients before they are stabilised under the best possible conditions at the emitting hospital. | Transport will not take place until the best possible clinical conditions have been established for the child. There is evidence that initiating transport without adequate stabilization beforehand has an important impact on morbidity and mortality.40 |
AEPap, Asociación Española de Pediatría de Atención Primaria; CM-AEP, Committee on Medicines of the Asociación Española de Pediatría; GEFP-SEFH, Spanish Group on Paediatric Pharmacy of the Sociedad Española de Farmacia Hospitalaria; SECIP, Sociedad Española de Cuidados Intensivos Pediátricos; SENeo, Sociedad Española de Neonatología; SEPIH, Sociedad Española de Pediatría Interna Hospitalaria; SEUP, Sociedad Española de Urgencias de Pediatría.
The definitive list of do not do recommendations address dimensions of care quality and patient safety such as information and communication, safe patient transfer, safe use of medication, good practices and prevention (Fig. 1).
Discussion and conclusionIn this project, we were able to produce a set of recommendations regarding practices to be avoided in different paediatric care settings in Spain. In this task, we counted on the collaboration of different scientific societies and working groups in the field of paediatrics dedicated to improve the quality of paediatric care, with participation of several professionals in paediatric medicine, nursing and pharmacy. To pursue this objective, like other scientific societies in the past,18 we used the Delphi methodology to establish the general opinion of a group of experts through a consensus process. This methodological approach allowed us to gain consensus-based recommendations with participation of a large number of professionals on the most important practices to eliminate in each care setting within a reasonable timeframe.
The identification of unnecessary practices, understood as those of unproven efficacy, limited or questionable effectiveness, that are not cost-effective or are not a priority, contributes to the improvement of care quality and the optimization of resources.19 We must promote quaternary prevention, that is, actions taken to prevent, reduce and/or ameliorate the harm caused by these unnecessary health care practices.20 Quaternary prevention has to do with the fact that it is easier to remedy what is left undone than what is done in excess, a social issue relevant to the entire population, especially given the current trend of increasing medicalization.
The implementation of safe practices in paediatric care is a necessity and one of the chief objectives of the Committee on Care Quality and Patient Safety of the AEP. Paediatric patients are at higher risk of health care-related adverse events and of these events, when they occur, having more severe complications. In consequence, identifying the most important practices to avoid in each paediatric care field is essential.
For each intervention that is to be delivered, we ought to consider different aspects: is it effective? is it safe? what is the risk-benefit balance? is it necessary? are there simpler alternatives? is it useful, will it have an impact on the patient? is it appropriate? will it improve the patient’s quality of life? is it reasonable? The identification and application of the DNDRs presented in this article could help improve the quality and safety of the care provided to paediatric patients in each of our clinical fields of practice.
Given all of the above, the publication and dissemination of these practices can contribute to improving the quality and safety of paediatric care in different settings (primary care, emergency care, inpatient care, neonatology, intensive care and home-based care) and reducing variability in clinical practice as well as the iatrogenic effects of unnecessary interventions.
The Committee on Care Quality and Patient Safety of the Asociación Española de Pediatría will continue to propose and develop initiatives in this area.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
SENeo: Roberto Ortiz Movilla, Mar Albújar Font, Elisabeth Gómez Santos, Beatriz Vacas del Arco, Tamara Carrizosa Molina, Marta Nicolás López, Felipe Verjano Sánchez, Adoración Vega Gil, Ana Filgueira Posse, Isabel de las Cuevas, Raquel Pinillos Pisón, Montserrat Sánchez Rubio, Elena Varela Rubio, Caridad Tapia Collados, Alicia Llorca Porcar, members of the SEGURNEO group.
AEPap:
Working groups: Cooperation, immigration and adoption, Health Education and Outreach, Familia y Salud, Pediatría Basada en la Evidencia, Previnfad, ADHD and Psychoeducational development, Airway, Infectious Disease, European Relations, PAPenRED, Gastronutri, FAPAP.
Affiliated regional associations: Andalusia, Aragon, Canary Islands; Castilla y Leon, Madrid, Murcia.
José Mengual Gil, José Miguel Ángel Fernández-Cuesta and Juana María Ledesma Albarrán.
SEUP: Carles Luaces Cubells, Francisco Javier Benito Fernández, Abel Martínez Mejías, Andrés González Hermosa, María Luisa Herreros Fernández, Silvia González Lago, Paula Vázquez López, Juan Luis Santos Pérez.
SEPIH: Pedro Alcalá Minagorre, Valeria Antoñanzas Bernar, Ángela Vidal Bataller. GT Calidad y Seguridad SEPIH. Jose David Martínez Pajares, Mariona Fernández de Sevilla, Ana Amat, Aroa Rodríguez, Ana Cordón, Nuria Gorina Ysern y Jimena Pérez. Executive board of the SEPIH.
Committee on Medicines of the AEP (CM-AEP): Cristina Calvo Rey, Ignacio Diez Lopez, Raquel Escrig Fernandez, María Angeles Gil Lemos, Daniel Lozano Martinez, Marcos Madruga Garrido, Santiago Manzano Blanco, Esmeralda Nuñez Cuadros, Roi Piñeiro Pérez, Belén Rodríguez Marrodan, Pedro Viaño Nogueira.
Spanish Group on Paediatric Pharmacy of the SEFH (GEFP-SEFH): María José Cabañas Poy, Concepción Álvarez del Vayo Benito, Carmen Gallego Fernandez, Beatriz Garrido Corro, Ana Alejandra García Robles, Yolanda Hernandez Gago, Ceclina Martinez Fernandez-Llamazares, Cristina Martinez Roca, María Teresa Pozas del Rio, Belén Rodriguez Marrodan, Miquel Villaronga Flaque, Daniel Fresán Restituto, Raquel Escrig Fernandez.
SECIP: María Teresa Alonso, Francisco José Cambra, Santiago Mencía, Raúl Borrego, José Luis de Unzueta, Alba Palacios, Alberto Salas, Julio Parrilla, Juan Carlos de Carlos, Sylvia Belda, Silvia Redondo, María José Solana, Rafael González, Mario Sánchez, Susana Reyes, Natalia Ramos, Artur Sharluyan, María Dolores Calvo, Reyes Fernández, José Luis López Prats.
Working Group on Safety of the SECIP.
Committee on Care Quality and Patient Safety: Marian Cuesta Rodríguez, Pilar Díaz Pernas, Victoria Díaz Marugán, Cristina Casado Reina, María José Salmerón Fernández.