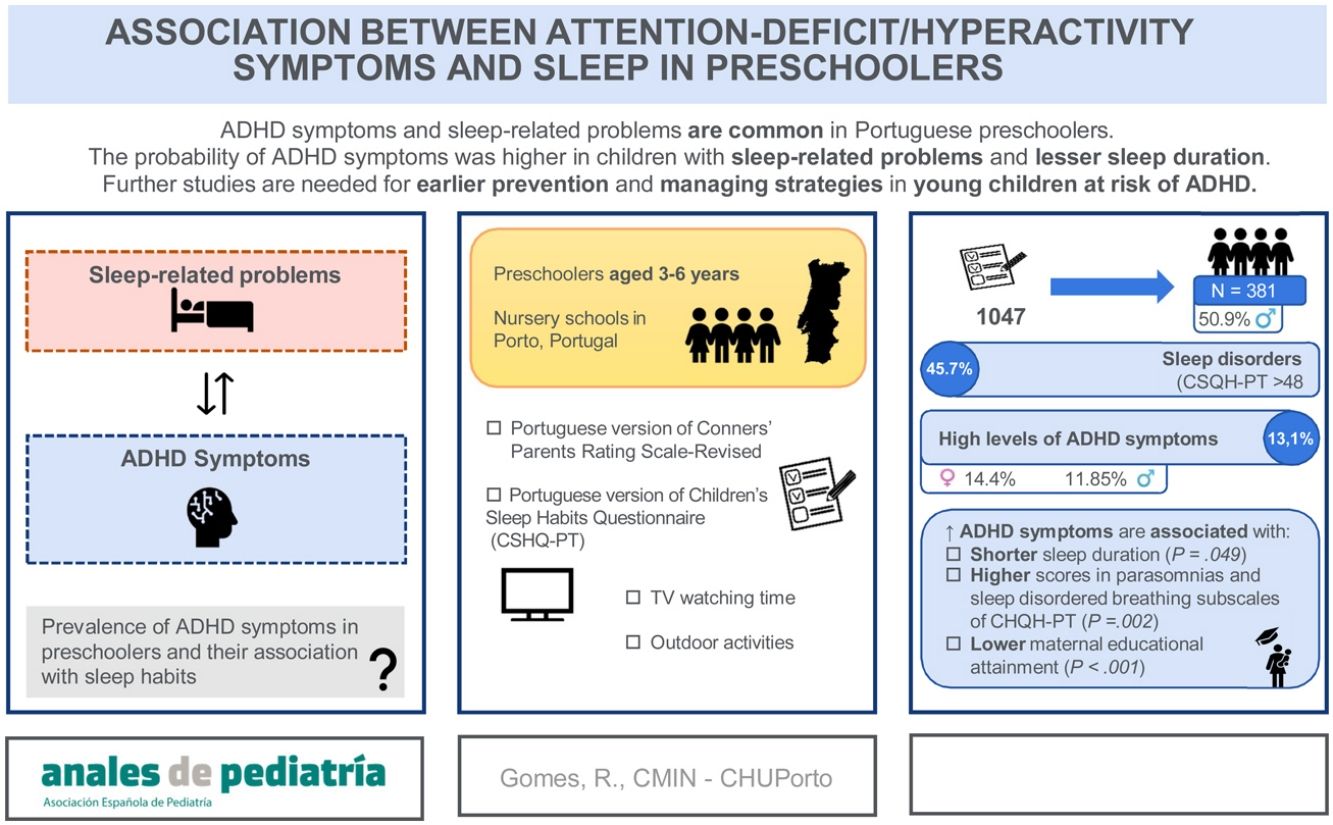
Sleep problems are frequent in children with attention-deficit/hyperactivity disorder (ADHD). Some authors have tried to characterize paediatric sleep habits in Portugal, but none has focused on preschool-age children nor attempted to establish their association with ADHD. We aimed to assess the prevalence of ADHD symptoms in preschool-age children and to study their association with sleep habits.
Material and methodsWe conducted a cross-sectional study. We distributed questionnaires to a random sample of caregivers of children enrolled in early childhood education centres in Porto. We collected data on sociodemographic characteristics, television watching and outdoor activities. We assessed ADHD symptoms and sleep habits with the Portuguese versions of the Conners’ Parents Rating Scale, Revised and the Children’s Sleep Habits Questionnaire (CSHQ-PT), respectively.
ResultsThe study included 381 preschoolers (50.90% male). We found high scores for ADHD symptoms in 13.10%, with a higher prevalence in girls (14.40% vs. 11.85%; P = 0.276). In the CSHQ-PT, 45.70% of participants had a mean total score greater than 48, which is the cut-off point applied in the screening of sleep disturbances in the Portuguese population. There was a significant association between high scores for ADHD symptoms and a lower maternal education level (P < 0.001), a shorter sleep duration (P = 0.049), and higher scores on parasomnias (P = 0.019) and sleep disordered breathing (P = 0.002) in CSHQ-PT subscales.
ConclusionsADHD and sleep disorders are common in preschoolers, in Porto, and this study suggests some clinical correlations between them. Since these interactions are complex and far from being elucidated, further studies are paramount to provide guidance for prevention and managing strategies in younger children at risk for ADHD.
Los problemas de sueño son frecuentes en niños con trastorno por déficit de atención/hiperactividad (TDAH). Algunos autores han tratado de caracterizar los hábitos de sueño pediátricos en Portugal, pero ninguno se ha centrado en los niños en edad preescolar ni ha intentado correlacionarlos con el TDAH. El objetivo fue evaluar la prevalencia de los síntomas del TDAH en niños en edad preescolar y estudiar su asociación con los hábitos de sueño.
Material y métodosEstudio transversal mediante la administración de un cuestionario a una muestra aleatoria de cuidadores de niños matriculados en guarderías en Oporto. Se recogieron datos de características sociodemográficas, consumo de televisión y actividades al aire libre. Los síntomas del TDAH y los hábitos de sueño fueron evaluados mediante las versiones portuguesas del Conners’ Parents Rating Scale-Revised y el Children’s Sleep Habits Questionnaire (CSHQ-PT), respectivamente.
ResultadosEl estudio incluyó 381 preescolares (50,90% varones). Se encontraron niveles altos de síntomas de TDAH en el 13,10%, con una prevalencia mayor en las niñas (14,40% vs. 11,85%; p = 0,276). El 45,70% tenían una puntuación total en el CSQH-PT superior a 48, que es el punto de corte establecido para el cribado de los trastornos del sueño en la población portuguesa. Se encontró una asociación significativa entre niveles altos de síntomas de TDAH y un nivel educativo materno más bajo (p < 0,001), una menor duración del sueño (p = 0,049) y mayores puntuaciones en las subescalas de parasomnias (p = 0,019) y de trastornos respiratorios del sueño (p = 0,002).
ConclusionesEl TDAH y los problemas de sueño son comunes en los preescolares de Oporto, y el presente estudio sugiere algunas correlaciones clínicas entre ambos. Dado que estas interacciones son complejas y están lejos de ser dilucidadas, es fundamental realizar más estudios para orientar las estrategias de prevención y de intervención temprana en los niños más pequeños con riesgo de TDAH.
Attention-deficit/hyperactivity disorder (ADHD) is the most common neurodevelopmental disorder of childhood and a rising public health concern.1,2 According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), it is defined by age-inappropriate symptoms of inattention and/or hyperactivity and impulsivity starting before the age of 12, which are present in more than one setting and interfere with academic or social functioning.3
Although ADHD is typically diagnosed during the school years, there is an increasing recognition that symptoms might manifest in preschoolers and persist through primary school and into adulthood.1 Therefore, the identification of factors contributing to ADHD in early childhood is essential to allow early intervention and improve outcomes.
According to the literature, the estimated worldwide prevalence of ADHD is 5%–7%.4,5 Since most epidemiological studies in the literature focus on school-age children, there is a dearth of data on preschool-age children and adults. Taking only children and adolescents into account, the reported prevalence ranges from 5.90% to 7.20%.6,7 When it comes to preschool-age children, prevalences ranging from 2% to 18% have been reported.2,7,8 To our knowledge, no population-based epidemiological studies on paediatric ADHD have been conducted in Portugal.
Sleep is an active and dynamic physiological process that is crucial for growth and development and is closely associated with many other neurophysiological mechanisms.1 Sleep habits are influenced by many factors, including biological (such as the neurodevelopmental stage), psychological, environmental and family-related ones.9,10
Sleep disorders are frequent disturbances in childhood, with an estimated prevalence of 25%–40%. In Portugal, preliminary studies suggest a high incidence of sleep-related complaints and deleterious sleep habits in children. However, few studies have addressed sleep habits in preschoolers, who are particularly vulnerable to sleep disruptions.1,11,12 Sleep-related problems have been linked to a range of adverse health outcomes, including emotional and behavioural dysregulation, poor academic performance, increased risk of accidents and obesity.1,9,13
There is growing interest in the relationship between sleep and ADHD, as there is evidence that sleep problems are among the most frequent comorbidities associated with ADHD.1,14,15 Between 70% and 85% of children with ADHD experience sleep problems, which may arise from poor sleep hygiene, comorbidities, a shared biological component or as an adverse effect of treatment with stimulant medications.16 Insomnia is common in children with ADHD, particularly resistance in going to bed and nighttime awakenings. There is also evidence that, overall, children with ADHD are more likely to experience sleep disordered breathing and periodic limb movement disorder.17 While there are plenty of studies on sleep patterns in children with ADHD, few have focused on nonclinical samples of preschoolers or investigated the direct association between sleep-related phenomena and ADHD symptoms.
Therefore, we aimed to assess the prevalence of high scores for ADHD symptoms in a sample of preschoolers aged 3–6 years in Porto, Portugal, to characterize their sleeping habits and identify sleep-related problems, and to study the association between high scores for ADHD symptoms and sleep disturbances.
MethodsWe conducted a school-based cross-sectional survey in Porto, Portugal. We provided a total of 1047 questionnaires to the caregivers of children enrolled in 22 randomly selected early childhood education centres, both public and private. The study only included children aged 3–6 years whose legal guardians signed the informed consent form allowing participation.
The caregivers of the preschoolers completed the self-administered questionnaires at home and then returned them to the teacher in the days that followed. The response rate was 37.2% (389 participants). We excluded questionnaires with missing values for more than 20% of items from the sample. The other exclusion criteria were the presence of neurodevelopmental or psychiatric disorder in the child reported by the parent and the use of medication that could impact sleep. Ultimately, the analysis included data regarding 381 preschoolers from seven civil parishes in Porto.
We collected data on the following sociodemographic characteristics: child’s age (3–6 years) and sex (male/female), and parental age (≤25th percentile, 25th–75th percentile, ≥75th percentile), nationality (Portuguese/other) and educational attainment (<9th grade, 9th grade, 12th grade, undergraduate degree or higher) and household structure (nuclear with and without siblings, single parent with and without siblings, and other). Open-ended questions were used to assess the child’s overall health and usual medication.
We assessed ADHD symptoms with the Portuguese version of the Conners’ Parent Rating Scale-Revised (CPRS-R), a validated screening tool for parent-proxy assessment of ADHD-related behaviours.18 This 27-item questionnaire reflects parental perceptions of the child’s behaviours in the past month. Items are scored on a Likert scale ranging from 0 to 3 points that reflects the frequency with which the child exhibits the behaviour (never, rarely, sometimes or very often). This yields a total score that is further divided into 3 subscales: cognitive problems/inattention, excessive motor activity and attention deficit/hyperactivity. In turn, these values correspond to percentiles that indicate which children are at risk of ADHD. A score above the 74th percentile (P74) is considered clinically relevant. The higher the percentile, the greater the risk of ADHD.
When it came to sleep, we used the Portuguese version of the Children’s Sleep Habits Questionnaire (CSHQ-PT), a retrospective parent-report questionnaire validated to screen sleep disturbances in Portuguese children, including those with ADHD.11,19 It comprises 33 items grouped into eight subscales that reflect the following sleep domains: bedtime resistance, sleep onset delay, sleep duration, sleep anxiety, night wakings, parasomnias, sleep-disordered breathing and daytime sleepiness. The sleep disturbance index (SDI) is then obtained by adding the partial scores of the subscales. Previous evidence shows that a cut-off value of 48 is the optimal threshold for sleep disturbance screening in the Portuguese population.20
Based on the recommendations of the American Academy of Pediatrics, television (TV) watching time was categorised into less than 1 h a day versus 1 or more on weekdays, and less than 2 h a day versus 2 h or more on weekends.21 Engagement in outdoor activities was reported with the categories often, sometimes and seldom.
The study adhered to all relevant national regulations and institutional policies as well as to the principles of the Declaration of Helsinki. It was approved by the Ethics Committee of Centro Hospitalar Universitário do Porto and Institute of Biomedical Sciences Abel Salazar. We obtained written informed consent from the parents of all patients included in the study.
The statistical analyses were performed with the software SPSS Statistics, version 26. We conducted a descriptive analysis of all the study variables and calculated the prevalence of high scores for ADHD symptoms. We have summarised categorical variables as absolute frequencies and percentages and compared them using the χ2 test. We assessed for significant associations by fitting logistic regression models and calculating odds ratios (ORs). We considered P values of less than 0.05 statistically significant.
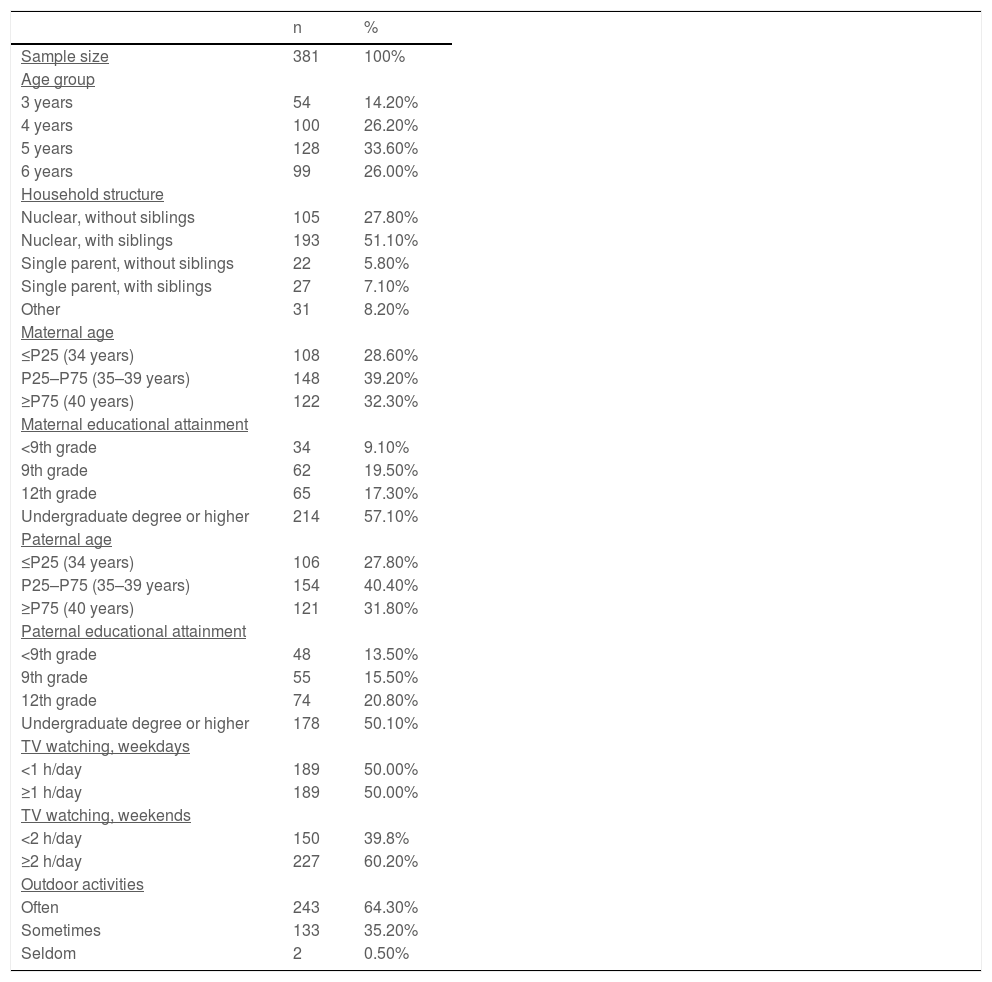
ResultsTable 1 presents the sociodemographic characteristics of the sample. The final analysis included 381 preschoolers, 194 (50.90%) male and 187 (49.10%) female. The median age of the participants was 5 years (interquartile range [IQR], 4–6). As regards nationality, 93.80% of the mothers and 92.10% and the fathers were Portuguese. Most parents were aged 35–39 years (39.20% and 40.40%) and had an undergraduate degree or higher (57.10% and 50.10%). When it came to outdoor activities, 64.30% of caregivers reported that their children engaged in them often. As for screentime, we found that 50.00% of preschoolers watched TV for 1 or more hours a day on weekdays and 60.20% for 2 or more hours a day on weekends.
Sociodemographic characteristics of the sample.
| n | % | |
|---|---|---|
| Sample size | 381 | 100% |
| Age group | ||
| 3 years | 54 | 14.20% |
| 4 years | 100 | 26.20% |
| 5 years | 128 | 33.60% |
| 6 years | 99 | 26.00% |
| Household structure | ||
| Nuclear, without siblings | 105 | 27.80% |
| Nuclear, with siblings | 193 | 51.10% |
| Single parent, without siblings | 22 | 5.80% |
| Single parent, with siblings | 27 | 7.10% |
| Other | 31 | 8.20% |
| Maternal age | ||
| ≤P25 (34 years) | 108 | 28.60% |
| P25–P75 (35–39 years) | 148 | 39.20% |
| ≥P75 (40 years) | 122 | 32.30% |
| Maternal educational attainment | ||
| <9th grade | 34 | 9.10% |
| 9th grade | 62 | 19.50% |
| 12th grade | 65 | 17.30% |
| Undergraduate degree or higher | 214 | 57.10% |
| Paternal age | ||
| ≤P25 (34 years) | 106 | 27.80% |
| P25–P75 (35–39 years) | 154 | 40.40% |
| ≥P75 (40 years) | 121 | 31.80% |
| Paternal educational attainment | ||
| <9th grade | 48 | 13.50% |
| 9th grade | 55 | 15.50% |
| 12th grade | 74 | 20.80% |
| Undergraduate degree or higher | 178 | 50.10% |
| TV watching, weekdays | ||
| <1 h/day | 189 | 50.00% |
| ≥1 h/day | 189 | 50.00% |
| TV watching, weekends | ||
| <2 h/day | 150 | 39.8% |
| ≥2 h/day | 227 | 60.20% |
| Outdoor activities | ||
| Often | 243 | 64.30% |
| Sometimes | 133 | 35.20% |
| Seldom | 2 | 0.50% |
P25, 25th percentile, P75, 75th percentile.
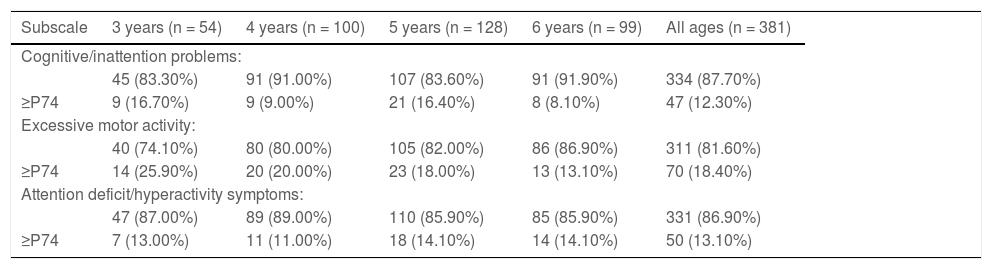
Table 2 presents the scores obtained in each subscale of the Portuguese version of the CPRS-R, overall and by age group. In the total sample of preschoolers, we found that 12.30% of the sample had high levels (defined as a score ≥ P74) of cognitive/inattention problems and 18.40% high levels of excessive motor activity. Also in the total sample, 13.10% of preschoolers had high levels of attention deficit/hyperactivity symptoms. The prevalence of high levels of ADHD symptoms was 13.00%, 11.00% and 14.10%, in children aged 3, 4 and 5-to-6 years, respectively. We found a higher prevalence of ADHD symptoms in girls compared to boys (14.40% vs 11.85%; P = 0.276).
Scores of the Portuguese version of the Revised Conners Parent Rating Scale (CPRS-R) according to age-group and subscales.
| Subscale | 3 years (n = 54) | 4 years (n = 100) | 5 years (n = 128) | 6 years (n = 99) | All ages (n = 381) |
|---|---|---|---|---|---|
| Cognitive/inattention problems: | |||||
| 45 (83.30%) | 91 (91.00%) | 107 (83.60%) | 91 (91.90%) | 334 (87.70%) | |
| ≥P74 | 9 (16.70%) | 9 (9.00%) | 21 (16.40%) | 8 (8.10%) | 47 (12.30%) |
| Excessive motor activity: | |||||
| 40 (74.10%) | 80 (80.00%) | 105 (82.00%) | 86 (86.90%) | 311 (81.60%) | |
| ≥P74 | 14 (25.90%) | 20 (20.00%) | 23 (18.00%) | 13 (13.10%) | 70 (18.40%) |
| Attention deficit/hyperactivity symptoms: | |||||
| 47 (87.00%) | 89 (89.00%) | 110 (85.90%) | 85 (85.90%) | 331 (86.90%) | |
| ≥P74 | 7 (13.00%) | 11 (11.00%) | 18 (14.10%) | 14 (14.10%) | 50 (13.10%) |
P74, 74th percentile.
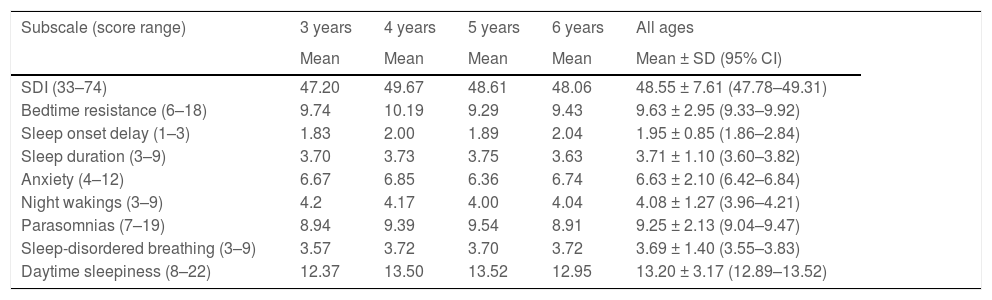
As regards night sleep duration, we found that the proportion of participants that met the recommended number of sleeping hours for preschool-age children (10–13 per day) was 87.50% on weekdays and 91.60% on weekends.22,23Table 3 shows the mean scores obtained in the subscales of the CSHQ-PT by age group. We found out that 45.70% of participants had a SDI greater than 48, which is the cut-off point recommended for screening sleep disorders in the Portuguese population. The mean SDI was 48.55 (standard deviation [SD], 7.61) in the full sample, and 49.67 (SD, 7.27), 48.61 (SD, 7.68) and 48.06 (SD, 8.33) in children aged 4, 5 and 6 years, respectively.
Mean scores obtained in the Portuguese version of the Children’s Sleep Habits Questionnaire (CSHQ-PT) by age-group, overall and in each of the 8 subscales.
| Subscale (score range) | 3 years | 4 years | 5 years | 6 years | All ages |
|---|---|---|---|---|---|
| Mean | Mean | Mean | Mean | Mean ± SD (95% CI) | |
| SDI (33–74) | 47.20 | 49.67 | 48.61 | 48.06 | 48.55 ± 7.61 (47.78–49.31) |
| Bedtime resistance (6–18) | 9.74 | 10.19 | 9.29 | 9.43 | 9.63 ± 2.95 (9.33–9.92) |
| Sleep onset delay (1–3) | 1.83 | 2.00 | 1.89 | 2.04 | 1.95 ± 0.85 (1.86–2.84) |
| Sleep duration (3–9) | 3.70 | 3.73 | 3.75 | 3.63 | 3.71 ± 1.10 (3.60–3.82) |
| Anxiety (4–12) | 6.67 | 6.85 | 6.36 | 6.74 | 6.63 ± 2.10 (6.42–6.84) |
| Night wakings (3–9) | 4.2 | 4.17 | 4.00 | 4.04 | 4.08 ± 1.27 (3.96–4.21) |
| Parasomnias (7–19) | 8.94 | 9.39 | 9.54 | 8.91 | 9.25 ± 2.13 (9.04–9.47) |
| Sleep-disordered breathing (3–9) | 3.57 | 3.72 | 3.70 | 3.72 | 3.69 ± 1.40 (3.55–3.83) |
| Daytime sleepiness (8–22) | 12.37 | 13.50 | 13.52 | 12.95 | 13.20 ± 3.17 (12.89–13.52) |
CI, confidence interval; SD, standard deviation; SDI, sleep disturbance index.
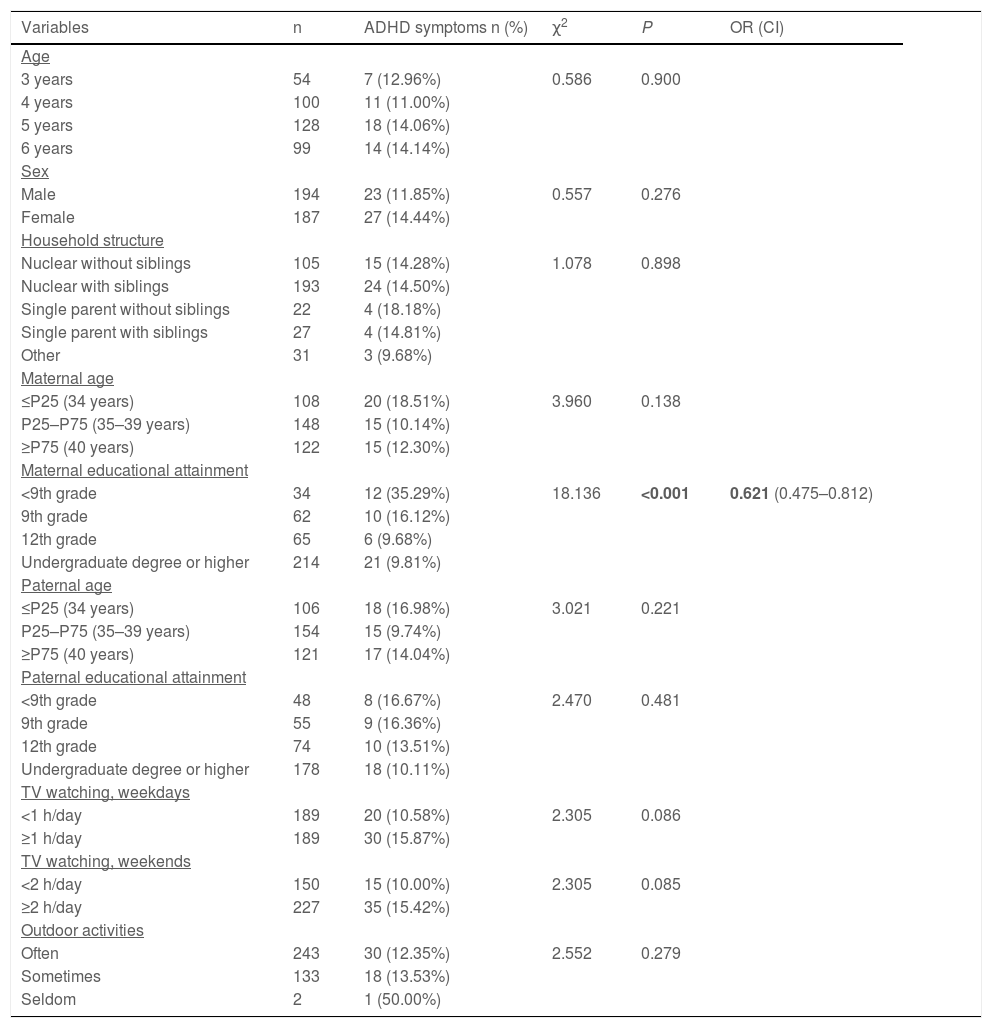
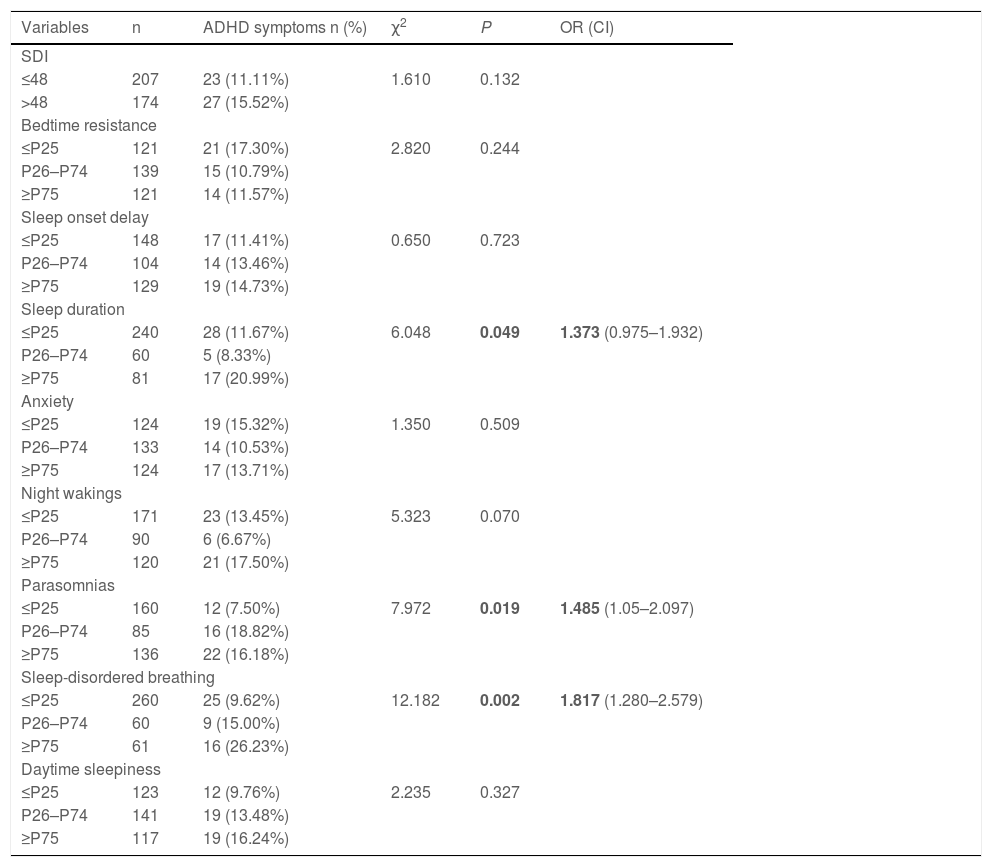
Tables 4 and 5 present the results of cross-tabulation analyses followed by logistic regression analysis for assessment of the association of high levels of ADHD symptoms (defined as a score ≥ P74 in the attention deficit/hyperactivity symptoms subscale of the CPRS-R) with sociodemographic variables and with sleep habits, respectively. We found that high levels of ADHD symptoms were significantly associated with lower maternal educational attainment level (OR, 0.621; confidence interval [CI], 0.475–0.812; P = 0.001), shorter sleep duration (OR, 1.373; CI, 0.975–1.932; P = 0.049) and higher scores in the parasomnias (OR, 1.485; CI, 1.051–2.097; P = 0.019) and sleep disordered breathing (OR, 1.817; CI, 1.280–2.579; P = 0.002) subscales of the CSQH-PT.
Results of the χ2 test and logistic regression analysis on the association of high levels of ADHD symptoms and sociodemographic variables.
| Variables | n | ADHD symptoms n (%) | χ2 | P | OR (CI) |
|---|---|---|---|---|---|
| Age | |||||
| 3 years | 54 | 7 (12.96%) | 0.586 | 0.900 | |
| 4 years | 100 | 11 (11.00%) | |||
| 5 years | 128 | 18 (14.06%) | |||
| 6 years | 99 | 14 (14.14%) | |||
| Sex | |||||
| Male | 194 | 23 (11.85%) | 0.557 | 0.276 | |
| Female | 187 | 27 (14.44%) | |||
| Household structure | |||||
| Nuclear without siblings | 105 | 15 (14.28%) | 1.078 | 0.898 | |
| Nuclear with siblings | 193 | 24 (14.50%) | |||
| Single parent without siblings | 22 | 4 (18.18%) | |||
| Single parent with siblings | 27 | 4 (14.81%) | |||
| Other | 31 | 3 (9.68%) | |||
| Maternal age | |||||
| ≤P25 (34 years) | 108 | 20 (18.51%) | 3.960 | 0.138 | |
| P25–P75 (35–39 years) | 148 | 15 (10.14%) | |||
| ≥P75 (40 years) | 122 | 15 (12.30%) | |||
| Maternal educational attainment | |||||
| <9th grade | 34 | 12 (35.29%) | 18.136 | <0.001 | 0.621 (0.475–0.812) |
| 9th grade | 62 | 10 (16.12%) | |||
| 12th grade | 65 | 6 (9.68%) | |||
| Undergraduate degree or higher | 214 | 21 (9.81%) | |||
| Paternal age | |||||
| ≤P25 (34 years) | 106 | 18 (16.98%) | 3.021 | 0.221 | |
| P25–P75 (35–39 years) | 154 | 15 (9.74%) | |||
| ≥P75 (40 years) | 121 | 17 (14.04%) | |||
| Paternal educational attainment | |||||
| <9th grade | 48 | 8 (16.67%) | 2.470 | 0.481 | |
| 9th grade | 55 | 9 (16.36%) | |||
| 12th grade | 74 | 10 (13.51%) | |||
| Undergraduate degree or higher | 178 | 18 (10.11%) | |||
| TV watching, weekdays | |||||
| <1 h/day | 189 | 20 (10.58%) | 2.305 | 0.086 | |
| ≥1 h/day | 189 | 30 (15.87%) | |||
| TV watching, weekends | |||||
| <2 h/day | 150 | 15 (10.00%) | 2.305 | 0.085 | |
| ≥2 h/day | 227 | 35 (15.42%) | |||
| Outdoor activities | |||||
| Often | 243 | 30 (12.35%) | 2.552 | 0.279 | |
| Sometimes | 133 | 18 (13.53%) | |||
| Seldom | 2 | 1 (50.00%) | |||
ADHD, attention-deficit hyperactivity disorder; CI, confidence interval; OR, odds ratio; P25, 25th percentile; P75, 75th percentile.
Results of the χ2 test and logistic regression analysis on the association of high levels of ADHD symptoms the mean scores obtained in the Portuguese version of the Children’s Sleep Habits Questionnaire (CSHQ-PT).
| Variables | n | ADHD symptoms n (%) | χ2 | P | OR (CI) |
|---|---|---|---|---|---|
| SDI | |||||
| ≤48 | 207 | 23 (11.11%) | 1.610 | 0.132 | |
| >48 | 174 | 27 (15.52%) | |||
| Bedtime resistance | |||||
| ≤P25 | 121 | 21 (17.30%) | 2.820 | 0.244 | |
| P26–P74 | 139 | 15 (10.79%) | |||
| ≥P75 | 121 | 14 (11.57%) | |||
| Sleep onset delay | |||||
| ≤P25 | 148 | 17 (11.41%) | 0.650 | 0.723 | |
| P26–P74 | 104 | 14 (13.46%) | |||
| ≥P75 | 129 | 19 (14.73%) | |||
| Sleep duration | |||||
| ≤P25 | 240 | 28 (11.67%) | 6.048 | 0.049 | 1.373 (0.975–1.932) |
| P26–P74 | 60 | 5 (8.33%) | |||
| ≥P75 | 81 | 17 (20.99%) | |||
| Anxiety | |||||
| ≤P25 | 124 | 19 (15.32%) | 1.350 | 0.509 | |
| P26–P74 | 133 | 14 (10.53%) | |||
| ≥P75 | 124 | 17 (13.71%) | |||
| Night wakings | |||||
| ≤P25 | 171 | 23 (13.45%) | 5.323 | 0.070 | |
| P26–P74 | 90 | 6 (6.67%) | |||
| ≥P75 | 120 | 21 (17.50%) | |||
| Parasomnias | |||||
| ≤P25 | 160 | 12 (7.50%) | 7.972 | 0.019 | 1.485 (1.05–2.097) |
| P26–P74 | 85 | 16 (18.82%) | |||
| ≥P75 | 136 | 22 (16.18%) | |||
| Sleep-disordered breathing | |||||
| ≤P25 | 260 | 25 (9.62%) | 12.182 | 0.002 | 1.817 (1.280–2.579) |
| P26–P74 | 60 | 9 (15.00%) | |||
| ≥P75 | 61 | 16 (26.23%) | |||
| Daytime sleepiness | |||||
| ≤P25 | 123 | 12 (9.76%) | 2.235 | 0.327 | |
| P26–P74 | 141 | 19 (13.48%) | |||
| ≥P75 | 117 | 19 (16.24%) | |||
ADHD, attention-deficit hyperactivity disorder; CI, confidence interval; OR, odds ratio; P25, 25th percentile; P26, 26th percentile, P74, 74th percentile, P75, 75th percentile; SDI, sleep disturbance index.
P-values <0.05 were considered statistically significant.
In our sample the prevalence of high levels of ADHD symptoms was 13.10%. The results for the total sample and for each age group (Table 2) were consistent with the literature, as epidemiological studies have estimated that the prevalence of ADHD in preschoolers ranges from 2% to 18%.2,7,8 This wide range is explained by several factors, including differences in the applied diagnostic criteria, the source of information (parents or teachers) and the sociodemographic characteristics of the population. In this sample, there was a slightly higher prevalence of ADHD symptoms in girls compared to boys, a difference that was not statistically significant. We ought to underscore that the questionnaire used for screening can only suggest the presence of ADHD symptoms, and actual diagnosis requires an individualised clinical assessment.
Although most parents reported that their children slept the recommended number of hours for preschoolers on both weekdays and weekends, 45.70% of participants had a SDI higher than 48 in the CSQH-PT, which is the recommended cut-off point for screening of sleep disorders in the Portuguese population.19 As can be seen in Table 3, this was also the case of children aged 4–6 years, while the mean SDI was slightly lower in the group aged 3 years (47.20; SD, 6.46). The mean SDI for the entire sample was 48.55 (SD, 7.61). Although cut-off values have not been established for the subscale scores, the results were concerning, as they suggested that nearly half of the sample should be evaluated for sleep disturbances.
We further analysed the group of children with high levels of ADHD symptoms to assess for potential correlations to sociodemographic characteristics, TV watching time and outdoor activity. We did not find statistically significant associations with age, household structure, parental age or outdoor activities, but lower maternal educational attainment was associated with high levels of ADHD symptoms (P < 0.001). Although the questionnaire only addressed TV watching time, there is increasing evidence that that overall screen time is greater than TV watching time, even at early ages. Thus, it is reasonable to infer that the screen time of these children far exceeds the maximum number of hours recommended by the American Academy of Pediatrics on weekdays and weekends.21 Previous studies have identified parental education and TV watching as risk factors for ADHD symptoms, findings similar to ours.18 A recent review concluded that there is a relationship between children’s media use and ADHD-related behaviours, albeit statistically small.24 Population-based studies continue to show associations between excessive TV watching in early childhood and cognitive, language, social and emotional delays. Additionally, excessive exposure to screens, particularly in the child’s bedroom, has been associated with shorter sleep duration.21 Nevertheless, further research is needed to fully understand the mechanisms of this association.
Contrary to school-age children, the impact of sleep problems in preschoolers is not well documented. We found that the probability of having high levels of ADHD symptoms was 1.373 times greater in children with shorter sleep duration (OR, 1.373; CI, 0.975–1.932; P = 0.049). The probability was also greater in preschoolers with higher scores in the parasomnias (OR, 1.485; CI, 1.051–2.097; P = 0.019) and sleep disordered breathing (OR, 1.817; CI, 1.280–2.579; P = 0.002) subscales of the CHQH-PT, which was consistent with the findings of previous studies. A large population-based study conducted in Australia showed that preschoolers with sleep problems (including difficulty falling asleep and snoring) were more likely to have ADHD.25 A meta-analysis revealed that children with ADHD exhibited significantly greater bedtime resistance, more sleep onset difficulties, night wakings, difficulty waking in the morning, sleep disordered breathing and daytime sleepiness compared to controls.26 Melegari et al. proposed that temperament might be an endophenotype underlying the association between ADHD and sleep disorders in preschoolers.27 More recently, findings from a population-based cohort study suggested that sleep disturbances in early life may be more important ADHD predictors than sleep duration, although the underlying mechanisms and differential roles of sleep duration and problems and ADHD still need to be clarified.15 Based on our findings and the current scientific evidence, sleep-related problems can be considered risk factors for the development of ADHD symptoms.
We ought to discuss the following strengths and limitations of our study. First, its cross-sectional design did not allow us to establish causality in the association of the variables under study. Another limitation involves the variables themselves, as most had a subjective nature and were assessed by means of parental reports. Furthermore, our sample included only children living in urban settings in Porto. Specifically, when it came to educational attainment, parents that chose to participate had an undergraduate degree or higher. This may have been a source of selection bias, as more educated people tend to be more willing to actively participate in scientific research. Further studies are needed to objectively measure sleep parameters and their relationship with ADHD symptoms in preschoolers, possibly including information about napping habits and periodic limb movements during sleep in addition to data provided by schoolteachers. Despite these limitations, we believe our sample to be representative of Portuguese preschoolers, as we randomly selected a nonclinical sample of children from both public and private kindergartens and the sample size was appropriate.
In conclusion, we found that both sleep-related problems and ADHD symptoms were common in Portuguese preschoolers living in Porto, and this study is a useful initial step in identifying some clinical correlations between them. Our findings highlight the importance of elucidating the complex relationship between sleep and ADHD, which is far from being understood. We found that children with lower sleep duration and sleep-related problems (namely parasomnias and sleep disordered breathing) had a higher probability of having ADHD symptoms. Therefore, it is our opinion that clinicians should always assess sleep when evaluating a child with ADHD symptoms and also screen for ADHD symptoms in children presenting with any type of sleep disorder. Future studies are required to define strategies for prevention and early intervention in young children at risk of ADHD.
Pre-presentation: The study was presented at the 7th ADHD World Congress, April 25–28, 2019, Lisbon, Portugal, and the CMIN Summit, July 5–6, 2019, Porto, Portugal.