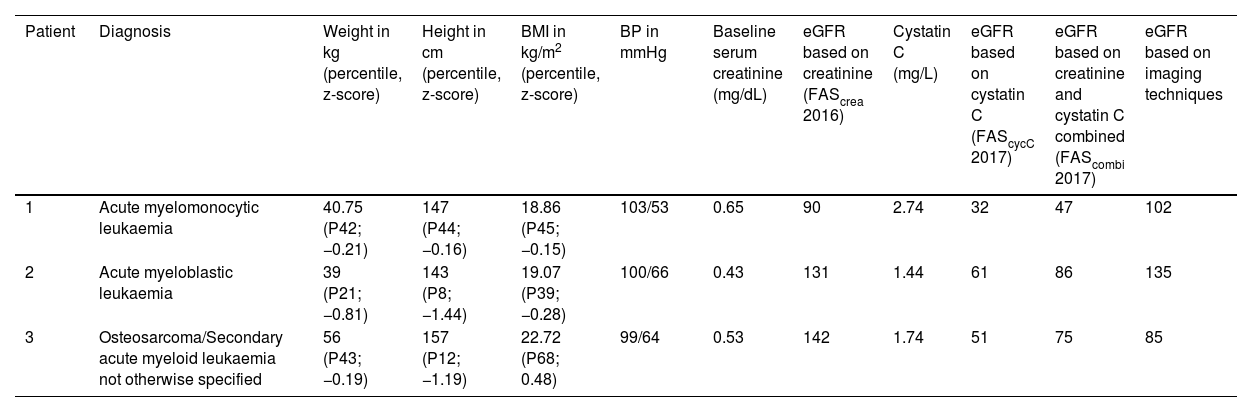
The assessment of glomerular filtration is a necessary practice in oncological patients, given the nephrotoxicity of the drugs used for treatment and its usefulness in guiding prescribing. We present 3 cases in which there was a discrepancy between creatinine and cystatin C-based estimates in patients with a history of acute myeloid leukaemia (Table 1).
Characteristics of the patients.
| Patient | Diagnosis | Weight in kg (percentile, z-score) | Height in cm (percentile, z-score) | BMI in kg/m2 (percentile, z-score) | BP in mmHg | Baseline serum creatinine (mg/dL) | eGFR based on creatinine (FAScrea 2016) | Cystatin C (mg/L) | eGFR based on cystatin C (FAScycC 2017) | eGFR based on creatinine and cystatin C combined (FAScombi 2017) | eGFR based on imaging techniques |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Acute myelomonocytic leukaemia | 40.75 (P42; −0.21) | 147 (P44; −0.16) | 18.86 (P45; −0.15) | 103/53 | 0.65 | 90 | 2.74 | 32 | 47 | 102 |
| 2 | Acute myeloblastic leukaemia | 39 (P21; −0.81) | 143 (P8; −1.44) | 19.07 (P39; −0.28) | 100/66 | 0.43 | 131 | 1.44 | 61 | 86 | 135 |
| 3 | Osteosarcoma/Secondary acute myeloid leukaemia not otherwise specified | 56 (P43; −0.19) | 157 (P12; −1.19) | 22.72 (P68; 0.48) | 99/64 | 0.53 | 142 | 1.74 | 51 | 75 | 85 |
BMI, body mass index; BP, blood pressure; eGFR, estimated glomerular filtration rate.
The eGFR is expressed as mL/min/1.73 m2 and was calculating based on the creatinine level, cystatin C level or both combined through the Full-Age Spectrum (FAS) equations6 published in 2016 and 2017, respectively, with the corresponding adjustment for height of the FAScrea in patients 1 and 2 (FAScrea-height), and the FAScombi.
The first was a girl aged 11 years, with no personal or family history of renal or urinary tract disease, who, prior to initiation of treatment, exhibited abnormal levels of cystatin C as high as 2.74 mg/L (turbidimetric assay traceable to ERM-DA471/IFCC), with repeated measurements of creatinine within the normal range (0.55−0.65 mg/dL) (enzymatic assay traceable to IDMS). Blood pressure measurements were within the normal range and the patient had not lost a significant amount of weight. Blood chemistry tests ruled out thyroid disorders and the routine urinalysis revealed mild proteinuria that was likely to be due to hyperfiltration secondary to hyperhydration. Steroid therapy has not been initiated. A renal ultrasound scan showed mild nonspecific echogenicity of the renal parenchyma. Last of all, filtration was measured by means of Cr-ethylenediamine tetraacetic acid (EDTA) scintigraphy, yielding a value of 102 mL/min/1.73 m2, which confirmed normal glomerular filtration, and the patient started treatment and has been free of nephrological complications to date.
The second was a boy aged 12 years who had undergone allogeneic haematopoietic stem cell transplantation (HSCT) one year prior and was in remission at the time he was referred to our clinic due to progressive worsening of renal function as inferred by the cystatin C level (1.44 mg/L) while the creatinine level remained stable (0.43 mg/dL). This was initially attributed to different drugs: baricitinib, used for treatment of cutaneous graft versus host disease, and acyclovir used for prophylaxis. His weight and blood pressure were within the normal range. The results of the blood and urine tests were normal, thyroid disease was ruled out and the patient was not receiving steroids. The glomerular filtration rate was measured with Tc-99 diethylenetriaminepentaacetic acid (DTPA) scintigraphy, which yielded a value of 135 mL/min/1.73 m2, within the normal range.
The third patient was a young woman aged 20 years with leukaemia secondary to osteosarcoma of the right femur, both in remission, who had undergone HSCT 2 years before. In recent follow-up visits, there had been a progressive increase in the levels of cystatin C to up to 1.74 mg/L, while creatinine levels remained stable at 0.5 mg/dL. The patient had normal anthropometric measurements and did not have hypertension. She was in treatment with levothyroxine for hypothyroidism, with adequate control. There were no urinary abnormalities and the renal ultrasound scan showed mild hyperechogenicity. The patient was not on steroid therapy. Suspending the nephrotoxic drugs she was receiving for prophylaxis, acyclovir and posaconazole did not resolve the discrepancy, which prompted measurement of the GFR with Tc-99 DTPA scintigraphy, the result of which was 85 mL/min/1.73 m2, a value in between those estimated based on the cystatin C and creatinine levels and indicative of mild chronic renal disease.
Cystatin C is a low molecular weight protein synthesised by all nucleated cells. It is considered the ideal endogenous marker of glomerular filtration, as it is freely filtered in the renal glomeruli and almost completely reabsorbed and catabolized in the proximal tubules, while its levels appear to be independent from sex, age, muscle mass or dietary habits.1 However, cystatin C may be elevated not only in the context of renal impairment, but also of thyroid disorders or with the use of corticosteroids.1,2 In the field of oncology, it has been found to play opposite roles in multiple types of cancer, as both a tumour suppressor and a tumour promoter.3 Thus, cystatin C may have a protective effect by inhibiting the activity of lysosomal cysteine proteinases, which have been found to be associated with tumour progression and metastasis.3 Its elevation unrelated to glomerular filtration has been described previously in adults with solid and blood tumours before initiation of treatment1,2 and as a result of chemotherapy.4 Different case series have found a subsequent descent in patients in remission.1,2 Thus, cystatin C may be useful as a biomarker3 and indicator of tumour burden.2
Last of all, there are specific circumstances in which accurate measurement of the glomerular filtration rate is required, which can be achieved by measurement of an exogenous marker, such as radioactive tracers like Cr-EDTA or Tc-99 DTPA, which yield values that are in agreement with each other, or iodinated contrast agents, such as the plasma clearance of iohexol, which is strongly correlated to the urinary inulin clearance.5
We present the cases of 3 patients with leukaemia in whom glomerular filtration rate estimates were corroborated using isotopic markers. The discrepancy with the estimates obtained based on the level of creatinine highlight the need to interpret cystatin C levels with caution in the context of malignancy, both at diagnosis and during the follow-up, and the need to introduce new markers in everyday clinical practice that provide a more accurate assessment of glomerular filtration.