In the treatment of patients with acute bronchiolitis there is great variability in clinical practice. Treatments whose efficacy has not been demonstrated are frequently used despite the recommendations contained in the Clinical Practice Guidelines.
Material and methodsA quality improvement strategy is implemented in the care of patients with acute bronchiolitis in the Emergency Department, which is maintained for five years and is periodically updated to be increasingly restrictive regarding the use of bronchodilators. To evaluate the impact of the intervention, a retrospective study of the rates of prescription of bronchodilators in children diagnosed with acute bronchiolitis in the month of December of four epidemic periods (2012, 2014, 2016 and 2018) was carried out.
Results1767 children are included. There were no differences regarding age, respiratory rate, oxygen saturation or the estimated severity in each of the study seasons. The use of salbutamol in the Emergency Department decreased from 51.2% (95% CI: 46.6–55.8%) in 2012 to 7.8% (95% CI: 5.7%–10.5%) in 2018 (P < .001) and epinephrine prescription rates fell from 12.9% (95% CI: 10.1%–16.3%) to 0.2% (95% CI: 0–1.1%) (P < .001). At the same time, there was a decrease in the median time of attendance in the Emergency Department and in the admission rate without changing the readmission rate in 72 h.
ConclusionsThe systematic and continuous deployment over time of actions aimed at reducing the use of salbutamol and epinephrine in the treatment of bronchiolitis, prior to the epidemic period, seems an effective strategy to reduce the use of bronchodilators in the Emergency Department.
En el tratamiento de los pacientes con bronquiolitis aguda existe una gran variabilidad de la práctica clínica y con frecuencia se utilizan de forma indiscriminada tratamientos cuya eficacia no está demostrada a pesar de las recomendaciones recogidas en las guías de práctica clínica.
Material y metodosSe implementó una estrategia de mejora de la calidad en la atención a los pacientes con bronquiolitis aguda en el Servicio de Urgencias que se mantuvo durante cinco años y se actualizó periódicamente para ser cada vez más restrictiva respecto al uso de tratamientos broncodilatadores. Para evaluar el impacto de la intervención se realizó un estudio descriptivo retrospectivo de las tasas de prescripción de broncodilatadores en los niños diagnosticados de bronquiolitis aguda en el mes de diciembre de cuatro periodos epidémicos (2012, 2014, 2016 y 2018).
ResultadosSe incluyeron 1.767 niños. No existieron diferencias respecto a edad, frecuencia respiratoria, saturación de oxígeno ni gravedad en cada una de las temporadas a estudio. El empleo de salbutamol en Urgencias descendió del 51,2% (IC 95%: 46,6–55,8%) en 2012 al 7,8% (IC 95%: 5,7–10,5%) en 2018 (p < 0,001) y el de adrenalina de 12,9% (IC 95%:10,1–16,3%) a 0,2% (IC 95%:0–1,1%) (p < 0.001). Se produjo a su vez un descenso en la mediana de tiempo de asistencia en Urgencias y en la tasa de ingreso sin que se modificase la tasa de readmisión en 72 h.
ConclusionesEl despliegue sistemático y continuado en el tiempo de acciones dirigidas a la reducción del uso de fármacos en el tratamiento de la bronquiolitis, previo al periodo epidémico, parece una estrategia eficaz para reducir el uso de broncodilatadores en urgencias.
Acute bronchiolitis (AB) is one of the most important pathologies in paediatrics.1 It is the most common lower respiratory tract infection in the first year of life, with an annual incidence of 10%–30%.2,3 In Spain it is the leading cause of hospitalisation in children under one year of age.4 The main aetiological agent is the respiratory syncytial virus (RSV), with a variable frequency of around 65%–85%.5,6 There is no other acute disease that has such an important effect on the health of infants and that produces such a high social and economic impact as AB.7
The diagnosis must be clinical, based on the findings from the medical history and physical examination. Routine performance of diagnostic tests is not recommended.8–12
As for treatment, there is great variability in clinical practice in every care setting, and treatments of unproven efficacy are often used indiscriminately.13–16 For this reason, more and more authors are suggesting that the time has come to recognise the limitations of therapeutic interventions and to focus efforts on doing more for the patient with less medication.17 Numerous meta-analyses have clarified the efficacy of the available therapeutic options.18–20 These have given rise to new clinical practice guidelines (CPGs) which discourage the use of bronchodilator treatments.10–12
The difficulties that arise in care delivery when trying to apply the best evidence included in CPGs to everyday practice are well known.21 In the case of AB, the recommendations of CPGs have had a limited impact.22–24 Consequently, some centres have adopted quality improvement strategies. There is a wide range of approaches and published results, and no evidence to identify which strategies are superior.25–28 In most cases it is a matter of implementing local protocols, with the intention of standardising management and putting into practice the recommendations formulated in CPGs.29 Acute bronchiolitis is a special case because the CPGs do not recommend specific interventions, but are rather designed to prevent excessive treatment and avoid unnecessary diagnostic procedures. Unfortunately, less research has been directed towards evaluating strategies for reducing the use of non-recommended resources than towards evaluating strategies for increasing the use of effective resources.30
The objective of this study is to analyse the impact of a quality improvement strategy, maintained over a period of five years, directed at care of patients with AB in the Emergency Department (ED), with the aim of bringing clinical practice closer to the available scientific evidence by decreasing the use of bronchodilator medication.
Materials and methodsThis is a retrospective descriptive study conducted in the ED of a specialised paediatric hospital which treats between 65 000 and 70 000 episodes per year. Medical staff participating in ED care during the study period included 8 paediatricians working full-time in the ED and 48 doctors from other paediatric specialties, as well as 120 paediatric residents and 50 family and community medicine residents.
HypothesisThe quality improvement strategy implemented is associated with a reduction in the use of bronchodilators (salbutamol and epinephrine) for the treatment of patients with AB, without affecting emergency care outcomes (rate of admission, rate of readmission, length of stay).
Study sampleWe included all the patients that met the diagnostic criteria for AB treated in the ED in the month of December in 4 epidemic seasons: 2012 (preintervention), 2014, 2016 and 2018. For this purpose, we manually reviewed all the ED discharge reports with a diagnostic code of “acute bronchiolitis” (ICD-9: 466.1 and ICD-10: J21) or “acute bronchitis” (ICD-9: 466.0 and ICD-10: J20). We defined AB as the first episode of wheezing with acute onset preceded by signs of viral upper respiratory tract infection in children younger than 24 months. We chose the month of December as it invariably coincides with the peak of the respiratory syncytial virus (RSV) epidemic season in Spain.
The exclusion criteria were
- -
Patients who after exhaustive review of the health records were found to have had previous episodes of bronchiolitis.
- -
Patients with incomplete data for the study variables.
We collected demographic data (date and time seen, age, sex) and clinical data (oxygen saturation, respiratory rate and severity). Severity was estimated according to the Wood-Downes scale modified by Ferrés31 up to 2016 and subsequently according to the Hospital de Cruces bronchiolitis assessment scale32 (Appendix B: Supplementary material).
InterventionThe improvement team consisted of two doctors from the paediatric emergency department. In 2013, we reviewed the health records of patients with AB treated in December 2012 with the aim of analysing the unnecessary therapeutic interventions used. Subsequently, we defined the objectives (use of bronchodilators in no more than 20% of patients) and designed the intervention, which began in 2014 and consisted of the following:
- -
Formulation of an AB protocol in the first year (2014), according to the scientific evidence and CPGs.
- -
Annual provision of a clinical teaching session, at the start of the epidemic, for all specialists and residents working in the ED, with presentation of the current protocol and the strategy. An email was also sent with the protocol, a summary of the recommendations and an up-to-date bibliography.
- -
Availability of all the documents on the intranet.
- -
Production and dissemination of printed resources: information sheets for parents, posters with the severity scale in examination rooms.
- -
Assessment of the results obtained each year by reviewing the histories of the patients treated in the month of December. In addition, as feedback, a second session was held in June at which these results were presented; information was also provided on the cost of non-indicated interventions and residents beginning their training were introduced to the strategy.
- -
The results obtained and the available scientific evidence led to the protocol being updated on two occasions: in 2016 (restriction of the use of bronchodilators to patients with severe AB who do not improve with oxygen therapy) and in 2018 (epinephrine as a therapeutic option removed from the protocol) (Table 1).
Table 1.Bronchodilator treatment recommendations in the emergency department.
2014 (1st version) 2016 (2nd version) 2018 (3rd version) Oxygen If O2Sat <94% If O2Sat <92% If O2Sat <92% Nebulised salbutamol Possibility of therapeutic test in patients older than 6 months with moderate or severe AB Therapeutic test in patients older than 6 months with severe AB that does not improve with oxygen Therapeutic test in patients older than 6 months with severe AB that does not improve with HFO Nebulised epinephrine Possibility of therapeutic test in patients younger than 6 months with moderate or severe AB Therapeutic test in patients younger than 6 months with severe AB that does not improve with oxygen Not recommended AB, acute bronchiolitis; HFO, high-flow oxygen; O2Sat: oxygen saturation.
- -
The primary measure of effect was the percentage of cases treated with salbutamol in the ED. The secondary measures of effect were the frequency of use of epinephrine in the ED and of prescription of salbutamol on discharge. To assess the possible undesired consequences of reducing these therapeutic interventions, the following benchmark measures were considered:
- -
Hospital admission rate: percentage of the patients who visited the ED admitted to the hospital.
- -
Length of stay in the ED: time elapsed from first contact with the doctor in charge to discharge; not calculated for patients admitted to hospital.
- -
Readmission rate: percentage of patients who returned to the ED for the same reason after receiving care in the ED in the previous 72 h. A distinction was made between patients who required hospitalisation and those discharged home again.
We summarised quantitative data using the mean and standard deviation. In the case of data that did not fit a normal distribution, we used the median and interquartile range (IQR) instead. We described categorical variables by means of absolute and relative frequencies. To compare the results for the variables under study in different years, we used the χ2 test for trend or the Fisher exact test in the case of qualitative data, or one-way analysis of variance (ANOVA) or the Kruskal–Wallis test if in the case of quantitative data, depending on whether or not they fit a normal distribution. We tested for normality using the Shapiro–Wilk test. We performed a multivariate analysis of the main results adjusted for age and severity. Statistical significance was defined as a P value of less than .05.
Ethical issuesThe studied conformed to the guidelines of the Oviedo Convention and the Declaration of Helsinki and was approved by the hospital’s clinical research ethics committee.
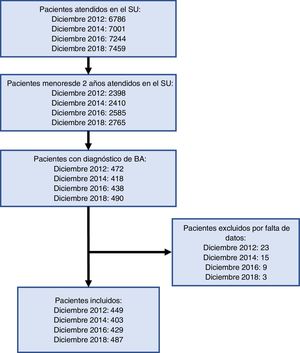
ResultsA total of 1767 children under the age of 2 years with AB were included in the study (Fig. 1). The annual reports of the ED indicate that 1017 episodes of AB were managed in 2012, 1126 in 2014, 1143 in 2016 and 1162 in 2018. The patients included in the study represented 44.1% of all AB cases managed in 2012, 35.8% in 2014, 37.5% in 2016 and 41.9% in 2018.
Table 2 presents the ages and clinical characteristics (respiratory rate, oxygen saturation and severity) of the patients included in each of the study periods.
Demographic and clinical characteristics of the patients with acute bronchiolitis.
| December 2012 | December 2014 | December 2016 | December 2018 | P value | |
|---|---|---|---|---|---|
| n | 449 | 403 | 429 | 487 | |
| Median age in months (IQR) | 5.7 (3.1–9.2) | 5.9 (3.3–9.0) | 6.5 (3.6–10.5) | 5.4 (3.0–8.9) | .167 |
| Median respiratory rate, bpm (IQR) | 48 (40–56) | 48 (41–55) | 48 (40–54) | 48 (42–56) | .903 |
| Median oxygen saturation, % (IQR) | 97 (96–99) | 97 (96–99) | 97 (96–99) | 97 (95–99) | .853 |
| Mild AB, % (N) | 68.3 (307) | 67.5 (272) | 64.8 (278) | 67.9 (331) | .760 |
| Moderate AB, % (N) | 27.2 (122) | 27.8 (112) | 31.7 (135) | 28.1 (137) | |
| Severe AB, % (N) | 4.5 (20) | 4.7 (19) | 3.5 (16) | 3.9 (19) |
AB, acute bronchiolitis; IQR, interquartile range; bpm, breaths per minute.
The described intervention achieved a 84.8% reduction in the use of salbutamol in the ED (95% confidence interval [CI], 79.1%–89.0%; P < .001) and a 98.4% reduction in the use of epinephrine (95% CI, 88.6%–99.8%; P < .001). When it came to the prescription of nebulised salbutamol on discharge, we found a decrease of 92.1% (95% CI, 88.0%–94.8%; P < .001) (Table 3).
Bronchodilator treatment used in the emergency department.
| December 2012 | December 2014 | December 2016 | December 2018 | P value | |
|---|---|---|---|---|---|
| n | 449 | 403 | 429 | 487 | |
| Nebulised epinephrine, n (%) | 58 (12.9) (95% CI, 10.1%–16.3%) | 39 (9.7) (95% CI, 7.2%–13%) | 8 (1.8) (95% CI, 0.9%–3.6%) | 1 (0.2) (95% CI, 0%–1.1%) | <.001 |
| Nebulised salbutamol, n (%) | 230 (51.2) (95% CI, 46.6%–55.8%) | 137 (34.0) (95% CI, 29.5%–38.7%) | 85 (19.8) (95% CI, 16.3%–23.8%) | 38 (7.8) (IC 95%: 5.7%–10.5%) | <.001 |
| Salbutamol on discharge, n (%) | 234 (65.7) (95% CI, 60.6%–70.4%) | 140 (45.4) (95% CI, 39.9%–51.0%) | 81 (23.1) (95% CI, 19.0%–27.8%) | 25 (5.2) (95% CI, 3.4%–7.8%) | <.001 |
CI, confidence interval.
Table 4 summarises the results regarding the effect of the strategy by age (younger or older than 12 months) and severity.
Proportion of use of salbutamol in the emergency department by age and severity.
| Proportion of salbutamol used, % (95% CI), N/N | |||||
|---|---|---|---|---|---|
| December 2012 | December 2014 | December 2016 | December 2018 | P value | |
| Younger than 12 months | |||||
| Mild bronchiolitis | 39.5% (33.7%–45.6%). 102/258 | 23.9% (18.9%–29.7%). 56/234 | 5.4% (3.1%–9.2%). 12/221 | 2.4% (1.1%–4.8%). 7/292 | <.001 |
| Moderate bronchiolitis | 61.4% (51.6%–70.2%). 62/101 | 42.4% (33.1%–52.2%). 42/99 | 24.5% (17.3%–33.5%). 26/106 | 11.7% (7.1%–18.7%). 14/119 | <.001 |
| Severe bronchiolitis | 61.1% (38.6%–79.6%). 11/18 | 29.4% (13.2%–53.1%). 5/17 | 50.0% (26.7%–72.2%). 7/14 | 11.1% (3.1%–32.7%). 2/18 | .003 |
| Older than 12 months | |||||
| Mild bronchiolitis | 65.3% (51.3%–77.0%). 32/49 | 55.3% (39.7%–69.8%). 21/38 | 24.6% (15.2%–37.3%). 14/57 | 17.9% (8.9%–32.6%). 7/39 | <.001 |
| Moderate bronchiolitis | 100%. 21/21 | 84.6% (57.7%–95.6%). 11/13 | 82.8% (65.4%–92.4%). 24/29 | 38.9% (20.3%–61.3%). 7/18 | .002 |
| Severe bronchiolitis | 100%. 2/2 | 100%. 2/2 | 100%. 2/2 | 100%. 1/1 | – |
CI, confidence interval.
As regards patient outcomes, the median length of stay in the ED decreased from 59 min (IQR, 24–99) in 2012 to 25 min (IQR, 15–78) in 2018 (P < .001). In 2012, the rate of hospital admission was 20.7% (95% CI, 17.2%–24,7%), the readmission rate was 16.3% without hospitalisation (95% CI, 12.8%–20.5%) and 4.5% with hospitalisation (95% CI, 2.8%–7.1%). In 2018, the rate of hospitalization was 16.8% (95% CI, 13.7%–20.4%) (P = .045) and the readmission rate was 14.8% without hospitalisation (95% CI, 11.7%–18.6%) and 4.0% with hospitalisation (95% CI, 2.4%–6.3%) (Table 5). The overall rate of hospitalisation documented in the annual report was 4.96% in 2012 (95% CI, 4.86%–5.20%), 5.02% in 2014 (95% CI, 4.87%–5.22%), 4.78% in 2016 (95% CI, 4.63%–4.95%) and 4.83% in 2018 (95% CI, 4.67%–4.99%) (P = .186).
Patient outcomes.
| December 2012 | December 2014 | December 2016 | December 2018 | P value | |
|---|---|---|---|---|---|
| Median care time in Emergency Department, min (IQR) | 59 (24–99) | 60 (24–114) | 26 (15–85) | 25 (15–78) | <.001 |
| Hospitalisation rate, n (%) | 93 (20.7) (95% CI, 17.2%–24.7%) | 95 (23.6) (95% CI, 19.6%–27.9%) | 79 (18.5) (95% CI, 15.0%–22.3%) | 82 (16.8) (95% CI, 13.7%–20.4%) | .045 |
| Rate of readmission within 72 h with hospitalisation, n (%) | 16 (4.5) (95% CI, 2.8%–7.1%) | 20 (6.5) (95% CI, 4.2%–9.8%) | 12 (3.9) (95% CI, 2.3%–6.8%) | 16 (4.0) (95% CI, 2.4%–6.3%) | .372 |
| Rate of readmission within 72 h without hospitalisation, n (%) | 58 (16.3) (95% CI, 12.8%–20.5%) | 40 (13.0) (95% CI, 9.7%–17.2%) | 48 (13.7) (95% CI, 10.5%–17.7%) | 60 (14.8) (95% CI, 11.7%—18.6%) | .940 |
CI, confidence interval; IQR, interquartile range.
Table 6 shows the multivariate analysis of the main outcomes adjusted for age and severity.
Multivariate analysis of the main outcomes adjusted for age and severity of symptoms.
| 2012 | 2014 | 2016 | 2018 | |
|---|---|---|---|---|
| Nebulised epinephrine | Reference | OR 0.63 (95% CI, 0.38–1.06) | OR 0.10 (95% CI, 0.04–0.22) | OR 0.01 (95% CI, 0.00–0.06) |
| Nebulised salbutamol | Reference | OR 0.37 (95% CI, 0.26–0.52) | OR 0.11 (95% CI, 0.07–0.16) | OR 0.04 (95% CI, 0.03–0.07) |
| Salbutamol on discharge | Reference | OR 0.31 (95% CI, 0.21–0.46) | OR 0.07 (95% CI, 0.05–0.11) | OR 0.02 (95% CI, 0.01–0.03) |
| Hospitalisation rate | Reference | OR 1.25 (95% CI, 0.83–1.88) | OR 0.83 (95% CI, 0.55–1.27) | OR 0.41 (95% CI, 0.27–0.63) |
CI, confidence interval; OR, odds ratio.
Maintaining an improvement strategy for 5 years, with progressively restrictive indications for bronchodilator treatment, succeeded in reducing the use of epinephrine and salbutamol below the levels previously published in studies conducted in the ED setting, without increasing length of stay in the ED, the hospitalisation rate or the readmission rate.
We ought to highlight the homogeneity of the patients across the seasons under study in terms of age (similar to that in other studies33,34), clinical parameters, such as respiratory rate and oxygen saturation, and severity.
Prior to the intervention, half the patients received salbutamol at the ED, and salbutamol was prescribed to 2 out of every 3 patients on being discharged home, similarly to what has been reported in other studies.27,33 We managed to decrease its use drastically (<8%), bringing it below the achievable benchmark of care, which Ralston et al, after a systematic review of published quality improvement strategies in hospitalised patients with AB, set at 16%,29 and our own initial target. The maintenance of this strategy over time and more restrictive recommendations succeeded in bringing the use of salbutamol below that threshold, which was not the case when we made the first analysis of the impact of this intervention in 2016.35 There are similar quality improvement strategies described in the literature, but few of them focus on the ED setting. Akenroye et al, with a local protocol introduced in 2011, managed to lower the use of salbutamol from 54% to 47% after a 2-year intervention; they achieved greater success by reducing diagnostic testing.27 Montejo et al describe a coordinated strategy of an ED with primary care centres, which, in the case of the ED, managed to bring the use of salbutamol down to 9.1%, although the use of epinephrine remained unchanged (9%).28 In our study, treatment with salbutamol was reduced both in children younger than 12 months and in the 12- to 24-month age group. If we take account only of patients aged less than 12 months, as is the case in most recent studies, the use of salbutamol in the ED was even lower (5.3%) and the decrease was independent of severity. In the 12- to 24-month age group, a reduction was observed only in mild or moderate bronchiolitis, which was consistent with the results described by Tyler et al.36
Nebulised epinephrine was used primarily in younger patients. The initial situation was similar to that of other EDs.33 In 2012, the CPGs mentioned the possibility of performing a therapeutic test when the evidence was considered equivocal or insufficient.8,9 A reduction in the use of epinephrine towards its total elimination, in accordance with the increasingly restrictive recommendations contained in the protocol, has not been described in any other study.
Healthcare overload, increased waiting times and the decreased availability of observation beds that occurs during the annual epidemic of AB caused by RSV make the length of stay in the ED a particularly important factor. More than half the patients who attended the ED with AB in the last year of the study were discharged in less than 30 min. The decrease in the use of bronchodilators makes it possible to send patients home more quickly, producing a saving not only of material resources but also of human resources.
For the strategy to be successful it is important to show that the hospitalisation and 72-h readmission rates did not increase with the reduction in administration of drugs. In this study, the hospitalisation rate for patients treated for AB not only did not increase, but decreased and stood below the levels described in other studies.37,38 This may be related to an increasing assurance on the part of all the professionals working in the ED in treating this disease, with a reduction in the side effects associated with the medications not being administered,39 as well as with a decrease in the oxygen saturation threshold contained in the protocol to determine the need of hospital admission, which has been gradually reduced from 94% to 91%. This decrease in the hospitalisation rate of patients with AB is not perceptible in the overall rate of admission of the ED.
Given the results of the intervention described, and taking all the available evidence into consideration, perhaps the wisest course is to forget about treatment with bronchodilators once and for all and concentrate efforts on standardising and coordinating care delivery across all levels of care. We must be very cautious in interpreting the modest positive results shown in some studies which continue to analyse various therapeutic interventions together or separately in the interminable search for that subgroup of patients with AB that can benefit from them. The only question to be resolved is the role of high-flow oxygen therapy compared to conventional oxygen therapy outside intensive care units, introduced by many hospitals in recent years despite the lack of solid evidence supporting its use.40 Finally, it is essential to devote the necessary time to explain to parents the expected course of the disease, the absence of effective treatments, the general recommendations and the signs of worsening that they must watch out for at home.
The results of the quality improvement strategy implemented have the following limitations:
- -
The study was conducted in a single centre. Although it might be possible to extrapolate the intervention and the resources underpinning it to other centres, other factors specific to the hospital could have assisted its success.
- -
There could be a long-term trend of reduction in the use of bronchodilators for management of AB that acted independently of the strategy implemented and that could not be assessed due to the lack of a control group. However, there is an extensive literature on the limited effect of CPG recommendations in the absence of other interventions.22,35
- -
Given that the impact of the intervention was only measured in the month corresponding to the peak incidence of the epidemic season, the study did not allow us to evaluate the variability of prescription that may exist in the other months.
- -
Although most of the study variables are objective and easily measurable, in the severity scale objective parameters coexist with subjective ones, and therefore mistakes may be made in interpreting them despite the provided clinical teaching sessions.
- -
With regard to patient outcomes, we cannot guarantee that they did not visit other hospitals and eventually admitted. If this did occur, there is no reason why it should have happened more frequently in one season than in another.
- -
Although the study is powerful enough to estimate the decrease in the use of bronchodilators, it was not designed to estimate the positive effects on the outcomes that were observed, so these must be interpreted with caution.
The future in AB demands that we continue moving forward in reducing the variability of clinical practice and the inappropriate use of therapeutic resources. Given the modest effectiveness of CPGs in changing the usual practice of health care professionals, local quality improvement strategies need to be designed and implemented. To be successful, such interventions must be continued over time, periodically updated, endowed with adequate resources and capable of producing measurable results. In our case, the findings described have served as a starting point for setting in motion the “Doing Nothing Strategy in Bronchiolitis” project, in coordination with all the EDs and primary care centres in the Community of Madrid. Eliminating the use of salbutamol and epinephrine in AB patients is possible.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Andina Martínez D, Escalada Pellitero S, Viaño Nogueira P, Alonso Cadenas JA, Martín Díaz MJ, de la Torre-Espi M, et al. Descenso del uso de broncodilatadores en el manejo de la bronquiolitis tras aplicar iniciativas de mejora. An Pediatr (Barc). 2022;96:476–484.
Meeting Presentation: partial results of the study were presented as an oral communication with the title “Impacto de una estrategia continuada de mejora de la calidad en la atención a los pacientes con bronquiolitis aguda entre 2012 y 2018”at the 24th Meeting of the Sociedad Española de Urgencias de Pediatría; May 11, 2019; Granada, Spain. It was awarded the prize for the best communication on the subject of the conference: “From knowledge and research to clinical practice”.