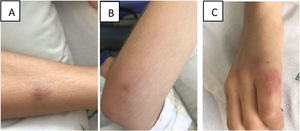
A girl aged 12 years presented with oral aphthae and bilateral cutaneous lesions in the extremities (Figs. 1 and 2) suggestive of vasculitis (Fig. 1A) and pain limiting movement of the lower right extremity of 6 days’s duration.
Evolution of the lesion in the dorsum of the right foot. (A) Active phase. Erythematous plaque with poorly defined borders, warm to the touch, with central purpuric bruise-like component and livedo reticularis, indicative of vasculitis. It was associated with hyperaesthesia and pain on palpation and movement of the foot. In the sole of the same foot, there was a nodule measuring approximately 1×1cm with external signs of inflammation (not featured in image). There was also a plaque measuring approximately 5×3cm extending from the lower third of the left leg to the lateral malleolus, indurated, with poorly defined borders, warm to the touch and painful on palpation (not featured in image). (B) Lesion in remission. Erythema in the dorsum of the foot and residual allodynia. Resolution of the purpuric component and livedo reticularis. (C) and (D) Evolution of the nodular lesion in the 2nd finger of the right hand.
The only relevant history was an episode of streptococcal pharyngitis 3 weeks prior, and erythema nodosum was initially suspected. Given the severity of the pain, which could only be alleviated with morphine, the location of the lesions and the presence of livedo reticularis, a lesion biopsy specimen was obtained, revealing vascular wall necrosis and thrombosis in medium-sized vessels, compatible with polyarteritis nodosa (PAN). The CT angiogram of the chest and abdomen angio-TC toraco-abdominal, acute phase reactants, autoimmune testing (including antineutrophil cytoplasmic and antiphospholipid antibodies) and serologic tests for infection were all normal.
The patient received a diagnosis of cutaneous PAN (cPAN) and started treatment with prednisone (2mg/kg/day). She had a partial response, leading to addition of intravenous immunoglobulin (IVIG, at a dose of 2g/kg over 48h) and colchicine. This achieved an excellent outcome. It allowed discontinuation of steroid therapy within 2 months and colchicine at 1year, without recurrence. The only remaining sequela is hyperaesthesia in the dorsum of the foot.
Cutaneous PAN is a necrotising vasculitis involving medium-sized vessels1–3 that is frequently preceded by streptococcal pharyngitis1,2 of which fewer than 100 cases have been described in the paediatric population.2
Its natural history consists in recurrent attacks characterised by the development of painful subcutaneous nodules in the extremities, occasionally with fever, articular involvement, peripheral neuropathy or myalgia.3 The prognosis is good, and progression to systemic disease is extremely rare.1–3 The most frequently used treatments are steroid therapy, colchicine, IVIG, methotrexate, mycophenolate and azathioprine,2 although there are no studies demonstrating their efficacy.
In conclusion, cPAN is a form of vasculitis that is infrequent in the paediatric age group and that should be considered in the diagnosis of cutaneous nodules with atypical localization or associated with livedo reticularis. The diagnosis is confirmed by histopathology,1,2 and there are various treatment options that may be useful.