Congenital left ventricular outflow tract obstruction that is symptomatic or associated with ventricular dysfunction is an indication for surgery in the paediatric population. When the obstruction is at the level of the aortic valve, the Ross procedure (pulmonary autograft) is the approach of choice. When the obstruction is found at several levels, the gold standard is the Ross-Konno procedure (pulmonary autograft combined with ventriculoseptoplasty). Both techniques have shown to provide excellent haemodynamic outcomes and potential for growth.1
However, none of these alternatives can be considered a definitive solution when the problem arises in neonates or infants.2,3 Outcomes in the medium to long term show a substantial number of reinterventions, both percutaneous and surgical. When both sides of the heart are involved, treatment becomes very complex.
A new possibility for these patients has recently emerged with the description of the Ozaki technique4 (complete aortic valve reconstruction using pericardial tissue). To be able to make meaningful comparisons in the future, the outcomes of techniques currently in use need to be analysed first. For this reason, we report our experience in the last decade using the gold standard techniques.
A total of 21 procedures (6 Ross/15 Ross–Konno) were performed between 2008–2019. Two in-hospital deaths were documented, both in the Ross–Konno group and caused by a failed aortic valvuloplasty in the neonatal period. Both of these patients required postoperative extracorporeal membrane oxygenation (ECMO). One of these patients was successfully weaned out, but later developed necrotising enterocolitis. The median aortic annulus diameter and age of surgery was significantly lower in the Ross-Konno group compared to the Ross group: 12 mm (interquartile range [IQR], 5.6–17) versus 17.5 mm (IQR, 15–19) and 60 months (IQR, 4–115) versus 97.5 months (IQR, 84–144). The number of previous surgeries and the hours of mechanical ventilation were significantly greater in the Ross–Konno group (Table 1).
Preoperative variables.
| Preoperative variables | Ross (n = 6) | Ross–Konno (n = 15) | P |
|---|---|---|---|
| Age in months, median (IQR) | 97.5 (84−144) | 60 (4−115) | .10 |
| Weight in kg, median (IQR) | 27 (18.5−38.7) | 15 (4,7−27) | .094 |
| Height in cm, median (IQR) | 124.5 (115−153) | 112 (55−138) | .14 |
| Number of previous surgeries | .027 | ||
| 0 | 5 | 3 | |
| 1 | 0 | 6 | |
| 2 | 1 | 6 | |
| Number of previous percutaneous procedures: | |||
| 0 | |||
| 1 | 3 | 9 | .37 |
| 2 | 3 | 2 | |
| 3 | 0 | 3 | |
| 0 | 1 | ||
| Aortic annulus diameter in mm, median (IQR) | 17.5 (15−19) | 12 (5.6−17) | .023 |
| Peak aortic pressure gradient in mmHg, median (IQR) | 55 (21−70) | 90 (70−115) | .035 |
| Mean aortic pressure gradient in mmHg, median (IQR) | 31 (13−45) | 48 (36−64) | .067 |
| Indication for surgery | |||
| Aortic stenosis | 2 | 4 | .26 |
| Aortic insufficiency | 1 | 0 | |
| Double aortic lesion | 3 | 11 |
There were no losses to follow-up, with a median duration of follow-up of 6.2 years (IQR, 5.9–6.5) in the Ross group versus 5.3 years (IQR, 3.6–7.2) in Ross–Konno group. There were 2 deaths, both associated with surgical reintervention. In 1 case, reintervention consisted of a right ventricle to pulmonary artery (RV-PA) conduit replacement with tricuspid valvuloplasty in a patient that had undergone the Ross–Konno procedure 9 years before. Before the surgery, the right ventricle was severely compromised, and the patient died 2 months post surgery due to multiple organ failure. In the second case, the death was not related to the Ross–Konno surgery, but resulted from thrombosis of a mechanical mitral valve prosthesis. This patient had hypoplastic left heart complex with a history of 5 prior surgeries, and had undergone the Ross–Konno procedure 7 months before the development of the valve thrombosis.
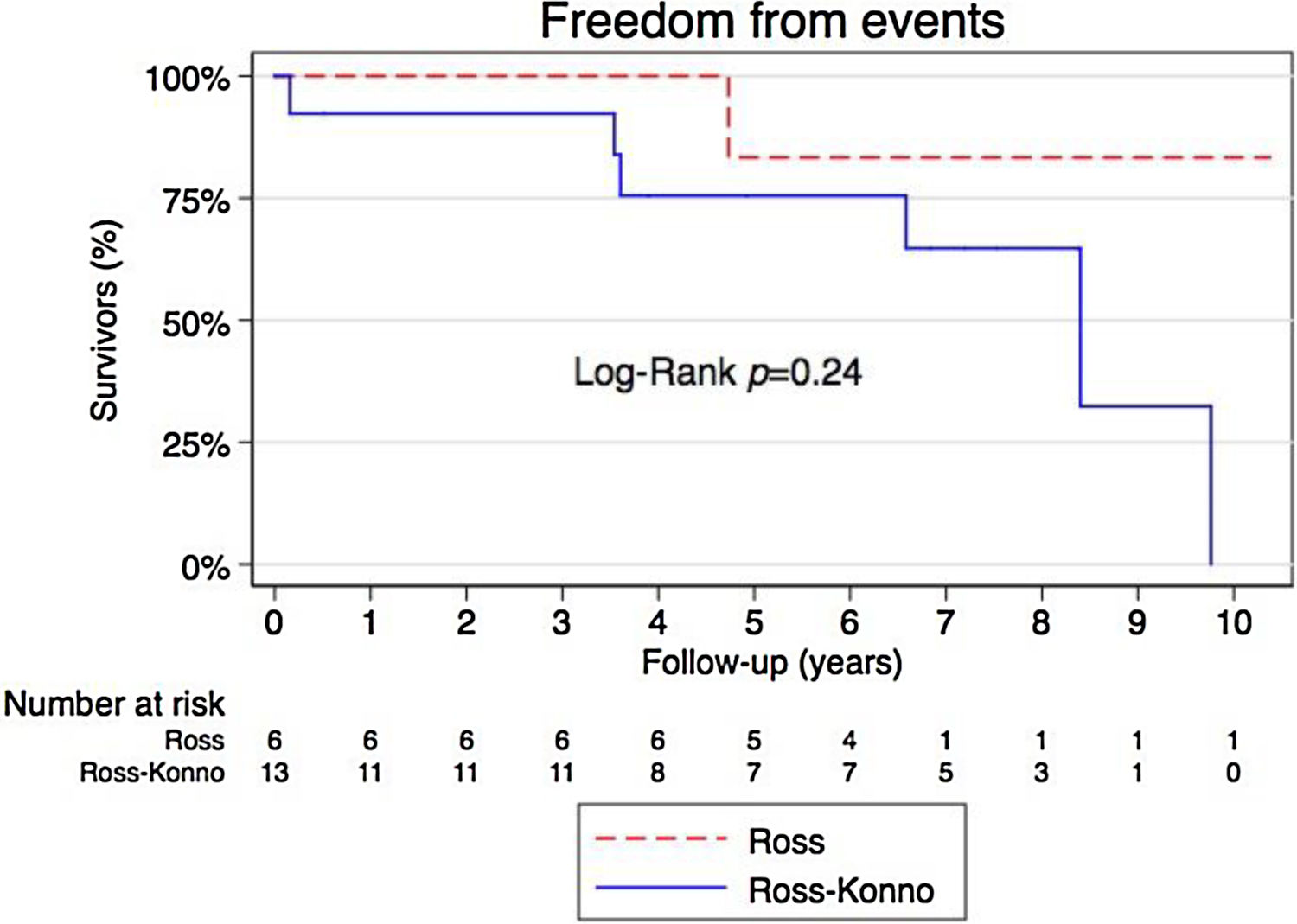
The 3-, 5- and 7-year event-free survival was 100%, 83% and 83%, respectively, in the Ross group and 92%, 76% and 65%, respectively, in the Ross–Konno group, with no statistically significant differences between groups (Fig. 1).
During the follow-up, 7 patients (37%) needed some form of reintervention (surgical and/or percutaneous): 1 in the Ross group (17%) and 6 in the Ross–Konno group (46%). Most of the reinterventions were related to RV-PA conduit dysfunction.
The late haemodynamic outcomes are good, especially the outcomes of autografts, none of which required reintervention on the aortic valve or the autograft. All patients had mild or no residual aortic regurgitation (AR), except 2 patients in the Ross group (33%), 1 with moderate AR and 1 with severe AR, but both with good left ventricular function, and 1 patient with severe AR in the Ross–Konno group that also had good left ventricular function. As for the right heart, all survivors had mild or no pulmonary regurgitation (PR), except 2 patients in the Ross–Konno group that had severe PR but good RV function, and 1 patient in the Ross group and 1 in the Ross-Konno group with moderate PR.
There are considerable limitations to our study due to its retrospective design and small sample size. However, we believe that our findings are relevant, as there are few reports of the medium- and long-term outcomes of these procedures in the paediatric age group. We believe that sharing our results provides information on clinical experiences that may contribute to a better understanding of this disease.
In conclusion, due to the complex nature of these procedures, postoperative complications are frequent. They achieve good solutions for the left ventricle outflow tract obstructions in the medium-to-long term, but at the expense of multiple RV-PA conduit reinterventions. The experience with the Ozaki technique is still limited to 4.5 years, but it is less aggressive, as it does not require manipulation of the right side of the heart (the pulmonary autograft is not needed).5,6 The initial experience in 6 patients with a 15-month follow-up shows promising results. Only time will tell whether this new technique will replace the current gold standard.
Please cite this article as: Aroca Á, Polo L, Ramchandani B, Sánchez R, González Á. Perspectivas actuales en el procedimiento de Ross y Ross-Konno: ¿es hora de buscar alternativas? An Pediatr (Barc). 2022;96:365–367.
This study was presented at the XXV National Congress of the Sociedad Española de Cirugia Cardiovascular y Endovascular, held online between October 14–17, 2020.