Several studies have suggested that the hospitalization rate for COVID-19 in children and adolescents may reflect the prevalence of the infection rather than the severity of the disease. The aim of this study was to describe the clinical features of hospitalised paediatric patients with SARS-CoV-2 infection in order to understand if the infection was the reason for admission.
MethodsRetrospective cohort study including patients aged 0–18 years with SARS-CoV-2 infection or multisystem inflammatory syndrome in children (MIS-C) admitted to a tertiary care children’s hospital in Spain between 01/01/2020 and 12/31/2021.
Results228 patients were included, corresponding to 150 cases of COVID-related admission (SARS-CoV-2 infection as main cause of hospitalization) and 78 of non-COVID-related admission (SARS-CoV-2 infection unrelated to the hospitalization).
In the group of COVID-related admissions, 58 patients had comorbidities. Forty-nine patients had acute respiratory disease (pneumonia, bronchospasm or bronchiolitis). Multisystem inflammatory syndrome in children was diagnosed in 27 and was significantly more frequent in the first year of the pandemic (wild type virus). Eighty percent of patients with acute respiratory disease needed respiratory support, mostly low-flow oxygen therapy. The severity of the disease was similar in all virus variants. Two patients (both with severe comorbidities) died from COVID-related conditions.
ConclusionsIn our study, one third of the patients were admitted with SARS-CoV-2 infection but not because of it. Acute respiratory disease was less frequent and had a better prognosis compared to the adult population, while MIS-C was a major cause of morbidity and hospitalization. The fatality rate was extremely low.
Varios estudios han sugerido que la tasa de hospitalización por COVID-19 en niños y adolescentes puede reflejar la prevalencia de la infección más que la gravedad de la enfermedad. El objetivo de este estudio fue describir las características clínicas de pacientes pediátricos hospitalizados con infección por SARS-CoV-2, con el fin de comprender si este fue el principal motivo de ingreso.
MétodosEstudio de cohortes retrospectivo que incluyó a pacientes de 0 a 18 años con infección por SARS-CoV-2 o síndrome inflamatorio multisistémico pediátrico vinculado a SARS-CoV-2 (SIM-PedS), ingresados en un hospital infantil de tercer nivel en España entre el 01/01/2020 y el 31/12/2021.
ResultadosSe incluyeron 228 pacientes: 150 fueron ingresos causados por COVID (infección por SARS-CoV-2 como principal causa de hospitalización) y 78 fueron ingresos no causados por COVID (infección por SARS-CoV-2 no relacionada con la hospitalización). Entre los ingresos causados por COVID, 58 pacientes tenían comorbilidades. 49 pacientes cursaron con enfermedad respiratoria aguda (neumonía, broncoespasmo o bronquiolitis). 27 pacientes fueron diagnosticados de SIM-PedS; este diagnóstico se observó con más frecuencia durante el primer año de la pandemia (variante wild type). El 80% de los pacientes con enfermedad respiratoria aguda necesitaron algún tipo de soporte respiratorio, principalmente oxígeno de bajo flujo. La gravedad de la enfermedad fue similar con todas las variantes del virus. Dos pacientes (ambos con comorbilidades graves) fallecieron por afecciones relacionadas con la COVID-19.
ConclusionesEn nuestro estudio, un tercio de los pacientes fueron hospitalizados con infección por SARS-CoV-2 pero no a causa de ella. La enfermedad respiratoria aguda tuvo menos incidencia y mejor pronóstico que en la población adulta, mientras que el SIM-PedS fue una causa importante de morbilidad y hospitalización. La mortalidad fue extremadamente baja.
Several studies have suggested that SARS-CoV-2 infection in the paediatric population is less prevalent and less contagious than in adults. The disease presentation also appears to be less severe in children, with a higher percentage of asymptomatic and mild cases.1–4 Severe acute COVID-19 forms have been found to be more common in adolescents and patients with comorbidities.5–8 On the other hand, multisystem inflammatory syndrome in children (MIS-C) has been described as an important cause of hospitalization and mortality.9–12
In general, paediatric hospitalization rates reported in western countries were low during the pandemic,2,3,8,13,14 except for a notable increase during the omicron wave (B.1.1.529 variant). In the United States, in early 2022, the COVID-19 hospitalization rate in children aged 0–4 years increased up to five times compared to what had been reported in previous months. These data raised concern about the impact of the new variants on the paediatric population, although it was also justified by the fact that this population was the only age group not yet eligible for vaccination at that time.15 In Spain, the first vaccination campaign against SARS-CoV-2 for the population aged 16 and 29 years began on June 30, 2021. The vaccination of children aged 12–15 started on August 4, 2021, and the vaccination of children aged 5–11 years started on December 15, 2021.
Since admitted patients were routinely screened for SARS-CoV-2 infection, some researchers have suggested that the hospitalization rate in children may reflect the prevalence of infection in the community rather than the actual severity of the illness. This would lead to overestimation of the cases requiring hospitalization.14
The aim of our study was to describe the clinical features of paediatric patients admitted with confirmed SARS-CoV-2 infection during the first 2 years of the pandemic in order to determine whether SARS-CoV-2 infection was the main reason for admission. A better understanding of the impact of COVID-19 in children may be helpful to assess public health decisions.
Patients and methodsPatients and settingWe conducted a retrospective cohort study that included patients aged 0–18 years with a diagnosis of SARS-CoV-2 acute infection or MIS-C admitted between January 1, 2020 and December 31, 2021 to a tertiary care children’s hospital in Spain.
The diagnosis of acute infection was made either by detection of SARS-CoV-2 RNA via real-time reverse transcriptase polymerase chain reaction (RT-PCR) in throat swab (TS), nasopharyngeal aspirate (NPA) or saliva samples, or by detection of SARS-CoV-2 antigen in NPA, according to the hospital protocol at the time of admission. The diagnosis of MIS-C was made by applying the WHO classification criteria, which includes, apart from a compatible clinical history and laboratory findings, the evidence of previous SARS-CoV-2 infection (by RT-PCR, antigen test or positive serology with anti-SARS spike antibody [Abbott]) or a known history of contact with a patient with COVID-19.10
We excluded patients readmitted within 90 days with a positive RT-PCR due to the known period of persistent viral shedding, with the exception of immunocompromised patients readmitted with respiratory symptoms and with a positive antigen test, which were considered cases of acute infection.16–18
It is important that we highlight that both the criteria for testing for SARS-CoV-2 infection and the diagnostic methods varied greatly during the study period. At the beginning of the pandemic, due to the scarcity of tests, the RT-PCR test was only used in patients with suspected infection.19,20 From June 2020, routine screening was performed in all admitted patients (which including patients admitted to the child and adolescent psychiatry unit). Following the marketing authorisation of rapid antigenic tests (Roche Laboratories), patients aged more than 1 year with respiratory symptoms lasting 5–10 days were tested with them, while all other patients were assessed with the RT-PCR test.
VariablesWe reviewed the health records of the selected patients to obtain information on pre-existing medical conditions, the course of disease, imaging features, laboratory and microbiological findings, received treatment and outcomes.
We classified cases as: COVID-19 as the cause of hospitalization (COVID-related admission) and COVID-19 as current infection not related to the hospitalization (non-COVID-related admission).
We classified cases in which SARS-CoV-2 infection was the main reason for admission (direct cause) or in which we considered that the patient would not have needed hospital admission if it were not for the infection (indirect cause) as COVID-related admissions. It would be the case of acute respiratory diseases (bronchiolitis, bronchospasm, pneumonia); MIS-C; observational admission in at-risk patients and febrile infants with neutropenia in whom no other infection was documented. The clinical phenotype of COVID-related admission patients was compared in different periods in relation to the predominant variants (>50% of random samples) in our setting: wild type (March 2020–January 2021), alpha (February 2021–May 2021), delta (June 2021–November 2021), and omicron (December 2021–April 2022).21,22 We ought to underscore that the study period ended on December 31, at the very beginning of the omicron wave.
On the other hand, non-COVID-related admission patients were those who had been admitted for other reasons and tested positive in the screening at admission. Uncertain cases were discussed among researchers until a consensus was reached.
As regards coinfection, patients aged 0–4 years with respiratory symptoms underwent routine testing at admission for respiratory syncytial virus (RSV) and influenza A/B during the epidemic season in addition to the screening for SARS-CoV-2, with tests conducted on TS/NPA samples (Xpert® Xpress CoV-2/Flu/RSV plus-Respiratory [Cepheid] or Allplex™ SARS-CoV-2/FluA/FluB/RSV Assay [Seegene Inc]). Real-time PCR testing for multiple respiratory viruses (BIOFIRE Respiratory 2.1 plus [RP2.1plus] panel [Biomerieux] or QIAstat-Dx Respiratory SARS-CoV-2 panel [Qiagen]) in NPA or tracheal aspirate (TA) samples, in addition to cultures, were performed in all patients admitted to the paediatric intensive care unit (PICU) due to respiratory complications and additional select patients with respiratory comorbidities.
Blood cultures were performed in cases of sepsis or fever and general health deterioration.
When it came to the specific treatment for COVID-19, the guidelines varied considerably over the study period.
All high-risk patients admitted for observation, diagnosed with acute respiratory disease or MIS-C or admitted to the PICU remained in follow-up in the hospital outpatient clinics for at least 3 months after discharge. The rest of the patients were referred for follow-up by their primary care paediatrician.
Statistical analysis and ethical considerationsWe made a descriptive analysis, expressing results in terms of median and interquartile range (IQR) or proportions, as applicable. We compared categorical variables with the χ2 and Fisher exact tests and considered P values of less than 0.05 indicative of a statistically significant difference. The statistical analysis was performed with the software Stata, version 15.1.
The study adhered to the principles of the Declaration of Helsinki declaration and was approved by the ethics committee of the hospital (PIC-90-22). Due to the large number of patients in the sample and the lack of experimental activity, the committee approved an exemption to the informed consent requirement. We entered the patient data into a database located in a protected folder on the hospital intranet, and the data was encoded by professionals independent from the research team to safeguard patient privacy.
ResultsDuring the study period, 201 patients with confirmed SARS-CoV-2 infection and 27 patients with MIS-C were admitted to the hospital. Of this total, 129 (56%) were male.
One hundred and fifty patients (66%) were classified as COVID-related admissions and 78 (34%) as non-COVID-related admissions. The median age in these groups was 6 years (IQR, 0.1–13.9) and 8 years (IQR, 0.6–14.5), respectively.
Due to the timing of SARS-CoV-2 vaccination, only 4 of the patients in the sample had received a complete 2-dose vaccination series before admission.
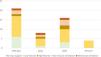
Fig. 1 presents the frequency of admission in relation to the predominant SARS-CoV-2 predominant variants.
COVID-related admissionsIn the COVID-related admission group, 58 (39%) of the patients had one or more comorbidities. The most frequent were asthma, obesity, neurological diseases, lung diseases and immunodeficiencies. (Table 1).
Comorbidities and diagnosis at discharge in COVID-related admission patients.
| COVID-related admissions (n = 150) | |
|---|---|
| Comorbidities | n (%) |
| Preterm birth ≤ 34 weeks of gestation | 3 (2%) |
| Recurrent wheezing | 5 (3.3%) |
| Asthma | 12 (8%) |
| Other pulmonary disease | 8 (5.3%) |
| Sleep apnoea syndrome | 3 (2%) |
| Bronchiectasis | 2 (1.3%) |
| Chronic aspiration syndrome secondary to neurologic disease | 2 (1.3%) |
| Bronchopulmonary dysplasia | 1 (0.6%) |
| Cerebral palsy | 4 (2.6%) |
| Neuromuscular disorder | 2 (1.3%) |
| Down syndrome | 2 (1.3%) |
| Other neurologic disorder | 14 (9%) |
| Congenital heart disease | 4 (2.6%) |
| Immunodeficiencies | 8 (5.3%) |
| Secondary | 5 (3.3%) |
| Primary (myelodysplastic syndrome) | 1 (0.6%) |
| Primary (MYD88 deficiency) | 1 (0.6%) |
| Primary (congenital asplenia) | 1 (0.6%) |
| Diabetes mellitus | 2 (1.3%) |
| Obesity/overweight | 12 (8%) |
| Other metabolic disorder | 4 (2.6%) |
| Glutaric aciduria type 1 | 2 (1.3%) |
| Hypothyroidism | 1 (0.6%) |
| Ornithine carbamoyltransferase deficiency OTC (NM_000531.5) | 1 (0.6%) |
| Nephropathy | 3 (2%) |
| Sickle cell anaemia | 2 (1.3%) |
| Other diseases | 29 (19%) |
| COVID-related admissions (n = 150) | |
|---|---|
| Diagnosis at discharge | n (%) |
| Pneumonia | 34 (23%) |
| Febrile infants younger than 3 months | 32 (21%) |
| MIS-C | 27 (18%) |
| Observational admission in high-risk patients | 20 (13%) |
| Bronchiolitis | 6 (4%) |
| Bronchospasm | 6 (4%) |
| Febrile neutropenia | 6 (4%) |
| Gastrointestinal symptoms requiring IV rehydration | 6 (4%) |
| Bronchopneumonia | 3 (2%) |
| Other diagnosis: | 10 (7%) |
| Decreased appetite | 2 (1.3%) |
| Epileptic status | 1 (0.6%) |
| Infant apnoea | 1 (0.6%) |
| Croup | 1 (0.6%) |
| Dyspnoea (without pneumonia) | 1 (0.6%) |
| Congenital heart disease decompensation | 1 (0.6%) |
| Cholestatic hepatitis (patient with metabolic disorder) | 1 (0.6%) |
| Encephalitis | 1 (0.6%) |
| Thrombocytopenia (exacerbation of chronic immune thrombocytopenia) | 1 (0.6%) |
The most common diagnosis at discharge was pneumonia (23%), followed by febrile illness in an infant aged less than 3 months (21%), MIS-C (18%) and observational admission in high-risk patients (13%) (Table 1).
MIS-C was more frequently observed during the wild type SARS-CoV-2 period, while acute respiratory disease and other diagnosis (including gastrointestinal manifestations) were more frequently observed during the delta variant period (Fig. 2). These differences were statistically significant (P = .012) (Table 2).
Diagnosis at discharge in COVID-related admissions, by groups and by variants.
| Acute respiratory disease | MIS-C | Observational admission | Other causes of admission | Total | |
|---|---|---|---|---|---|
| Wild type | 21 | 21 | 13 | 22 | 77 |
| Alpha | 8 | 3 | 3 | 3 | 17 |
| Delta | 16 | 2 | 2 | 21 | 42 |
| Omicron | 4 | 0(*) | 2 | 8 | 14 |
| Pearson χ2(9) = 21.2491 P = .012 | |||||
Of the 150 patients with COVID-related admissions, 24 (16%) required transfer to the PICU: 13 (54%) had MIS-C and needed vasoactive support, 10 (42%) had acute respiratory disease and requiring more aggressive respiratory support, and 1 (4%) had encephalitis requiring close monitoring and observation.
The percentage of patients with acute respiratory disease who required admission to the PICU was 20% (n = 10), while the percentage of the patients with MIS-C who required admission to the PICU was 48% (n = 13).
We classified 123 cases based on severity (excluding the 27 MIS-C cases out of the total 150 to avoid bias leading to overestimation of severity). Eighty three (68%) were classified as mild (no need of respiratory support), 27 (22%) as moderate (need of supplemental low-flow oxygen therapy [LFOT]), 4 (3%) as severe (need of supplemental high-flow oxygen therapy) and 9 (7%) as critical (need of non-invasive ventilation [NIV] or mechanical ventilation [MV]).
A separate analysis of the 49 patients with acute respiratory disease revealed that 39 (79%) needed some kind or respiratory support, chiefly LFOT (Fig. 3). The severity of disease did not vary significantly between the periods corresponding to different variants, although the 4 patients with acute respiratory disease during the omicron wave only received LFOT.
None of the patients in our study needed extracorporeal membrane oxygenation support (ECMO).
Table 3 summarises the information on the specific treatment for COVID-19.
COVID-specific treatment administered to patients with COVID-related admissions.
| Treatment | n (%) |
|---|---|
| Azithromycin | 11 (7%) |
| Corticosteroids | 51 (34%) |
| Remdesivir | 4 (2.6%) |
| Tocilizumab | 4 (2.6%) |
| Tocilizumab + other monoclonal antibodies (Siltuximab, Anakinra) | 1 (0.6%) |
| Intravenous immunoglobulins | 26 (17%) |
| Heparin | 41 (27%) |
Table 4 presents the data concerning coinfection. Bacterial coinfection was detected in 3 cases and viral coinfection in another 6 cases; among the latter, the most frequently isolated pathogen was rhinovirus/enterovirus. Five patients (83% of the patients with viral coinfection) required some type of respiratory support, of who 2 (33%) required PICU admission and NIV/MV. We did not find statistically significant differences in severity (need of respiratory support or PICU admission).
Bacterial and viral coinfections in COVID-related admission patients.
| Microorganism | Sample | n |
|---|---|---|
| Bacterial coinfection | ||
| S maltophilia | Tracheal aspirate (culture) | 1 |
| K pneumoniae | Urine culture | 1 |
| S hominis | Blood culture | 1 |
| Viral coinfection | ||
| RSV | Nasopharyngeal aspirate | 2 |
| Rhino/enterovirus | Nasopharyngeal aspirate | 3 |
| Rhino/enterovirus, influenza B, parainfluenza | Bronchoalveolar lavage (BAL) | 1 |
Two patients died from COVID-related conditions, both of who had multiple comorbidities. The first patient was a 12-year-old boy with acute lymphoblastic leukaemia who had received chimeric antigen receptor T-cell (CAR-T) therapy and undergone allogeneic hematopoietic stem cell transplantation complicated by acute and chronic graft-versus-host disease. The second patient was an 8-year-old boy with a history of extremely preterm birth, severe cerebral palsy, epilepsy and recurrent respiratory infections.
One patient reported persistent COVID-19 symptoms (long COVID) during the follow-up. It was a boy aged 14 years who had been admitted to the PICU due to MIS-C and reported persistent dizziness and fatigue for 6 months after the admission.
Three patients were found to have long-term sequelae: one had long-term neurological impairment secondary to encephalitis and the other two developed coronary aneurysms after having MIS-C.
Finally, we ought to mention that 2 patients had had a previous SARS-CoV-2 infection, although the symptoms had been mild and had not required hospitalization.
Non-COVID-related admissionsIn the study, 78 (34%) patients were classified as non-COVID-related admissions. Table 5 details the diagnoses that led to their admissions. In most of these patients, the SARS-CoV-2 infection was completely asymptomatic, and only 26 (33%) were oligosymptomatic (mild cold symptoms). None required any form respiratory support.
Diagnosis at discharge of patients with non-COVID-related admissions.
| Non-COVID-related admissions (n = 78) | |
|---|---|
| Diagnosis | n (%) |
| Urinary tract infection | 12 (15%) |
| Psychiatric disorder | 11 (14%) |
| Appendicitis | 8 (10%) |
| Other surgical problems | 8 (10%) |
| Fracture or traumatic injury | 6 (8%) |
| Cutaneous or dental infection | 6 (8%) |
| Oncological or haematologic disease | 4 (5%) |
| Diabetes mellitus | 2 (3%) |
| Newborn delivered to SARS-CoV-2 positive mother | 2 (3%) |
| Other diagnosis | 19 (24%) |
Of all the children admitted with a SARS-CoV-2 infection during the study period, 34% were not admitted because of COVID-19 as a direct or indirect cause, illustrating that the hospitalization rate for SARS-CoV-2 infection in the paediatric population is probably overestimated. Other authors have analysed this aspect in the past, like Kushner et al.,14 who found that 45% of admissions were classified as unlikely to be caused by SARS-CoV-2. This percentage was slightly higher than the one found in our sample.
Separating and analysing these two groups is important to correctly define the impact of the disease in the paediatric population. Cases considered COVID-related admissions were classified as such because the infection was the primary reason for the admission, but most of these patients did not develop severe COVID. This was the case, for example, of patients with mild symptoms but with underlying disease (high-risk patients) admitted for observation and preventive treatment with remdesivir; or of febrile infants aged less than 3 months in whom no infection other than SARS-CoV-2 could be detected. The latter scenario is a challenge for clinicians in primary care level and emergency care settings, and algorithms have been proposed to better identify children at high risk of bacterial infection.23
Clinical features of COVID-related admissionsUnlike in adults, only one third of COVID-related admissions in children were due to acute respiratory disease, which was also less severe.24–27 It is worth noting that among these patients, pneumonia was the most common diagnosis at discharge (34 patients; 23%), while only 6 (4%) had bronchiolitis, 6 (4%) bronchospasm and another 3 (2%) bronchopneumonia. This confirms the previous reports in the literature about the extremely low incidence of bronchiolitis among infants with SARS-CoV-2 infections.1,28 Pneumonia was more frequent in adolescents, as previously described in both the literature and a previous case review in our hospital.29
In our study, MIS-C was an important cause of COVID-related admission, a form that, while not an acute presentation of SARS-CoV-2 infection, is associated with the greatest severity and morbidity in the paediatric population.11,12,30 The percentage of patients requiring admission to the PICU was higher in patients with MIS-C compared to patients with acute respiratory disease. These results were consistent with the results described by the EPICO-AEP working group for the Spanish cohort.9
The case fatality rate was 4% in patients with acute respiratory disease and 0.9% in the overall group of paediatric patients admitted with COVID-19, which was consistent with the previous literature.2,4,31 The presence of pre-existing comorbidities has been found to be directly correlated to an increased mortality in paediatric patients.32 In our study, the 2 patients who died of COVID-19 had severe comorbidities.
Changes in clinical features during the pandemicIn our study, as previously described,22,33 MIS-C was more frequent in the period that the wild type virus was most prevalent, while acute respiratory disease and other presentations (including gastrointestinal symptoms) were more frequent during the delta variant wave; these differences were statistically significant.
Regarding the severity of the disease, several studies have suggested that the omicron variant is associated with a milder clinical course.24,34 In our study, we did not find significant differences in disease severity between the different periods, probably due to the low number of patients included in the omicron period.
Notwithstanding, our results are similar to those of some previous studies,13,14,31 suggesting that they could be representative of the real impact of SARS-CoV-2 in the paediatric population of western countries.
When it comes to the 2 patients who experienced reinfection, it can be hypothesized (although it could not be conclusively proven in our study) that a different degree of disease severity is associated with each SARS-CoV-2 variant and, furthermore, that the immunity granted by the infection does not guarantee 100% protection against reinfection, which may even be more severe.
CoinfectionsIn our study, coinfection with RSV was not common. One retrospective study conducted in 32 children aged less than 24 months admitted with respiratory compromise due to COVID-19 found that 18.7% had RSV coinfection.35 We found a much lower incidence of coinfection, although the real incidence could be underestimated because we did not perform the test in all patients. However, coinfection by SARS-CoV-2 and RSV was probably uncommon. In this regard, it has also been described that the COVID-19 pandemic has affected the epidemiological trends of acute bronchiolitis, with a noticeable decline in the incidence of bronchiolitis caused by RSV compared to previous years.36 It would be interesting to analyse the epidemiological changes in all respiratory diseases that require admission, comparing what was observed during the pandemic with previous years.
LimitationsOur study is limited by its retrospective and single-centre design. Our centre is a referral centre for many paediatric diseases, which may have been a source of bias in relation to the prevalence of comorbidities, especially in patients with chronic complex illnesses.
As we mentioned earlier, there was significant variation in the screening and diagnostic protocols during the study period, which may have been an important source of bias, especially in terms of overestimating the incidence of severe COVID-19 in the first months of the study (due to the scarcity of tests) and underestimating the prevalence of viral coinfections in patients with acute respiratory diseases due to lack of routine screening for coinfection.
Our decision to include observational admissions of high-risk patients in the COVID-related admissions group, even though they did not ultimately have a severe course of disease, may have skewed the perceived impact of the infection on this group.
Since not all patients included in the study (COVID-related as well as non-COVID-related cases) were followed up at the hospital, we may have underestimated the frequency of long COVID.
Finally, the time of the study (finishing December, 31th, 2021) makes difficult to evaluate the impact of the Omicron variant.
ConclusionOur study confirmed that the clinical significance of SARS-CoV-2 infection in children is different compared to adults. In up to one third of the patients, SARS-CoV-2 infection was diagnosed solely due to the routine screening, and a majority remained asymptomatic. The fatality rate was extremely low and was associated with the presence of underlying comorbidities.
Contrary to the adult population, the incidence of acute respiratory diseases was much lower and the prognosis was generally favourable. Pneumonia was more frequent in adolescents. The incidence of bronchiolitis was very low and RSV coinfection was uncommon. On the other hand, bronchospasm related to SARS-CoV-2 infection was observed in children with a history of recurrent wheezing/asthma.
MIS-C was one of the main causes of COVID-related admissions and morbidity.
The clinical phenotype of SARS-CoV-2 infections varied depending on the predominant variant, but we did not detect any changes in severity.
Last of all, we conclude that the hospitalization rate for SARS-CoV-2 infection in children and adolescents has probably been overestimated, since one third of the patients in our study were admitted with COVID-19 and not because of COVID-19.
FundingThis study received no funding.
Conflict of interestsThe authors have no conflict interests to disclose.
We thank our colleagues in the inpatient care team, especially Maria Melé-Casas, Gemma Pons-Tomàs and Juan José García-García. We also thank Carmen Muñoz-Almagro, for her contribution from a microbiological perspective.
Previous meeting: This study was presented the Seventh Annual Meeting of the Sociedad Española de Pediatría Interna Hospitalaria (SEPIH), October 21–22, 2022, Hospital Gregorio Marañón, Madrid, Spain.