Inflammatory bowel disease (IBD) is a multisystemic disease in which 30% of affected patients develop some type of extraintestinal manifestation (EIM). Extraintestinal manifestations may emerge at different stages during the disease, and may or may not be associated to the level of activity.1,2
Among the haematologic manifestations of IBD is primary immune thrombocytopenia (PIT), formerly known as idiopathic thrombocytopenic purpura. It is characterised by an isolated platelet count less than 100000/mm3 in the absence of an initiating cause. It is diagnosed by the exclusion of other causes in patients with persistent thrombocytopenia (Table 1).1,3,4
Causes of secondary PIT and thrombocytopenia.
| Non-immune mechanism | Immune mechanism |
|---|---|
| Congenital thrombocytopenias, Bernard-Soulier syndrome, von Willebrand disease type IIb, MYH9-related disorders | Post-transfusion purpura and alloimmune thrombocytopenia |
| Bone marrow diseases: myelodysplastic syndromes, leukaemias, aplastic anaemia, bone marrow infiltration | Drug-induced immune thrombocytopeniaRecent vaccinationInfection by HIV, HCV. Other infections |
| Thrombotic thrombocytopenic purpura and other thrombotic microangiopathies | Association with other autoimmune diseases: lupus erythematosus, antiphospholipid syndrome, inflammatory bowel disease and thyroid disorders, among others |
| Chronic liver disease | Association with common variable immunodeficiency and autoimmune lymphoproliferative syndrome |
| Drug use (alcohol among others), natural medicine products and environmental toxins | Thrombocytopenia following haematopoietic stem cell or solid organ transplant |
| Drug-induced thrombocytopenia | Lymphoproliferative syndromes (CLL, NHL, HL, etc.) |
The association between IBD and PIT in children is rare, with prevalences estimated at 0.1–0.48%, and with a higher frequency of association with ulcerative colitis (UC) compared to Crohn's disease (CD).3,5 We describe two cases of concurrent IBD and PIT, which are of interest considering the rarity of the association and the effects that the administered treatment may have on the course of disease.
Patient 1Female aged 11 years with a history of CD (Paris classification A1a L2 B1 G0) diagnosed based on the Oporto criteria at age 4 years and undergoing maintenance treatment with azathioprine (AZA) at 2.5mg/kg/day. At 9 years of age, while in clinical remission, she presented with ecchymosis and petechiae of sudden onset. Blood testing found a platelet count of 2000/mm3, and diagnostic tests were negative. The patient was given two doses of gammaglobulin (0.8g/kg/dose) and intravenous corticosteroids (2mg/kg/day) with no improvement, leading to diagnosis of PIT, and requiring maintenance therapy with gammaglobulin every three to four months (0.8g/kg/dose) for persistent thrombocytopenia. Eighteen months after being diagnosed with PIT, the patient had a clinical and endoscopic relapse of CD (PCDAI 35; SES-CD, 6). Induction therapy was initiated with humanised anti-TNF factor alpha (adalimumab [ADA]) following the standard dosage with administration every two weeks (160, 80 and 40mg by the subcutaneous route), after which the patient went into remission (PCDAI 0; faecal calprotectin [FC], 15mg/kg). The patient responded favourably, with stabilisation of the platelet levels, and corticosteroid therapy was discontinued. At present, the patient is being treated with combined AZA-ADA, and has not required additional courses of gammaglobulin or corticosteroids 24 months after initiation of ADA. The patient is awaiting a control colonoscopy, based on which a switch to monotherapy will be considered.
Patient 2Male aged 15 years with a CD diagnosis (A1bL2B1G0) undergoing maintenance treatment with mercaptopurine (6-MP) (1.5mg/kg/day). Seven months after the diagnosis, while in clinical remission (PCDAI 0), the patient developed isolated thrombocytopenia (85000/mm3). To rule out thiopurine-induced cytopenia (even though the rest of the cell counts and the thiopurine methyltransferase activity were normal), treatment was discontinued temporarily; the patient showed no improvement, with platelet levels reaching 9000/mm3, so treatment was resumed. The PIT diagnosis was reached after diagnostic test results came up negative. The patient was treated with gammaglobulin (0.8g/kg/dose) and showed an initial favourable response, although he subsequently needed corticosteroid therapy (0.4–1mg/kg/day) for maintenance. At present, 19 months following the PIT diagnosis, the patient remains in clinical remission with stable laboratory results (PCDAI 0; FC, 20mg/kg) under low-dose corticosteroid treatment (0.1mg/kg/day) with concurrent administration of mercaptopurine.
There are few descriptions of the association of CD and PIT in the literature (Table 2). The onset of PIT in association with IBD is variable, although based on the published cases it seems to occur more frequently after the diagnosis of IBD. Since the cases described in the literature involved UC more frequently than CD, we think it is worth noting that our patients with CD had exclusive colonic involvement, which supports the hypothesis that the inflammation of the colonic mucosa and/or the dysregulation of the local immune system may be associated with the development of PIT in these patients.3,5
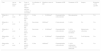
Cases of Crohn's disease associated with primary immune thrombocytopenia described in the paediatric age group.
| Case | Age at disease onset | Sex | Type of onset and time elapsed until first evidence of association | Localisation of CD | Platelets at onset of PIT | Treatment of PIT | Treatment of CD | Surgery | Remission of CD and PIT |
|---|---|---|---|---|---|---|---|---|---|
| 1Higuchi et al.3 | 11 years | M | CD 2.5 years before PIT | Colon | <10,000/mm3 | Gammaglobulin, corticosteroids | Mercaptopurine | No | Yes |
| 2Higuchi et al.3 | 2 years | F | CD 3 months before PIT | Ileocolonic | 6000/mm3 | Corticosteroids | 5-ASA | No | Yes |
| 3Higuchi et al.3 | 5 years | F | PIT 6 years before CD | Ileocolonic | <10,000/mm3 | Gammaglobulin, corticosteroids | 5-ASA, cyclosporin, tacrolimus | Splenectomy, colectomy | Yes |
| 4Manceñido et al.5 | 17 years | F | CD 6 years before PIT | Colon | <10,000/mm3 | Gammaglobulin, corticosteroids | 5-ASA, corticosteroids | YesColectomy | Yes |
| 5Manceñido et al.5 | 14 years | F | PIT 6 months before CD | Colon | 4000/mm3 | Gammaglobulin, corticosteroids | 5-ASA, azathioprine, corticosteroids, infliximab | No | Yes |
CD, Crohn's disease; F, female; M, male; PIT, primary immune thrombocytopenia; AIT, autoimmune thrombocytopenia; 5-ASA, sulfasalazine.
Studies in adults have described cases of PIT refractory to conventional treatment that responded well to treatment with anti-TNF factor, and it has been hypothesised that the pathogenic mechanism involves the apoptosis of monocytes and macrophages (which produce TNF alpha, as do CD4 lymphocytes), with a decline in the anti-platelet antibodies produced by B lymphocytes.6
We believe that in the cases reviewed here, while conventional therapy was used when PIT first developed (gammaglobulin and corticosteroids), the adequate control of CD with anti-TNF factor agents in case 1 and thiopurines in case two allowed for the improved management and outcomes of PIT, without requiring further gammaglobulin doses. The additional option of discontinuing corticosteroid treatment in our patient treated with anti-TNF factor makes the possibility of escalating treatment in patient 2 attractive if his CD does not respond favourably.
To conclude, it could be said that the association between PIT and CD is rare. The treatment used for maintaining CD in remission can also achieve adequate control of PIT. Thus, aggressive treatments can be avoided, improving quality of life in these patients.
Please cite this article as: Crespo Madrid N, Ruiz Hernández C, Giraldo Escobar L, Pujol Muncunill G, Martín de Carpi J. Coexistencia de enfermedad de Crohn y trombocitopenia inmune primaria y sus implicaciones en el tratamiento. An Pediatr (Barc). 2015;83:433–435.