To update the literature review on the effectiveness of clinical interventions on childhood obesity, proposed in Clinical Practice Guidelines, excluding prevention and pharmacological and surgical treatments.
MethodA systematic review was carried out in electronic databases of the Cochrane Database of Systematic Reviews (The Cochrane Library), MEDLINE, and SCOPUS, replicating the search for the Clinical Practice Guidelines, from 2009 to 2014. The Clinical Practice Guidelines of National Institutes for Health and Care Excellence were taken as a reference. Systematic reviews were given priority, and the quality of the studies was assessed.
ResultsOut of a total of 3.703 documents initially identified, 48 were finally included. Studies showed great heterogeneity in the type and duration of interventions, and in outcome measures. Adherence to treatment was, in general, low. Multi-component interventions including diet, physical activity, sedentary lifestyle, and behaviour changes, involving the family, and starting at early ages, were the most effective for reducing body mass index. There is no consensus on criteria for referral to specialised care.
ConclusionsIt is recommended to implement multi-component programs conducted by professionals with previous training, involving the family, and addressing behavioural, individual and socio-demographic aspects. Lack of adherence is one of the reasons for failure of interventions. Diagnostic and referral criteria, the outcome measures, and the type and duration of interventions need to be improved and standardised.
Actualizar la revision bibliográfica sobre la efectividad de las intervenciones clínicas en obesidad infantil propuestas en una Guía de Práctica Clínica, excluyendo los tratamientos farmacológicos y quirúrgicos y el abordaje de la prevención.
MétodoRevisión sistemática de las bases de datos electrónicas Cochrane Database of Systematic Reviews (The Cochrane Library), MEDLINE y SCOPUS replicando la búsqueda de la Guía de Práctica Clínica, desde el año 2010 a 2014. Se tuvieron en cuenta las Guías de Práctica Clínica del National Institute for Health and Care Excellence. Se priorizaron las revisiones sistemáticas. Se llevó a cabo un análisis de la calidad de los estudios.
ResultadosDe 3.703 documentos identificados se incluyeron 48 en la revisión. Los estudios mostraron gran heterogeneidad en cuanto al tipo y duración de la intervención, y a la medida de los resultados. En general, la adherencia a los tratamientos ha sido baja. Las intervenciones multicomponentes que incluyen alimentación, actividad física, sedentarismo y cambios de conducta, que implican a la familia y comienzan en edades precoces, son las más efectivas en la reducción del índice de masa corporal. No existe consenso en los criterios de derivación a la atención especializada.
ConclusionesSe recomienda implementar programas multicomponentes llevados a cabo por profesionales con formación previa, con participación de la familia, y que aborde aspectos conductuales, individuales y sociodemográficos. La falta de adherencia es uno de los motivos de fracaso de las intervenciones. Sería necesario mejorar y homogeneizar los criterios de diagnóstico, las medidas de resultados y los criterios de derivación.
The World Health Organization defines overweight and obesity as abnormal or excessive fat accumulation that may impair health and manifesting with excess weight and increased body volume.1 It has been labelled a XXI century epidemic on account of its impact on morbidity and mortality, quality of life and health care costs. Childhood obesity is a risk factor, given its frequent association with comorbidities both in childhood and adulthood. Thus, it is associated with type 2 diabetes mellitus, high blood pressure, dyslipidaemia, fatty liver disease, psychiatric disorders and others in the paediatric age group. Furthermore, obesity in adolescence is associated with a higher risk of obesity and increased morbidity and mortality in adulthood associated with stroke, ischaemic heart disease, tumours, etc.2 In addition, we have been witnessing an alarming increase in the prevalence of overweight and obesity in the past few decades, with a cohort effect in the epidemic, that is, obesity in younger generations is more prevalent and has earlier onset. In Spain, this phenomenon has been particularly pronounced, with prevalences that exceed those of most other European countries. The extent of the problem is considerably smaller in Anglo-Saxon and Scandinavian countries compared to Mediterranean countries. The ALADINO3 study found a prevalence of overweight of 14–26% in boys and 13–25% in girls, depending on the cut-off point applied, while the prevalence of obesity was 11–20% in boys and 11–15% in girls. According to the 2014 Health Survey of Catalonia, based on data reported by parents, the prevalence of overweight in children aged 6–12 years was 18.7%, the same for both sexes, and the prevalence of obesity was 11.7% (13.5% in boys and 9.9% in girls).4 These results are consistent with those of previous studies that had already found an increased prevalence of childhood obesity, such as the EnKid study.5
In this context, any preventive measures or interventions aimed at reducing overweight and obesity at early ages become critically important.
One of the multiple initiatives carried out to attempt to curb this epidemic was the development of the Clinical Practice Guideline (CPG) on the Prevention and Treatment of Childhood and Adolescence Obesity of the Spanish National Health System (Sistema Nacional de Salud [SNS]) in 2009.6 Since the intervention strategies that are being implemented now seem unable to control the increase of obesity and overweight, a critical review of the most recent evidence seems necessary in order to update the recommendations of CPGs.
The aim of our study was to perform an updated review of the literature on obesity and overweight in children and adolescents. More specifically, we intended to update part of the literature review in the aforementioned CPG,6 focusing on the criteria for referral from primary care (PC) to specialty care, and the evidence available on the management of overweight and obesity taking into account effectiveness and safety criteria. We excluded prevention and pharmacological and surgical treatment from the review. In addition, we included an analysis on some of the most recently developed interventions that could be effective on the target population, such as the use of information and communication technologies (ICTs).
MethodologyWe conducted a systematic review (SR) of the literature, replicating the literature search methodology used in the CPG of the SNS. We selected the questions of the CPG related to the criteria for referral from PC to specialty care (SC), and nonpharmacological and nonsurgical clinical interventions (Table 1). The literature search prioritised the identification of SRs and other critical summaries of the scientific literature, such evaluation reports on health technologies. We used the major updates on CPGs published recently by the National Institute for Health and Care Excellence (NICE)7,8 as a reference. We conducted searches in the Cochrane Database of Systematic Reviews (The Cochrane Library), MEDLINE and Scopus databases.
Questions of the SNS CPG included in the literature review.
| 1) Question 3: Which are the criteria for referral to specialty care? |
| 2) Question 15: In the population of children and adolescents with overweight or obesity, what is the effectiveness of dietary interventions on weight loss and maintenance and other specified variables? |
| 3) Question 16: In the population of children and adolescents with overweight or obesity, what is the effectiveness of physical activity or active play in weight loss or maintenance and other specified variables? |
| 4) Question 17: In the population of children and adolescents with overweight or obesity, what is the effectiveness of the reduction of sedentary time in weight loss or maintenance and other specified variables? |
| 5) Question 18: In the population of children and adolescents with overweight or obesity, what is the effectiveness of psychological treatment in weight loss or maintenance and other specified variables? |
| 6) Question 19: In the population of children and adolescents with overweight or obesity, what is the effectiveness of multicomponent interventions in weight loss or maintenance and other specified variables? Furthermore, in the last question, we added new interventions that may be effective. |
We mainly considered documents in Spanish, English and French. We searched for publications from January 2009 to December 2014. A description of the methodology used can be found in an earlier version of this document.9 Details on the search criteria can be obtained by consulting with the authors. The search was completed replicating the searches performed for the remaining questions of the SNS CPG, as we considered that most questions included nonspecific criteria and thus allowed the identification of documents that would answer the search questions for other CPG questions. We tried to replicate the inclusion and exclusion criteria of the original CPG during data collection. Once we had selected the documents, we developed evidence tables and assessed the quality of the evidence using the Scottish Intercollegiate Guidelines Network (SIGN) system10 (Table 2). We have attempted to summarise the primary outcomes based on body mass index (BMI) as changes in BMI expressed in standard deviations (SDs) or changes in the standardised score (z-score), effect size (ES) or kg/m2, when possible. We strived to summarise the rest of the primary or secondary outcomes for each question individually (for example, the lipid profile, duration of physical activity, sedentary time, etc.).
Levels of evidence and grading of recommendations of the Scottish Intercollegiate Guidelines Network (SIGN).
| Levels of evidence | |
| 1++ | High quality meta-analyses, systematic reviews of randomised controlled trials, or randomised controlled trials with a very low risk of bias |
| 1+ | Well conducted meta-analyses, systematic reviews, or randomised controlled trials with a low risk of bias |
| 1− | Meta-analyses, systematic reviews, or randomised controlled trials with a high risk of bias |
| 2++ | High quality systematic reviews of case control or cohort studies. High quality case control or cohort studies with a very low risk of confounding or bias and a high probability that the relationship is causal |
| 2+ | Well conducted case control or cohort studies with a low risk of confounding or bias and a moderate probability that the relationship is causal |
| 2− | Case control or cohort studies with a high risk of confounding or bias and a significant risk that the relationship is not causal |
| 3 | Non-analytic studies, e.g. case reports, case series |
| 4 | Expert opinion |
| Grading of recommendations | |
| A | At least one meta-analysis, systematic review or randomised controlled trial rated as 1++, and directly applicable to the target population; or a body of evidence consisting principally of studies rated as 1+ demonstrating overall consistency of results |
| B | A body of evidence including studies rated as 2++ directly applicable to the target population, and demonstrating overall consistency of results; or extrapolated evidence from studies rated as 1++ or 1+ |
| C | A body of evidence including studies rated as 2+ directly applicable to the target population, and demonstrating overall consistency of results; or Extrapolated evidence from studies rated as 2++ |
| D | Evidence level 3 or 4; or Extrapolated evidence from studies rated as 2+ |
| Good practice point | |
| Recommended best practice based on the clinical experience of the guideline development group | |
Source: Scottish Intercollegiate Guidelines Network (SIGN).10
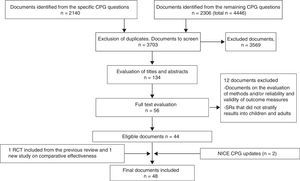
The initial literature search identified 3.703 documents after excluding duplicates (Fig. 1). After reading the titles and abstracts, we selected 134 documents, reading the full text of 55. Finally, 44 documents were included in the review and four others were added, two from secondary sources, and the NICE CPGs, which are considered the gold standard of CPGs. Appendix A, which is available online, details the included publications.
The review of the evidence and the updated NICE CPG for children was published in 2013,7 and the 2014 update8 includes recommendations for both prevention and management and targets both the paediatric and the adult population. The literature review in this CPG included 41 studies, of which 30 were randomised controlled trials (RCTs) and 11 real-life clinical trials. The recommendations of the NICE guideline focus on the development and implementation of “lifestyle weight management” programmes based on the best available evidence. This approach is based on a multicomponent intervention that includes physical activity, diet, behaviour change and family involvement.
Criteria for referral (Table 3)The updated review provides information based on the NICE CPGs and the review of six other CPGs (level of evidence [LE]=4), cross-sectional studies (LE=2) and two RCTs (LE=1−) (Table 3).
Criteria for referral from PC to SC.
| Authors, journal, year | Design and participants | Analysed outcome measures | Summary of results | Level of evidencea |
|---|---|---|---|---|
| Seibert, et al., J Clin Outcome Manage, 2014 | Narrative literature overview. Based on case study | Descriptive analysis of factors associated to referral to specialist | Severe obesity, comorbidity and lack of improvement in six months are the criteria for referral to specialty clinic. Obesity classified into four levels of severity. The two first levels are treated in PC, the third by a multidisciplinary team, and the fourth in SC | Level 4 |
| Walsh et al., Clin Pediatr (Phila), 2013 | Cross-sectional study based on visit data sets (United States). Includes 34,000 visits | Factors associated to specialist referral | 17% of PC visits had excess weight; 7% ended in referrals Two factors associated with referral: area of residence and obesity as reason for the visit | Level 2++ |
| Yaeger-Yarom, J Ped Endocrinol Metab, 2011 | Cross-sectional study (with a survey of minor patients and their parents) at the time of referral (n=227) | Reasons for referral, factors associated with obesity | The majority of patients were self-referred, mostly by the mother. The reason for the request in 45% of the cases was a desire to improve appearance or psychosocial factors | Level 3 |
| Banks et al., Br J Gen Pract, 2001 | RCT with two arms: PC vs inpatient treatment (initial n=152), ages 5–16 years. Nurses took a standardised training course on the management of obesity | BMI at 12 months. Inclusion criteria: BMI >98th percentile | Participation of 50% (final n=52, 30% refusal to participate) Reduction in BMI by −0.17 SD and −0.15 SD in each group, respectively. Reduction in both groups was statistically significant, with no differences between groups. The study has numerous risks for bias due to its methodology, lack of blinding, the variability in outcome measurement, etc. | Level 1− |
| Vander Baan et al., JAMA Pediatr, 2014 | RCT conducted in the Netherlands comparing inpatient and outpatient treatment (n=90) | Multicomponent structured programme that included parents, BMI, lipid profile and short- and long-term interventions | 45 patients assigned to 6 months of inpatient treatment vs 45 patients assigned to ambulatory treatment. The effect was better in the inpatient group in the short term (BMI z −0.26 [−0.59/−0.01]) and had disappeared by 30 months (−6.3%; P=.38). The ambulatory group also improved, although less: at 6 months, −10.5% (P=.001). The lipid profile also improved in the inpatient group. Both groups have similar long-term outcomes | Level 1+ |
| Richardson et al., Prev Med, 2013 | Review of CPGs in English and Dutch | Quality of the guidelines (AGREE instrument) and recommendations concerning lifestyle and criteria for diagnostic classification and referral | Six guidelines published up to 2010: NICE (2006), SIGN, Canada, New Zealand, Australia and Netherlands guidelines. In general, they agreed on recommending changes in lifestyle and multicomponent interventions that involve the parents. There was considerable variability in the classification of obesity and the criteria for referral | Level 4 |
BMI, body mass index; NICE, National Institute for Health and Care Excellence; PC, primary care; RCT, randomised clinical trial; SC, specialty care; SD, standard deviation.
The updates of the NICE guidelines did not include specific recommendations on the criteria for referral to SC, but show that intensive multicomponent interventions involving the multidisciplinary cooperation of different specialists are associated with a greater reduction of BMI than traditional treatments. The lifestyle weight management approach involves the development of interventions at the PC level with specific education on the subject.
A narrative overview of the reasons for referral to SC based on a case study explicitly proposed severe obesity, comorbidity and lack of improvement at six months as criteria for referral. Two cross-sectional studies showed that sociodemographic factors (area of residence), family predisposition and a previous diagnosis of obesity were associated with referral to the specialist. Studies comparing intensive treatment or inpatient treatment with treatment in PC found similar results in both groups at one year of followup (mean change in BMI=−0.17 SD in PC and −0.15 SD in inpatient), or better outcomes for short-term inpatient treatment, but these differences had disappeared by 30 months. These studies had relatively low participation rates (between 34% and 64%), so their results cannot be generalised. A review of six CPGs11 on the criteria for referral found significant differences in the criteria used for the diagnosis and classification of obesity and for referral from PC.
Dietary interventions (Table 4)The update of the SR improves the LE compared to the previous CPG, as it provides information based on a RCT (LE=1+), one SR of RCTs (LE=1+), and one SR of longitudinal studies (LE=2+) (Table 4).
Nutrition and diet interventions.
| Authors, journal, year | Design and participants | Analysed outcome measures | Summary of results Comments | Level of evidencea |
|---|---|---|---|---|
| Ebbeling et al., New Engl J Med, 2012 | RCT (n=224). Intervention in adolescent population with overweight and obesity focused on beverages (home delivery of sugar-free beverages), with regular check-in visits. Evaluation at 1 and 2 years | BMI, type of diet | Significant improvement at 1 year (BMI=−0.57kg/m2); when the intervention was finished, at the 2-year followup, the differences in BMI disappeared (−0.3, P=ns), but the differences in diet persisted (healthier) The effect varied by ethnic group | 1+ |
| Bourke et al., J Epidemiol Community Health, 2014 | SR in children aged 4–12 years. Longitudinal studies of dietary interventions for increasing fruit and vegetable consumption | Parent or child reports on fruit and vegetable consumption | Five studies implementing 7 interventions. Followup duration of 1 year (2 years in one study). No long-term differences were found. The authors attributed this to its being an isolated intervention | 2+ |
| Ossei-Assibei et al., BMJ Open, 2012 | SR of intervention and longitudinal studies in children aged less than 9 years on the influence of the food environment and certain dietary elements | BMI, body fat, diet questionnaires, food knowledge and preferences | Thirty-five studies; 19 reported BMI outcomes or outcomes of other measures linked to obesity, 7 studies of dietary intake, 7 of food knowledge and 2 of food preferences. The reduction of the promotion of high-calorie foods, making smaller portions available and providing alternatives to sugary drinks had an effect on obesity-linked measures, and above all improved habits. The review provides information on the influence of food availability | 2+ |
| Pérez Escamilla et al., J Acad Nutr Med, 2012 | SR of cohort studies in adults and children that included individuals with normal weight and obesity. Analysed the association between dietary energy density and adiposity | Energy intake (in beverages, in some cases) and BMI and/or adiposity | Six of the studies were conducted in children (n=48/2275). Duration of followup of 1–12 years. Variable outcomes: in general, the higher the energy density at 5–7 years, the greater the fat mass index at 9 years, but results were not consistent | 1− |
| Van Hoek et al., Child Obes, 2014 | SR of multicomponent or isolated interventions for obesity in children aged 3–8 years | BMI and z-score, variable duration of followup | Included 27 studies, 20 interventions in 1.015 participants. Heterogeneity in interventions based on their components. Two multicomponent interventions (diet+exercise+behaviour) achieved a reduction of BMI (−0.46 SD). This association was stronger in adults than in children | 1+ |
| Ho et al., JAMA Pediatr, 2013 | RS on the effects of diet and exercise in childhood obesity in individuals aged less than 18 years | Anthropometric measurements and metabolic levels. Interventions lasting 6 weeks to 6 months. Compares interventions using diet only to those using diet and aerobic exercise or resistance training | Fifteen studies. Diet-only interventions improved the levels of triglycerides. Diet and exercise interventions improved levels of HDL cholesterol, fasting glucose and fasting insulin. There were improvements in BMI, but there were variable, and it was difficult to determine whether there was an actual difference | 1+ |
| Van der Kruk et al., Obes Rev, 2013 | SR of RCTs to analyse the level of parental involvement and the outcomes, especially dietary, in the prevention and/or management of obesity. Children aged less than 12 years | Type of intervention, degree of parental involvement, outcome assessed based on BMI. Minimum followup of 6 months, maximum of 5 years. Taxonomy of behaviour change techniques | Twenty-four studies. The effectiveness depended on the intensity of involvement: greater involvement (active participation, not only knowledge and information) was associated with maintenance of BMI during intervention and through 1 year. Author-developed taxonomy of type of involvement and intervention. Possible biases in the assessment of effectiveness | 1− |
| Ajie et al., J Adolesc Health, 2014 | SR of studies on the use of computer-based interventions for changing dietary habits | Various measures: BMI, consumption of sugar-sweetened beverages, changes in dietary habits, etc. | Fifteen studies with considerable heterogeneity. In general, they found a small effect on BMI or dietary habits in the short-term. Gender differences must be taken into account based on the results of the study. The studies did not control for the type of programme or web contents, the type of intervention, parental participation, etc. | 1− |
| Hamilton et al., Health Tech Assess, 2014 | Community-based RCT that used an electronic device to control diet compared to standard care. Children aged 5–11 years with obesity. Intervention: use of the Mandolean device during meals to eat more slowly and monitor fullness | Analysed BMI at 12 months | The study did not achieve the necessary recruitment (initial recruitment was 58% of target) or followup to find evidence of differences between the two groups | 1− |
BMI, body mass index; RCT, randomised clinical trial; SR, systematic review.
Extreme dieting may have deleterious effects and is not associated with positive outcomes in the long term. Avoidance of sugary drinks is associated with a reduction of BMI at one year from the beginning of the intervention (BMI=−0.57kg/m2). Consumption of high-calorie foods is associated with increased body fat. Decreased promotion of high-energy foods and smaller portion sizes are associated with a more balanced diet and a decrease in obesity. Multicomponent interventions have better outcomes than diet-only interventions. In children aged less than 12 years, greater involvement of parents in dietary interventions is associated with better short-term outcomes.
Physical activity and sedentary time (Table 5)The update has not changed the existing LE in relation to physical activity, although it has reinforced some of the previous findings on its impact on the reduction of body fat and, to a lesser extent, of BMI (LE=1++) (Table 5).
Physical activity and sedentary time interventions.
| Authors, journal, year | Design and participants | Analysed outcome measures | Summary of results | Level of evidencea |
|---|---|---|---|---|
| Madsen et al., Child Obes, 2014 | Study of participation in physical activity programmes. Patients aged 6–18 years | Percent participation in community-based programmes after referral by health provider | The percent participation was 27% (n, 35/133). The mean duration of physical activity was 1.4h/week. The study did not identify specific factors associated with participation. Provides useful information on customary clinical practice | 2+ |
| Metcalf et al., BMJ, 2012 | SR and meta-analysis of interventions lasting at least 4 months with objectively measured outcomes of physical activity. Individuals with normal weight not excluded | Physical activity measured with accelerometers, measuring total and vigorous activity. Data collection period of 1–21 days | Thirty studies, n=14,326, 6153 with accelerometer-measured physical activity. Overall ES, 0.12 (0.04–0.2) and for moderate or vigorous activity, 0.16 (0.08–0.24). In the obese group, ES=0.22; ns. The study also found no differences between interventions lasting more or less than 6 months. No effect on BMI. Only six of the studies focused on obese children (n=691) | 1+ |
| Cesa et al., Prev Med, 2014 | SR and meta-analysis of RCTs. Inclusion: intervention lasting at least 6 months | Cardiovascular risk: BP, cholesterol, TG and BMI | Eleven RCTs. Overall, the interventions had no effect on BMI, but had an effect on BP (−1.24mmHg and −1.34mmHg in systolic and diastolic BP); and −0.09mmol/L in TGs Very heterogeneous interventions. Some studies also included minimal dietary changes | 1+ |
| Escalante et al., Prev Med, 2012 | SR and meta-analysis of RCTs to analyse the impact of physical activity and type of exercise (aerobic alone/combined) in the lipidic profile | Lipid profile: HDL, LDL, TG, TC | Six RCTs (n=318) and one CCT (non-randomised, n=38). Aerobic activity had an impact on LDL cholesterol (ES, −0.49) and TG levels (ES, −0.55). The minimum effective exercise was 60min 3times/week. Combined exercise improved HDL cholesterol (ES=0.5). The assessment of physical activity and participant characteristics was not fully controlled (for example, ethnicity was not controlled) | 1+ |
| Vasconcellos et al., Sports Med, 2014 | Narrative review in population of obese adolescents to study the association between physical activity and cardiovascular risk | Percent fat, BP, lipid profile, waist circumference, glucose and insulin | Twenty-four studies; n=1635. Fifteen studies with physical activity-only interventions, the rest with physical activity plus other interventions. Changes in % body fat, waist circumference, systolic BP, LDL and TC. Many heterogeneous studies with different objectives in relation to the outcomes | 1+ |
| Aguilar Cordero et al., Nutr Hosp, 2014 | Narrative SR of studies analysing physical activity | Lipid profile, anthropometric measurements. Duration of intervention and of sessions, type of exercise and role of diet | Includes 85 studies. Recommends a minimum of 2 weeks of combined aerobic and anaerobic exercise at least three times a week for at least 60min. Reinforces the idea that isolated interventions are less effective, and that family involvement is very important. The criteria for selecting studies were not clear and there was risk of bias | 1− |
| Kelley et al., J Obes, 2013 | SR of meta-analysis, children aged 5–18 years | Body fat, BMI and other outcome measures | Two meta-analyses with n=487 and n=701 and a reduced risk of bias. One of the meta-analysis focused on exercise and the other included other interventions (nonsurgical). Evidence of a significant reduction in body fat, but not in other measures. Calculated NNT=4 and 3 to achieve the significant reduction in body fat. High-quality SR | 1++ |
| Kelley et al., BMC Pediatr, 2014 | SR of RCTs | BMI. Physical activity for a minimum of 2 weeks | Ten studies (n=456 intervention and n=379 control). Significant reduction in BMI z-score of −0.06. Small risk of bias, although it included different types of interventions | 1+ |
| García Hermoso et al., Obes Rev, 2013 | SR and meta-analysis to analyse the effect of physical activity on BP. Age 7–16 years | Systolic and diastolic BP at rest. Exercise, type and duration. Duration of intervention in weeks | Nine studies (n=205 intervention and n=205 control). Aerobic or combined exercise. One hour more than 3 times a week reduces systolic BP (ES, −0.46). More than 12 weeks and more than 3sessions/week reduces diastolic BP (ES, −0.35). Some studies measured physical activity with accelerometers, while others used questionnaires (recall) | 1+ |
| Friederich et al., Rev Saude Publica, 2012 | SR and meta-analysis of interventions in the general population aimed at analysing the effect of physical activity, diet and a combination of both on BMI | Measurement of different types of physical activity, all studies on general population of school-aged children (includes individuals with and without obesity) | Twenty-three studies. The outcomes of exercise-only or diet-only interventions were not significant; however, combined interventions (n=9997) achieved a reduction in BMI with an ES of −0.37 (−0.63/−0.12). The study had a risk of bias associated to the measurement of interventions, and did not differentiate between children with obesity and children with normal weight | 1− |
| Liao et al., Obes Rev, 2014 | SR of studies of interventions targeting sedentary behaviours (age <18 years) | Limitation of sedentary behaviour alone or combined with exercise and/or diet. BMI as outcome measure | Twenty-five studies. Five studies with sedentary behaviour interventions (n=389 alone vs n=2.865 combined with physical activity and n=3851 combined with physical activity and diet interventions). Overall ES=−0.07, but ES was not significant when multicomponent and sedentary-behaviour only interventions were analysed separately. The pooled ES of multicomponent interventions was not different from the pooled ES of sedentary behaviour-only interventions. Some factors could not be stratified. Multicomponent interventions were carried out in clinic- or school-based | 1+ |
| Wahi et al., Arch Pediatr Adolesc Med, 2011 | SR of studies on reducing sedentary time in obese individuals aged less than 18 years | Primary outcome (BMI) and secondary outcome (hours of screen time) | Thirteen studies. Meta-analysis of BMI in six studies (n=21/1295). Ages 3–12 years. BMI=−0.10kg/m2; 95% CI, −0.28 to −0.9. Differences in total hours of screen time were not significant save in the under-6 years group, of −3.72h/week (95% CI, −7.23 to −0.20). Heterogeneous interventions | 1+ |
| Marsh et al., Obes Rev, 2014 | SR of studies of sedentary habits | Separates studies by setting. Seven of the 17 studies were in obese children (2–14 years). Analyses parental involvement. Hours of screen time in 4 studies | Overall n=3433 for the included studies, with wide sample-size variability in the different RCT (n=10–819). Challenges in the stratification of results by weight status (normal/obese). It suggests that screen time outcomes are better with active participation of parents and in the preschool-age group. Improvement could be due to energy intake (less sedentary time, reduced intake) rather than physical activity. Different outcome measures depending on setting (school, PC, community) | 1− |
| Schmidt et al., Obes (Silver Spring), 2012 | SR of various types of studies on the reduction of sedentary habits in children aged <6 years and children aged 6–12 years. Includes children with normal weight | Different methods to measure screen time (observation, self-report, TV monitor, other). Types of intervention: counselling, monitoring, physical activity, prohibition or removal of TV units from rooms | Of the 47 studies, 29 found a significant reduction in screen time. Fewer than half were studies focused on obese children. Eighteen studies analysed BMI. The SR had limitations. Includes the analysis of more vulnerable populations as a specific goal | 1− |
BMI, body mass index; BP, blood pressure; CCT, controlled clinical trial; ES, effect size; HDL, high-density lipoprotein; LDL, low-density lipoprotein; NNT, number needed to treat; RCT, randomised controlled trial; SR, systematic review; TC, total cholesterol; TG, triglycerides.
There is evidence that adherence to physical activity is poor when it is an isolated intervention. The studies that include physical activity for a minimum of 60min three times a week, either aerobic or of combined type, show a decrease in BP and improvement in the lipid profile. A review of interventions involving physical activity found a low increase in physical activity (ES=0.12 [P<.01]; in obese individuals, ES=0.22 [P=ns]). The type of physical activity (aerobic or anaerobic) and its duration may influence the levels of cholesterol or high- and low-density lipoprotein (HDL, LDL). Family involvement enhances intervention outcomes. Physical activity is associated with decreases in body fat and BMI, of very small magnitude in the latter. Interventions that combine physical activity and diet achieve significant reductions in BMI.12 Individual, family and environmental aspects should be taken into account in the recruitment and followup of intervention programmes.
When it came to sedentary time, most studies recommend a maximum of 2h a day, in agreement with the recommendation of the American Academy of Pediatrics.13 The outcomes of interventions that target sedentary time in isolation are not conclusive. Interventions that targeted sedentary habits were more effective when they involved the parents and when they were implemented at younger ages.
Psychological interventions (Table 6)The update has not changed the existing level of evidence (LE=1−), but we identified two studies that made a thorough analysis of interventions targeting behavioural factors. The analysis of the behavioural factors associated with diet (eating when not hungry, bingeing, emotional or addictive eating, or eating associated with family stress) allows a better approach to the management of obesity. Multicomponent lifestyle change interventions that involve the family (the parents and patients or the parents alone) seem to be more effective, as do interventions implemented at earlier ages (Table 6).
Psychological interventions.
| Authors, journal, year | Design and participants | Analysed outcome measure | Summary of results | Level of evidencea |
|---|---|---|---|---|
| Braet et al., Obes Facts, 2014 | Expert opinion and review of theories related to psychological factors in childhood obesity | Descriptions of different types of behaviours associated to food-related symptoms in obese children and approach to their assessment | Eating without hunger. Association between restrained eating, binge eating, emotional eating, craving and addiction or eating in the context of stress in the family. This study is a good source to understand the behavioural factors associated with obesity | 4 |
| Altman. et al., J Clin Child Adolesc Psychol, 2015 | SR of behavioural interventions and other treatment components. Types of intervention: family-based or parent-only behavioural treatment | Four categories of efficacy: well-established, probably efficacious, possibly efficacious, experimental, or of questionable efficacy | Family-based and parent-only behavioural programmes seem to be most efficacious. The treatments considered well-established were multicomponent and included diet, physical activity and behavioural interventions. There were multiple outcome measures. This SR has some bias risk. Other treatments considered less effective were motivational interviewing, appetite awareness, etc. | 1− |
SR, systematic review.
This update has changed the existing LE (LE=1++) regarding multicomponent interventions compared to isolated interventions, usual clinical practice and being on a waitlist. We have included nine SRs, some of high methodological quality, as well as a review of observational studies, one RCT, a comparative effectiveness study and the review of six CPGs mentioned above. Multicomponent intervention programmes are most effective if they are multidisciplinary and implemented by well-trained PC providers. These programmes should target families and address individual and social aspects (Table 7).
Multicomponent and other interventions.
| Authors, review, year | Design and participants | Analysed outcome measure | Summary of results | Level of evidencea |
|---|---|---|---|---|
| Reinher et al., Proc Nutr Soc, 2011 | Narrative review and comments based on the authors’ experience. No information on the criteria used to select studies or on the methodology of the review | Discusses possible interventions and a study by the author that applied a specific intervention, obeldicks, in Germany Analysis of the outcomes of the study at 2 years | Exhaustive review of several types of interventions, especially behavioural. It provides information on an intensive, one-year long multicomponent intervention (obeldicks). Multicentre studies (n=21,784) showed a significant decrease in BMI in 20% of the patients at 6 months, 14% at 1 year, and 7% at 2 years. Obeldicks was associated with better outcomes (BMI decrease by 0.4 SD) in 80% of the patients at the two-year mark in a sample of children aged 8–14 years. Cost of treatment=1.000 euro/patient. Recommends specific elements based on sex, type of intervention and family involvement. Addresses differences between everyday clinical practice and RCTs. Lack of motivation is not the only factor at play in low adherence. Interventions must be selected to fit individual needs | 1− |
| Reinehr et al., Nat Rev Endocrinol, 2013 | Narrative SR of long-term intervention studies | Review of weight measurements and the effectiveness of some factors of the interventions | Short-term interventions had little effect, with positive outcomes in only 10% of individuals, although some centres achieved success in 50%. Lifestyle change interventions worked better in overweight than in obese individuals. Interventions at age 5 years achieved weight loss or maintenance in 50%. The review did not include a description of the inclusion and exclusion criteria and risks of bias of the selected studies. Appropriate training of the providers delivering the intervention is an important factor | 1− |
| Ewald et al., J Public Health (Oxf), 2014 | SR of RCTs in children aged 5–12 years that compare parent-only vs parent-and-child or child-only interventions. Minimum duration of 6 months | Change in BMI at 12 months. Other changes, such as the BMI of parents, or changes in dietary habits | Six studies and two protocols for ongoing studies, with a total of 466 participants. The review found that parent-only interventions are at least as effective as interventions on the parent–child dyad or children alone. It analysed secondary outcomes such as reduction of BMI in parents | 1− |
| Gayes et al., J Consul Clin Psychol, 2014 | SR on motivational interviewing by specialised professionals and its effect on different health problems | Outcome effect size. Parent-only or parent-and-child interventions. Various health problems | Thirty-seven studies: 12 on obesity, the rest on other health problems. The results were significant in 2 of the 12 studies. Comparison of individual vs group therapy. Motivational interviewing seemed more effective when both parents and children participated | 1− |
| Ho et al., Pediatrics, 2012 | SR and meta-analysis comparing lifestyle interventions: behaviour modification and/or diet, with no treatment or waitlist, usual care and educational materials | Outcomes for BMI in weight in kg and z-score, lipid profile and fasting insulin | Thirty-eight studies: 22 with no-treatment controls, 11 with usual care controls, and 5 with educational materials. Meta-analysis of each comparison. Outcomes of studies with waitlist controls showed a reduction in BMI (−1.25kg/m2 [−2.18 to −0.32]). Studies of interventions >6 months compared to usual care (7 studies, n=586) also found a reduction in BMI (−1.30kg/m2 [−1.58 to −1.03]). All studies showed positive effects on lipid levels (except for HDL cholesterol) and BP. The SR is of very high quality and showed considerable variability in lifestyle, behavioural modification and combined interventions | 1++ |
| Hillier-Brown et al., BMC Public Health, 2014 | SR of RCTs or CCTs that analyse BMI or other obesity measures and socioeconomic status. Specifies intervention level (individual, community, school, societal) and the approach to inequalities (vulnerable population, reducing the gap, or the gradient), and whether interventions are targeted (vulnerable groups) or universal | BMI, body fat mass and others, and differential impact by SE status | Twenty-three studies: 4 individual-based, 17 community-based, one societal (environment/macropolicy) and one multilevel. Outcomes by SE status were variable. Seventeen studies of different community-based interventions also had variable results in the analysis by sex and SE status. A community-based study in Switzerland showed a trend towards a lower ES in individuals of low SE status. In general, the review shows that interventions do not widen existing inequalities. Wide variability in outcomes. The authors propose researching the impact of macropolitical measures on inequalities in obesity in school-aged children | 1− |
| Janicke et al., J Pediatr Psychol, 2014 | RS with meta-analysis of RCTs in individuals aged less than 19 years that compare multicomponent interventions with waitlist controls and isolated interventions | ES on weight, BMI, z-score or % body fat | Twenty studies, two-year followup, n=1671. Significant ES: 0.47 (0.36–0.58), considered small to moderate. Some moderators were also significant: age, duration and type of intervention, and number of sessions. Another secondary outcome was the reduction in energy intake | 1+ |
| Leech et al., Int J Behav Nutr Phys Act, 2014 | Review of observational studies that analyse the clustering of factors in ages 5–18 years | Measures of correlation between factors associated with obesity | Eighteen studies examined factors related to sedentary behaviour, diet or physical activity by sex and age. Socioeconomic factors also had an impact on outcomes | 2 |
| Sargent et al., Obes Rev, 2011 | Review of studies in PC settings that analysed the environment and interventions that showed an effect | Types of intervention, changes in BMI and other measures, and what factors of the intervention are associated with these changes | Seventeen studies; 12 describe effective interventions at the PC level. Training for health professionals before intervention delivery; behaviour change options and especially effecting behaviour change via a combination of counselling, education, written resources, support and motivation; and tailoring interventions all had an effect | 1− |
| Oude et al., Cochrane Review, 2009 | SR of RCTs that evaluate behavioural intervention, pharmacological treatment and surgery | Changes in BMI and adverse effects of interventions | Fifty-four studies (10 on pharmacological treatment). Physical activity=12; behaviour modification=36; diet=6. Behavioural interventions (n=321) achieved reduction of BMI (−0.14 SDs [−0.18 to −0.10]; or −3.27kg/m2 [−3.38 to −3.17]). One study of an internet-based intervention in girls showed that the effect disappeared in 18 months; 18 studies reported adverse effects, such as the development of eating disorders, anxiety or depression | 1+ |
| Taveras et al., JAMA Pediatr, 2015 | Comparative effectiveness RCT in PC settings. Three arms: (1) use of computer-based tools in the detection of obesity; (2) family coaching with motivational interviewing; (3) usual care | BMI and other secondary outcomes, such as adherence to treatment and robustness of information systems available to paediatricians | Fourteen PC centres, n=549. Patients aged 6–12 years with weight >95th percentile. One-year followup. Arm 2 had the largest change in BMI: −0.51kg/m2 (−0.91 to −0.11). The combined intervention arm also had better outcomes than the usual care arm. Secondary outcomes: improved description of providers, adherence and satisfaction of patients. Minimal results at one year. The group receiving the most intensive intervention did not achieve the best outcomes. Paediatricians showed improvement in the documentation of indicators, while patients showed improved adherence and satisfaction | 1+ |
| Other interventions: hours of sleep | ||||
| Ahuja et al., Agro Food Ind Hi-Tech, 2014 | Narrative review and opinion of authors | Unstructured review of different studies that analyse the association between sleep duration and obesity, does not exclude adults but focuses on childhood obesity | Mentions several studies that assess the association between sleep deprivation and obesity, and summarises the potential impact of hormones such as leptin and ghrelin that may be involved in the mechanisms underlying this association | 4 |
| Magee et al., Sleep Med Rev, 2014 | Review of longitudinal studies | Baseline hours of sleep and BMI or measure of obesity during followup | Out of the 20 studies, 7 were in children and found a correlation between fewer hours of sleep and a later increase in BMI. There was variation in the assessment of sleep duration | 2+ |
| Nielsen et al., Obes Rev, 2011 | SR of non-experimental studies | Association between baseline hours of sleep and subsequent increase in BMI | Includes 23 studies, of which 13 were in the paediatric population. Suggests a longitudinal association, although at least 4 studies were cross-sectional. Has some limitations regarding sleep measurement, methods, and timeframe, among others | 2+ |
| ICT tools (videogames and other) | ||||
| Trost et al., JAMA Pediatr, 2014 | RCT carried out in male and female participants with a mean age of 10 years | Monitoring of weekly physical activity by means of accelerometers and measurement of BMI at 16 weeks from initiation in the context of a family-based multicomponent intervention | Participation of 75 children, 34 were given a videogame and 41 were controls. Measurement of activity level and BMI. The control group was not given the videogame. The intervention group showed an increase in vigorous physical activity (2.8min/day) and decrease in BMI z-score (−0.25 vs −0.11, significant). The study was of acceptable quality | 1+ |
BMI, body mass index; CCT, controlled clinical trial; ES, effect size; HDL, high-density lipoprotein; ICT, information and communication technology; PC, primary care; RCT, randomised controlled trial; SE, socioeconomic.
Intensive interventions had better short-term outcomes. Long-term interventions with specialised training of health professionals and family involvement achieved better outcomes in younger children. Motivational interviewing is a technique that may have positive outcomes in behaviour change. Sociodemographic and socioeconomic factors impact the outcome of interventions. Training the providers that carry out the interventions is associated with better outcomes.
The literature includes reports of adverse effects of interventions, such as worsening of eating disorders, anxiety or depression.
The use of digital tools for the detection and followup of obesity in PC settings has been associated with fair outcomes at one year of followup.
Sleep deprivation is associated with an increase in BMI in the long-term. Further research is needed to elucidate the mechanisms underlying this association. The use of active videogames may have an impact in reducing BMI by four months of use.
Broadly speaking, given the association between the level of obesity and the presence of comorbidities, interventions that lead to improvements in obesity also have a direct impact on the improvement of associated comorbidities.
DiscussionOur study shows that multicomponent interventions on obesity and overweight in children and adolescents that include dietary, physical activity, sedentary time reduction and behavioural change interventions applied simultaneously achieve better outcomes than isolated interventions. Intensive interventions delivered by professionals with previous training on the subject in PC settings with consultation with SC are most effective. Furthermore, withdrawal of sugary drinks from the diet showed a short-term effect on BMI reduction. Outcomes also improve when families are involved, especially in younger children, and when socioeconomic status and other individual factors are taken into account. Further research is needed to evaluate the role of ICTs and to analyse the association between obesity and sleep duration.
The interpretation of the results of this review must take its limitations into account. We replicated the SNS CPG6 inclusion and exclusion criteria, although we prioritised SRs over other types of study. Therefore, we may have omitted some RCTs or other experimental studies. The considerable heterogeneity of the outcome measures analysed in the included studies precluded a quantitative summary of the results and hindered their comparison. In fact, some studies that analysed the validity and reliability of the outcome measures and the interventions performed in childhood obesity studies underscored the heterogeneity and wide variability of outcome measures, the challenges to the extrapolation of results, the different type and duration of interventions, and how these barriers prevent reaching generalisable conclusions in most instances.14,15 Last of all, this SR focused on interventions in the clinical setting and excluded pharmacological and surgical interventions. Still, our intent was to update the evidence in interventions delivered in PC settings, which is where most overweight or obese children and adolescents receive care. Finally, the information analysed in this SR has improved the existing LE on the effectiveness of multicomponent interventions compared to isolated interventions, and provides information that may help identify factors associated with lack of adherence and participation in interventions, as well as some of the potential adverse effects of interventions.
There is a clear need to standardise the criteria for the classification of weight, height and BMI and for referral to SC.11 There is no consensus on the reference values to be used, and this has negative repercussions on the analysis and assessment of the problem. In this sense, it would probably be beneficial to increase agreement compared to the current status quo.
One of the interventions that may be effective is the withdrawal of sugary drinks from the diet.16 Similarly, both the reduction of the energy density of foods and of portion sizes were associated with favourable outcomes.17 In any case, multicomponent interventions are most effective. However, many of the reviewed studies highlighted the poor adherence to treatment, and it is likely that adherence is even lower in real-life clinical practice. This is one of the main factors that contribute directly to treatment failure. The review also supports the beneficial impact of formal and standardised training of the providers that deliver the intervention with the purpose of improving outcomes.
On the other hand, the implementation of interventions should take into account individual factors and the fact that there is a significant socioeconomic gradient in obesity.18 The burden of morbidity, the decreased life expectancy and the health care costs caused by obesity in the adult population are rooted in the early stages of life; a more effective approach would be to tackle the health inequalities in childhood obesity, that is, the “causes of the causes”.19
ConclusionBased on the findings of our review, we recommend the implementation of multicomponent programmes delivered by professionals with special training, with family involvement, and addressing aspects analysed in this review such as behaviour and individual and sociodemographic factors (LE=1++; 4). Lack of adherence is one of the reasons why interventions fail, and the criteria for diagnosis, the outcome measures and the type and duration of interventions should be standardised and improved (LE=1+, 2++). Further research is needed on the evaluation of emerging ICT tools, as well as to develop a consensus on specific criteria for referral to SC tailored to the National Health System (LE=1+).
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Rajmil L, Bel J, Clofent R, Cabezas C, Castell C, Espallargues M. Intervenciones clínicas en sobrepeso y obesidad: revisión sistemática de la literatura 2009-2014. An Pediatr (Barc). 2017;86:197–212.