Pain in children population is prevalent, but its proper diagnosis and management are frequently insufficient in pediatrics daily practice. Lack of knowledge of the professionals in charge is a recognized barrier to ensure an appropiate approach to pain in this population. Our present study reflects the current status of pain management and the challenges in diagnosis and treatment that pediatricians face in their daily work. This information is obtained from a survey made with a voluntary questionaire, desinged and distributed online by “Grupo Español para el Estudio del Dolor Pediátrico (GEEDP)” to pediatricians in Spain from october 2021 to march 2022. The final objective of the questionaire was to shed some light into the problem and find out which areas of pain management knowledge are in need of improvent.
El dolor en Pediatría es un síntoma con frecuencia infradiagnosticado y deficientemente tratado a pesar de su prevalencia, siendo el déficit de conocimientos de los pediatras una de las barreras para garantizar un manejo eficaz. El presente trabajo describe el escenario actual y los retos en el abordaje diagnóstico y terapéutico del dolor infantil por pediatras en nuestro medio. Los resultados se obtienen de un estudio transversal descriptivo que se realiza entre octubre de 2021 y marzo de 2022 mediante encuesta de difusión a pediatras españoles diseñada por el Grupo Español para el Estudio de Dolor Pediátrico. Se pone el foco especialmente en las oportunidades de formación en diferentes aspectos del dolor pediátrico.
In a recent review published in 2020, the International Association for the Study of Pain defined pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”1 One of the proposed modifications of this definition that stands out for its comprehensive approximation to the concept of pain is “a distressing experience associated with actual or potential tissue damage with sensory, emotional, cognitive, and social components”2.
In paediatrics, the epidemiology of pain is difficult to establish, with an estimated prevalence of 30%–78% in the emergency care setting, of more than 70% during procedures and after surgery and 30% in chronically ill patients.3 Pain is a symptom that is often undetected and undertreated, which carries a risk of physical, psychological and social sequelae for the patient. Inadequate knowledge of pain and related skills in health care professionals is one of the main barriers to guaranteeing its effective management. Education is, unquestionably, the cornerstone of any strategy aimed at improving this inadequacy.4,5
To shed light on this problem, several working groups have been established in Spain,6–9 including the Spanish Group for Research in Paediatric Pain (Grupo Español para el Estudio del Dolor Pediátrico, GEEDP), of which the authors of this article are members. From a practical standpoint, training in a field as broad as paediatric pain poses significant challenges, motivating the GEEDP to conduct a cross-sectional descriptive study to analyse the perceptions of paediatricians in Spain about their knowledge and experience in the management of paediatric pain in different scenarios, in addition to their areas of interest and training needs. We conducted the study by distributing a questionnaire (Table 1) developed in the Google Forms platform through the electronic mail account of the Technical Office of the Asociación Española de Pediatría (Spanish Association of Pediatrics, AEP) to be completed anonymously between 25/10/2021 and 25/03/2022. The questionnaire comprised 36 items, and the answers were open-ended with a free-text field, or, in the case of items assessing satisfaction, rated on a Likert scale (1 inadequate, 5 excellent). We expressed quantitative variables as median and interquartile range (IQR) or mean and standard deviation (SD), as applicable depending on the distribution of the data, and categorical variables as absolute frequencies and percentages. The data were analysed with the software Stata version 14.2 (StataCorp; College Station, TX, USA).
Needs of training in paediatric pain.
| Training topics | Total (percentage) |
|---|---|
| Acute pain | 617/737 (83.7%) |
| Chronic pain | 567/737 (76.9%) |
| Procedural pain | 527/737 (71.5%) |
| Pain in specific groups | 501/737 (68%) |
| Nonpharmacological pain management | 477/737 (64.7%) |
| NS/NC | 5/737 (0.68%) |
NK/NA, does not know/does not answer.
We received 737 responses to the total questionnaires distributed to the members of the AEP, through which we obtained a perspective of the current management of pain in paediatric practice in Spain and identified areas of improvement.
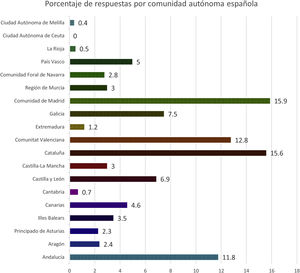
The paediatricians that submitted responses were mainly female (77.9%), with a median age of 43 years (IQR, 35–54) and a median experience in paediatric practice of 16 years (IQR, 9–25). Fig. 1 shows the geographical distribution of the sample. We were unable to determine how many questionnaires had been sent out. As regards the clinical setting, nearly half of the respondents (46%) worked in primary care (PC), followed in frequency by emergency care (40.3%), inpatient care (39.2%), and outpatient hospital-based care (33.8%), with a lower proportion of respondents in intensive care unit (neonatal, 12.5%; paediatric, 8.3%). In addition, 43.86% worked in more than one paediatric care setting or field (median, 1; IQR, 1–2), and most (81.8%) worked exclusively in the public health system (7.3% in the private system and 10.9% in both).
Less than half of respondents (49.93%) had received some form of specific training on paediatric pain, and this type of training was more frequent in hospital-based paediatricians compared to those in PC (57.93% vs 40.71%; P<0.01). Most of them received training in the form of courses (47.8%), while 2.68% had master’s degrees and fewer than 1% workshops or training sessions. Only 13 paediatricians (1.74%) had participated in more than 1 type of pain education. Yet, 96.4% of respondents considered that paediatric patients suffered easily preventable acute pain (93.15%), chronic pain (23.76%), procedural pain (66.31%) or postoperative pain (21.48%).
The results of the self-reported knowledge on paediatric pain assessed through items rated on a Likert scale were: management of acute pain, median of 3 points (IQR, 2–4), management of chronic pain, median of 2 points (IQR, 2–3) management of procedural pain, median of 3 points (IQR, 2–4). In consequence, 99.05% of respondents thought that educational activities on paediatric pain would be beneficial, without differences between the hospital and PC setting, addressing the subjects listed in Table 1. Respondents preferred online trainings (63%) and hybrid online-in person trainings (58.5%), to in-person trainings, either practical (34.8%) or theoretical (13%). Furthermore, in the section devoted to suggestions, respondents reasserted the need of training in paediatric pain management in the PC and palliative care settings and during the medical residency.
Current situation of paediatric pain management in SpainDiagnosis and assessment of painMost respondents (97.8%) reported that pain was assessed at some point in the management of paediatric patients, more frequently in the hospital setting compared to the PC setting (99.51% vs 95.87%; P<0.01). A high percentage (58.6%) also reported that pain was assessed by more than 1 professional, with a median of 2 professionals per patient per care episode/visit (IQR, 1–3), most frequently by staff physicians (87%), especially in PC compared to the hospital setting (91.45% vs 83.70%), and by nurses (62%), especially in hospitals compared to PC (80.74% vs 39.23%), while medical interns and residents were mostly not involved in this task (36%) and very infrequent involvement of nursing technicians (6%).
Studies focused on paediatric inpatients have found a prevalence of pain of 66%–77% and documentation of pain in 27% of the patient health records.10–12 In our study, 91.3% of paediatricians reported that pain was assessed at some point during the hospital stay, usually on demand (38%). Routine assessment of pain was reported by fewer than half (34.3%) and pain assessment at admission by only 19.5%, with a median of 1 pain assessment documented per inpatient episode (maximum, 3; minimum, 0). These figures reflect an underdiagnosis of pain during hospitalization and a status quo that is far from the recommendation of assessing pain as the fifth vital sign.3
Pain must also be assessed and appropriately documented in all patients that visit a paediatric emergency department, as its intensity will proportionally affect the priority assigned in the classification of the patient or triage process.13 Furthermore, the assessment of pain would continue throughout the entire care episode.14 A multicentre study conducted by the Sociedad Española de Urgencias Pediátricas (Spanish Society of Paediatric Emergency Medicine) found that pain was documented at the time of triage in 42% of encounters and in the discharge summary in 27.6%; documentation in the discharge summary was significantly more frequent when pain had also been documented at the time of triage than when it had not (60.5% vs 39.5%).15 In our study, most respondents reported that pain was assessed at some point in the emergency department visit (92.5%), mainly during triage (42.6%), and less frequently after triage or when the patient met the paediatrician (both 37.4%), and the median number of times that pain was assessed during the care episode was 1 (maximum, 3; minimum, 0).
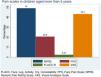
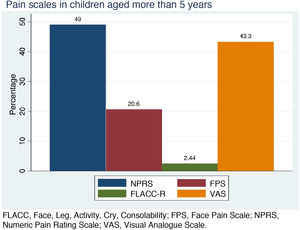
Effective diagnosis of pain in children is an aspect of care that is still not up to standard. The preferred approach for pain assessment and diagnosis in children capable of verbal communication is, whenever feasible, self-reporting, as pain is a subjective experience. However, the validation of an adequate instrument that can be applied to the entire age range and in different scenarios has proven elusive. Although it has limitations, the instruments that can be recommended with the most rigorous evidence in support of their use are the FACES Pain Rating Scale-Revised for acute pain, and the Numeric Pain Rating Scale and the Visual Analogue Scale for all types of pain in children from age 6 years without impairments in communication.16 This was reflected by the results of our survey, in which 78.7% of respondents reported using an appropriate scale for these patients; Fig. 2 shows the use of the different scales in this group of respondents (31.89% reported using more than 1 scale).
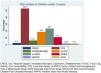
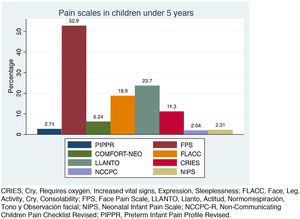
In children under 5 years (preverbal stage) or with communication difficulties, assessment of pain and its intensity becomes complicated. Multiple scales have been validated to assess pain based on behavioural and/or physiological parameters. A recent systematic review highlighted that of the 65 scales most frequently used in this age group, only 43% had an adequate construct validity, interrater agreement and reliability.17 The fact that most have been developed in English-speaking countries also complicates their application.18 The recommendation to use one instrument or another depends on the care setting, but an essential aspect is the routine use of some of these scales. Of all respondents, 25.2% did not use any instrument in this group of patients, especially in PC, where this percentage increased to 32.45%, while 56.5% of respondents used inadequate scales; Fig. 3 shows the frequency of the use of different scales (37.3% used more than 1 scale).
As we highlighted in our previous publication,3 several scientific associations, with the support of the World Health Organization (WHO), endorse the approach to pain management as a human right.19 This necessitates documentation of pain somewhere in the health records, where it can be accessed by all health care professionals, including information of its intensity and characteristics at specific time points. This necessity has even been identified as a priority by accreditation programmes and institutions.20 The diagnosis of pain in Spain is seamlessly integrated in nursing practice applying the diagnostic criteria of the North American Nursing Diagnosis Association (NANDA), used to code acute and chronic pain. Thus, and the NANDA has stated, these diagnoses “help strengthen a nurse’s awareness, professional role, and professional abilities”, in this case, in pain management.21 This is not the case of medical records, for, while in 2019 the WHO launched the new International Classification of Diseases, 11th revision (ICD-11), which includes new classifications related to diseases that manifest with chronic pain, there are still inadequacies in the diagnosis of acute and chronic pain in care delivery.22 Illustrating this situation, many respondents in our study (54.2%) did not document pain in the health records as one of the diagnoses or conditions of paediatric patients, while 29.6% did it sometimes and 15.4% did it routinely.
Treatment of painIn our survey to investigate the current situation of paediatric pain management in Spain, the most important aspects had to do with the management of chronic or complex pain, severe pain, and mild to moderate procedural pain.
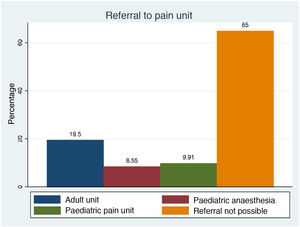
Based on data from the Sociedad Española del Dolor (Spanish Pain Society), there are approximately 200 pain management units in Spain,23 but a recent study only identified 10 units or programmes to manage pain in children and adolescents, and only 5 specifically devoted to pain management in children. The programmes were very heterogeneous in terms of size, type of patients and the professionals involved (100% included anaesthesiologists and 87% paediatricians in the care team).24 There are no established standards as to the composition of paediatric chronic pain management units.25 When it came to the management of pain in chronically ill or medically complex patients, 14% of respondents did not know whether they had access to a specialised pain management unit to refer patients to, and only 35% reported access to pain management units, in most cases units developed for adults (Fig. 4).
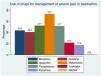
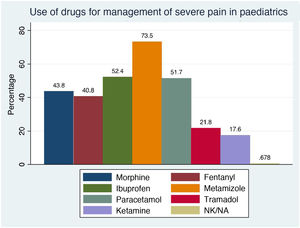
There is frequent mention in the literature of the lack of training in the management of severe pain in paediatrics, which can contribute to the persistence of some myths and barriers in the use of opiates and translate to suboptimal pain relief.26,27 On the other hand, due to the scarcity of studies in the paediatric population, morphine continues to be the most frequently recommended opioid, especially for pain in patients with life-limiting illnesses or at the end of life.28 In our survey, in response to the question regarding the pharmacological management of severe pain in paediatric patients, 99.3% of respondents confirmed the use of at least 1 drug and 87.4% of more than 1 drug (median, 3; IQR, 2–4). Fig. 5 presents the distribution of the most widely used drugs, with opioids, alone or in combination, being the most frequent type (36.6%). However, only 15.9% reported having adequate or expert knowledge on their use, with a higher frequency in hospital-based physicians compared to those working in PC (25.19% vs 4.42; P<0.01), and 19.3% knowledge of how to manage their adverse effects. On the other hand, fewer than half (49.2%) reported using medication for management of opioid withdrawal, and the drug used most frequently for this purpose was methadone (37.2%).
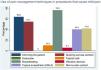
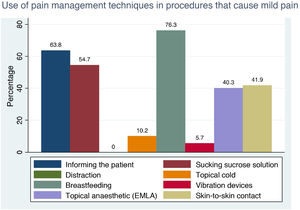
When it comes to mild to moderate procedural pain, which is very frequent in paediatric clinical practice in any care setting (e.g. vaccination, heel puncture, phlebotomy etc), there are pharmacological and non-pharmacological approaches to analgesia.29 A salient finding in our survey was that 20.6% of paediatricians reported not using any prophylactic analgesic technique, although most of the respondents that reported using prophylactic analgesia used a mean of 2 strategies (IQR, 1–3) in each procedure (see techniques featured in Fig. 6). In most instances, reported pharmacological approaches consisted in the topical administration of analgesic creams, which has been proven to reduce pain during these procedures.30,31 Although there has been evidence in support of the use of analgesic creams for more than three decades,32 only 40.3% of respondents used them. This low percentage could be due to a fear of methaemoglobinaemia developing as a side effect and to the time that has to elapse from the application of these creams until they start having an effect, which is a disadvantage in an emergency.
In recent years, there has been an increase in the literature devoted to nonpharmacological analgesia.33 Nonpharmacological methods may be adjunctive (such as videos, games), cognitive (such as distraction, music), behavioural (such as breathing or relaxation exercises) and physical (such as application of heat or cold, massage).34 Specifically, distraction strategies have proven effective in reducing anxiety and pain in invasive procedures.35 Breastfeeding and administration of sucrose solutions are also effective in reducing pain by inducing the release of endogenous opiates27 even at very low doses, which allows their use in patients that cannot have enteral nutrition.36 Despite this evidence, our study revealed infrequent use of these methods by surveyed paediatricians: respondents only reported the use of physical methods such as application of cold (10.2%) or vibrations (5.7%), but not of distraction methods. However, on the positive side, 76.3% of respondents did promote breastfeeding (most frequently in the PC setting, where this practice increased to 79.9%; P<0.01) y un 54.7% used sucrose solutions (more frequently in the hospital setting, 74.32%; P<0.01).
Nitrous oxide is a colourless, odourless gas with analgesic, sedative and amnesic properties. The equimolar mixture of oxygen and nitrous oxide (EMONO) is the one that has become most widespread for sedation and analgesia. It has significant advantages, such as an easy and painless administration, a rapid onset and short duration of action37 and a low incidence of adverse events.38,39 This suggests that it could be safely administered by adequately trained health care professionals other than anaesthesiologists,40 so it could be used in procedures performed by physicians and nurses that require mild to moderate anaesthesia, anxiety relief, partial amnesia or a combination thereof. In spite of this evidence, a very small percentage of respondents (13.8%) reported having access to EMONO for procedures, and in those instances, the professionals most frequently responsible for its administration were paediatricians (34.87%), followed by nurses (6.8%) and anaesthesiologists (<1%).
Limitations of the studyThere are several methodological limitations to our study that may restrict the interpretation or applicability of its results. Due to the distribution of the questionnaire through a scientific society (AEP), we do not know the actual number of questionnaires that were sent out. The AEP currently has 12 200 members, but not all received the questionnaire. The 737 members that submitted responses were conscious of the deficient visibility and awareness of paediatric pain, and constituted a substantially large group whose opinion should be taken into account. Furthermore, we did not distribute the questionnaire among nursing professionals, and given that it is nursing staff that assess pain in a large proportion of cases, this was also a limitation of the study.
ConclusionAdequate management of paediatric pain continues to be a challenge. One of the barriers to guaranteeing effective management of pain in children is a lack of knowledge by paediatricians, so it is key that an emphasis continues to be placed on training needs.
Based on the findings of our study, we may conclude that surveyed paediatricians were aware of pain as a health problem, but despite long years of clinical practice, we found a persistent lack of confidence in its management and an interest in participating in educational activities on different aspects of pain. One possibility that deserves particular consideration is the integration of pain education in the educational curriculum of the residency in paediatrics.
The main opportunities for improvement identified in the study were the assessment of pain as a vital sign, the use of opiates in paediatric patients and the use of analgesia in procedures that cause mild to moderate pain. As regards to chronic or complex pain, given the small number of specialised multidisciplinary units in Spain, we must promote the coordination and networking of health care professionals and streamline the referral process.
Lastly, to address these challenges, it would be helpful if the different working groups interested in paediatric pain in Spain were to join efforts.
Please cite this article as: Mozo del Castillo Y, Toledo del Castillo B, Navarro Marchena L, Leyva Carmona M, Monfort Carretero L, Míguez Navarro MC, et al. Situación actual y retos de los pediatras Españoles en el manejo del dolor infantil. An Pediatr (Barc). 2022;97:207.