The characteristics of catch-up growth in very low birth weight infants (VLBW) have not been clearly established. The aim of this study was to analyse the height catch-up and some associated factors in a cohort of VLBW birth weight <1,500 g from birth to age 14 years.
MethodsWe obtained retrospective data on weight and height at birth and ages one, 2, 3, 4, 6, 8, 10, 12 and 14 years in a cohort of 170 VLBW. We compared these anthropometric values with those documented in a control group.
ResultsThirty-seven children (21.8%) were born with an extremely low birth weight and 32 (18.8%) extremely preterm. At 10 years of age, 7% of VLBW (1,000–1,500 g) and 35% of extremely low birth weight <1,500 g children had short stature P = 0.001). Almost all VLBW children who had a normal height at ages 2, 4 and 10 years had exhibited adequate weight catch-up in previous evaluations. We found that extremely low birth weight and extremely preterm were independent predictors for inadequate height catch-up.
ConclusionThe growth pattern of VLBW children has specific characteristics. The catch-up in weight seems to be an important factor for catch-up in height, and therefore a thorough nutritional follow-up is recommended in these children.
Las características del crecimiento recuperador en niños con muy bajo peso (MBP) al nacer no se han establecido con claridad. El objetivo del estudio fue analizar el crecimiento recuperador de talla y factores asociados en una cohorte de niños con MBP al nacer (< 1.500 g) desde el nacimiento hasta los 14 años de edad.
MétodosSe recogieron datos retrospectivos de peso y talla a uno, 2, 3, 4, 6, 8, 10, 12 y 14 años de edad en una cohorte de 170 recién nacidos con MBP. Se compararon estos datos antropométricos con los registrados en un grupo de control.
ResultadosTreinta y siete niños (21.8%) nacieron con extremado bajo peso y 32 (18.8%) fueron pretérmino extremo. A los 10 años de edad, el 7% de los niños con MBP (1.000-1.500 g) y el 35% de los niños con extremado bajo peso < 1.500 g tenían talla baja p = 0,001. Casi todos los niños con MBP que tenían una talla normal a los 2, 4 y 10 años de edad habían alcanzado un peso adecuado en evaluaciones previas. El extremado bajo peso al nacer y el nacimiento pretérmino extremo resultaron ser predictores independientes de un crecimiento recuperador de talla inadecuado.
ConclusiónEl patrón de crecimiento de niños con MBP al nacer tiene unas características específicas. El crecimiento recuperador de peso parece ser un factor importante para el crecimiento recuperador de talla, por lo que se recomienda un seguimiento nutricional cuidadoso en estos niños.
Infants born to term with a history of intrauterine growth restriction constitute a heterogeneous population with multifactorial health problems and, in addition to exhibiting a higher morbidity and mortality, are at increased risk of cardiovascular and/or metabolic disease in adult life.1 These patients show an accelerated compensatory growth pattern (catch-up growth) that is usually complete by age 2 years.2–4 However, the characteristics of catch-up growth have not been well established in very preterm (VPT) infants (born before 32 weeks’ gestation) or very low birth weight (VLBW) infants (birth weight < 1500 g). Nonetheless, the follow-up of these patients, despite the presence of contradictory data, suggests that their catch-up growth could occur at a later stage, and therefore have an impact on future adult size.5–7
Little is known about the factors that determine whether catch-up growth occurs in VPT or VLBW infants, but there is evidence that low birth weight or prematurity and medical complications are negatively correlated to postnatal growth.5 On the other hand, few authors have analysed the catch-up growth in weight of these children in relation to the concurrent catch-up growth in height, although unsurprisingly previous studies have found a positive correlation between energy intake and postnatal growth in preterm infants.8,9
The objective of our study was to make a longitudinal descriptive analysis of anthropometric measurements in a cohort of very low birth weight (VLBW) infants from birth to 14 years of age, and then analyse the characteristics of catch-up growth in height and some associated factors in these patients.
MethodsParticipantsThe official child wellness programme of the public health system of the region of Navarre in Spain includes regular health screenings during which anthropometric measurements (weight and height) are documented in the clinical records, at birth and at ages 1, 2, 3, 4, 6, 8, 10, 12 and 14 years.
Within this framework, the anthropometric measurements considered in our study (weight and height) corresponding to birth and ages 1, 2, 3, 4, 6, 8, 10, 12 and 14 years had been recorded for the cohort of VLBW infants (<1500 g). The inclusion criteria were being Caucasian and born to Caucasian Spanish parents, and birth in the Neonatal Unit of the Complejo Hospitalario de Navarra between January 2001 and December 2005.
The weight and height measurements were made with the children in their undergarments and barefoot. Weight was measured using an Año-Sayol scale (range of 0–120 kg and accurate to 100 g), and height was measured with a Holtain wall stadiometer (range of 60–210 cm and accurate to 0.1 cm).
We found records for 217 births of VLBW infants in this period, of which we excluded 47 for different reasons: perinatal mortality in 20 (9.2%), severe malformations and/or chromosomal disorder in 6 (2.8%), severe neurosensory impairment and motor sequelae in 5 (2.3%), non-Caucasian descent in 8 (3.7%) and other reasons (distance to hospital, lack of continuity in paediatric health screenings, etc.) in 8 cases (3.7%).
We classified the VLBW infants included in the study into two groups: those born with weight appropriate for gestational age (AGA) and those small for gestational age (SGA), based on whether the birth weight and/or length where or not 2 or more standard deviations below the mean for gestational sex and age of the reference population. The growth reference charts for newborns that we used in this came from the Spanish cross-sectional growth study by Carrascosa et al.10 We considered infants with birth weights of less than 1000 g extremely low birth weight (ELBW). We categorised preterm birth based on gestational age (GA) into extremely preterm (EPT, GA < 28 weeks), very preterm (VPT, GA = 28–32 weeks) and late preterm (LPT, GA = 32–37 weeks).
On the other hand, we obtained a control group from an observational epidemiological study carried out in an infant population (healthy full-term infants, Caucasian and children from Caucasian parents, 482 male and 448 female) in who anthropometric measurements were taken on a similar schedule to the one followed in the cohort of VLBW infants.11
We defined adequate catch-up growth in either height or weight in VLBW infants as the height or weight, as applicable, being above the value of 2 standard deviations below the mean in the growth charts of the control group.2–4
Statistical analysisWe summarised the data as percentages (%) and mean values with the corresponding standard deviations (SD) and 95% confidence intervals (CIs). We performed the statistical analysis (descriptive statistics, Student t test, analysis of variance, chi square test and multiple logistic regression analysis) with the Statistical Package for the Social Sciences (SPSS) version 20.0 (Chicago, IL, USA). We defined the threshold of statistical significance at a p-value of 0.05.
The study was approved by the Ethics Committee for Research in Humans of the Complejo Hospitalario de Navarra, Pamplona, Spain, and conducted in adherence to the ethical standards of the Declaration of Hensinki of 1964 and later amendments. The parents and/or legal guardians of children included in the study gave their informed consent for participation.
ResultsThe sample included 170 VLBW infants (82 male and 88 female), of who 42.4% were product of multiple pregnancies (n = 72). Out of all infants born with VLBW, 40.6% (n = 69) were small for gestational age (SGA group) and the remaining 59.4% (n = 101) appropriate for gestational age (AGA group). Within the SGA group, both weight and length were affected in 59.4% of the infants (n = 41), while only length was abnormal in 23.2% (n = 16) and only weight in 17.4% (n = 12). Thirty-seven (21.8%) were considered ELBW. The distribution of infants born preterm by GA was 18.8% extremely preterm (n = 32), 42.4% very preterm (n = 72), and 38.8% late preterm (n = 66).
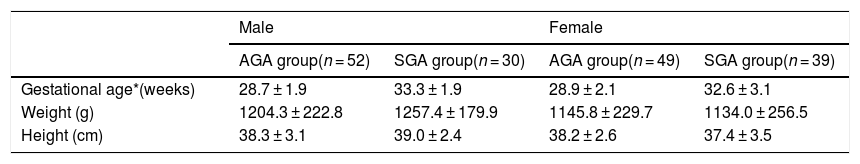
Table 1 presents and compares the anthropometric values at birth of VLBW infants in the AGA and SGA groups and by sex. We found no statistically significant differences in the mean weight and height values at birth between the 2 groups. Gestational age was significantly higher in the SGA group compared to the AGA group.
Gestational age, birth weight and birth length of VLBW infants by sex (mean ± SD).
| Male | Female | |||
|---|---|---|---|---|
| AGA group(n = 52) | SGA group(n = 30) | AGA group(n = 49) | SGA group(n = 39) | |
| Gestational age*(weeks) | 28.7 ± 1.9 | 33.3 ± 1.9 | 28.9 ± 2.1 | 32.6 ± 3.1 |
| Weight (g) | 1204.3 ± 222.8 | 1257.4 ± 179.9 | 1145.8 ± 229.7 | 1134.0 ± 256.5 |
| Height (cm) | 38.3 ± 3.1 | 39.0 ± 2.4 | 38.2 ± 2.6 | 37.4 ± 3.5 |
(*) Student t test, P < 0.05 in comparison of AGA and SGA.
AGA, appropriate for gestational age; SGA, small for gestational age.
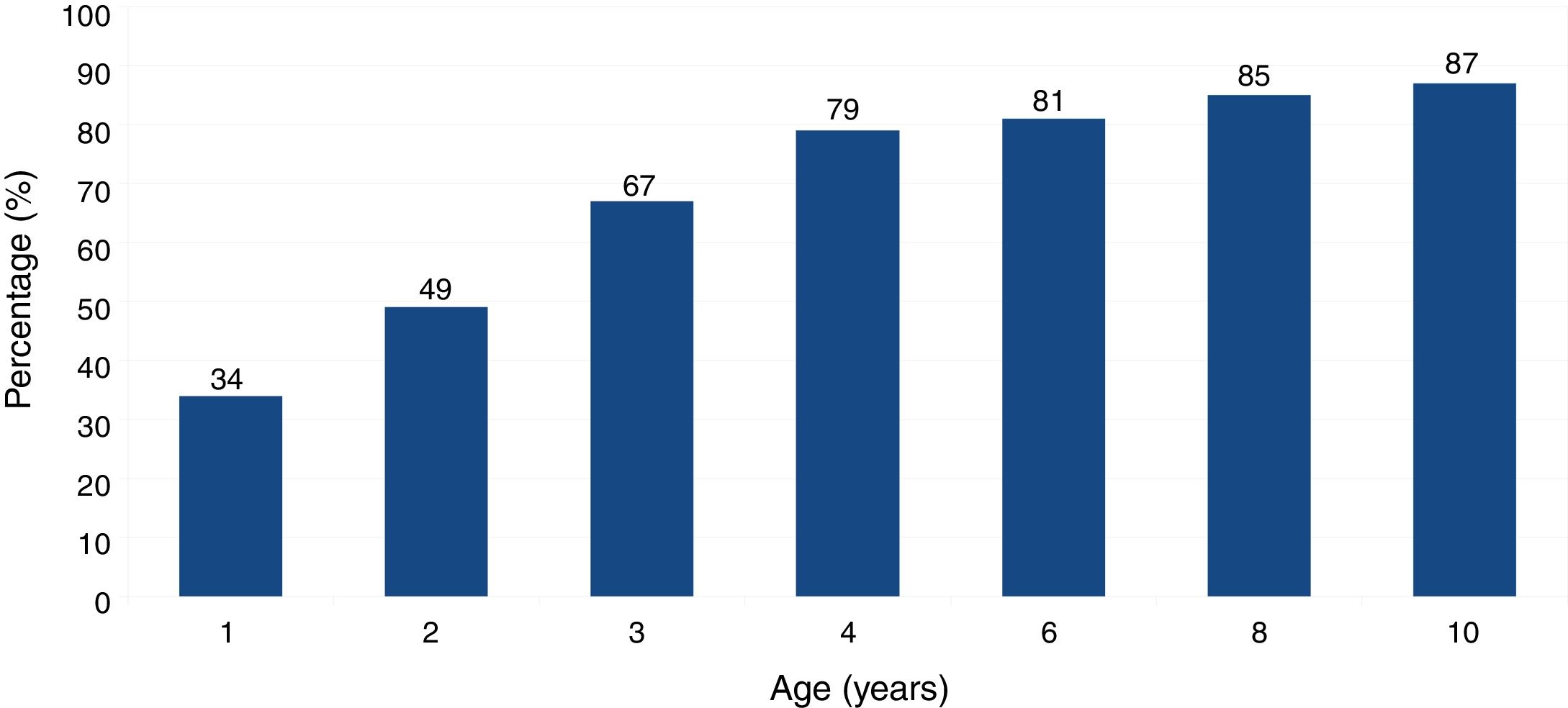
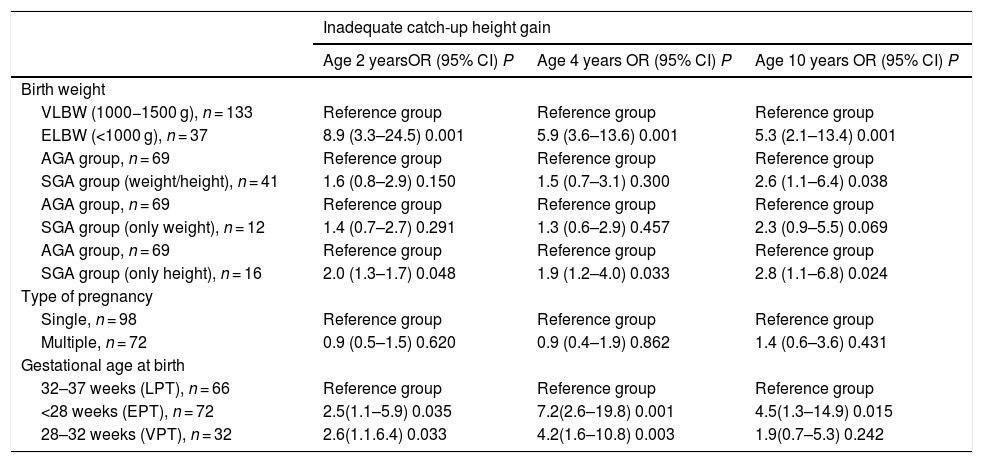
Fig. 1 presents the percentage of VLBW infants who had achieved a normal height at the different ages considered in the study. At age 2, 4 and 10 years, 49.4%, 78.9% and 87.1% of infants, respectively, had achieved a normal height. Thus, 8.2% of VLBW infants reached normal height between ages 4 and 10 years.
Our results show that 86% of VLBW infants that had achieved a normal weight after the first year of life achieved a normal height (P < 0.001) by age 2 years. In addition, 98.6% of VLBW infants with a normal weight at age 2 years had achieved a normal height (P < 0.001) by age 4 years. Similarly, 97.2% of VLBW infants with normal weight at age 4 years had normal heights (P < 0.001) by age 10 years, 99.2% of VLBW infants with normal weights at age 6 years had normal heights by age 8 years (P < 0.001), and lastly, all VLBW infants that had normal weights at age 10 years also had normal heights at this time point (P < 0.001).
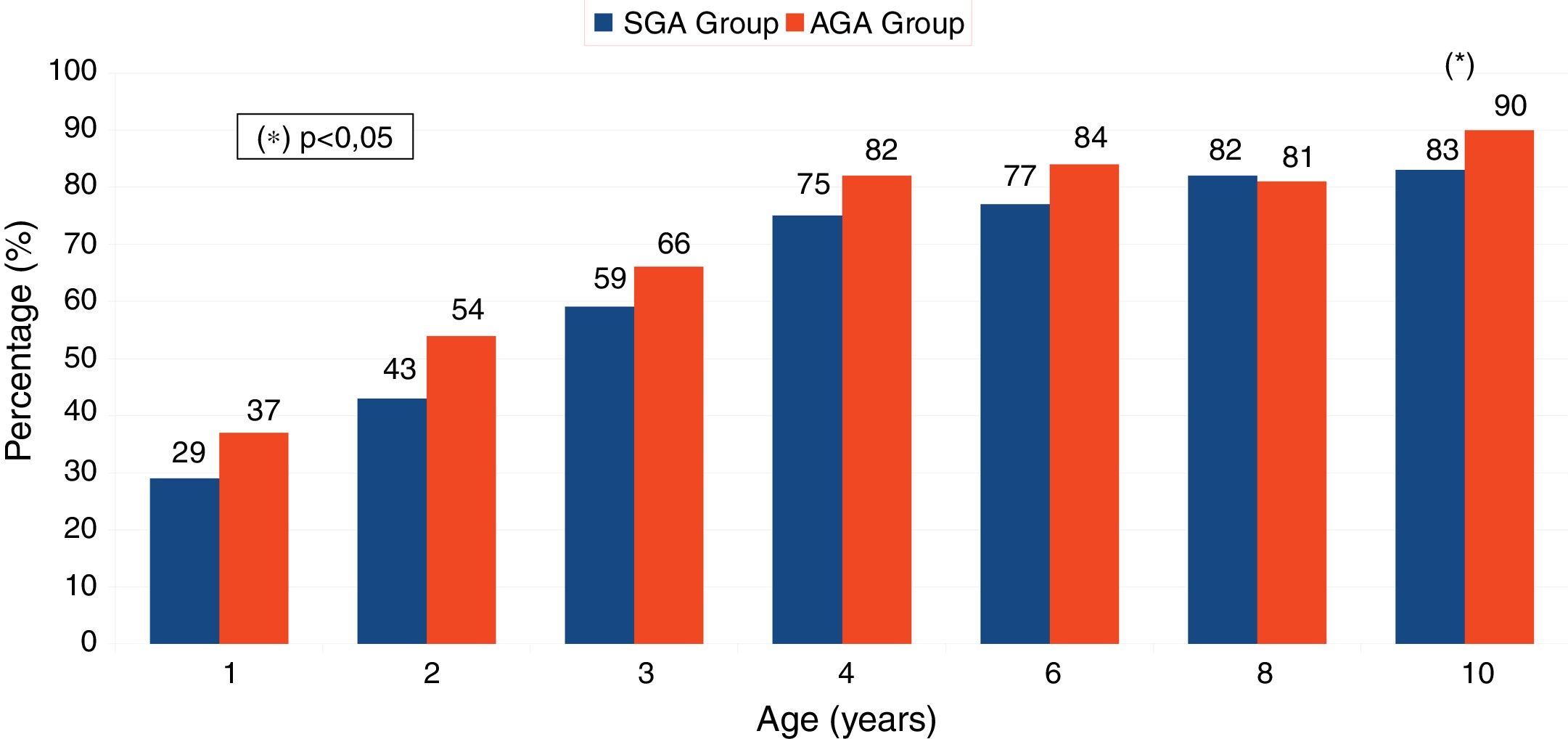
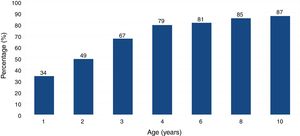
Fig. 2 presents and compares the percentages of individuals in the AGA and SGA groups that reached normal size at the different ages under consideration. We found no statistically significant differences between groups, except at age 10: 17% of children in the SGA group (n = 12) and 10% of children in the AGA group (n = 10) had low height (P = 0.018).
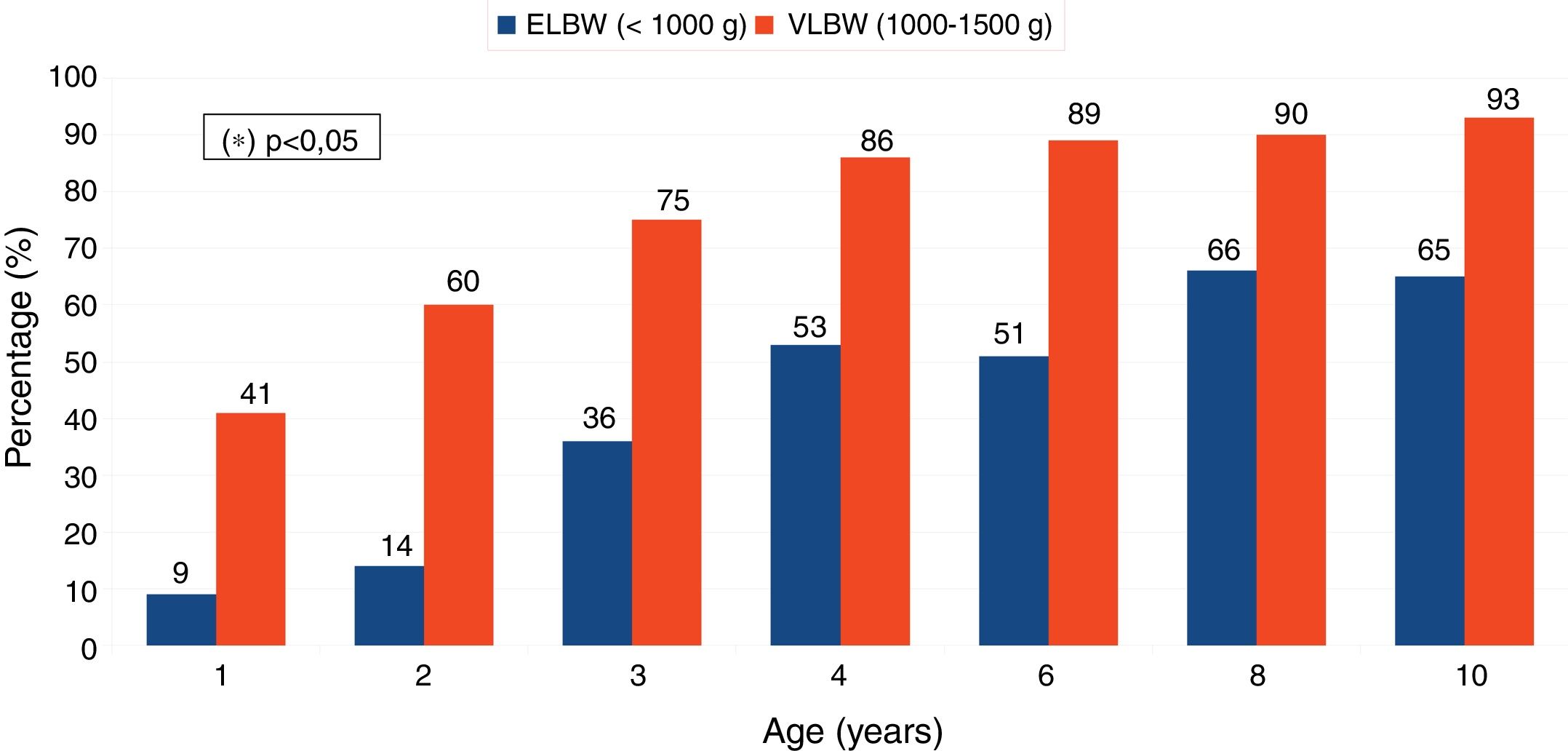
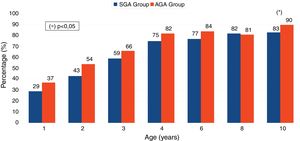
Fig. 3 presents and compares the percentages of children born with VLBW (1000–1500 g; n = 133) and children born with ELBW (<1000 g; n = 37) that achieved a normal height at the different ages under consideration. We found significant differences between groups at every age. At age 10 years, 7% of children born with VLBW (n = 9) and 35% of children born with ELBW (n = 13) had short stature (P = 0.001).
In the SGA group, of the 12 children that had short stature at age 10 years (7 of who were ELBW), 7 had achieved a normal height by age 14 years (of who 6 had undergone treatment with recombinant human growth hormone [rhGH]), while the remaining 5 out of 12 children (3 of who were ELBW) continued to have short stature (3 had undergone treatment with rhGH). Treatment with rhGH was initiated between ages 6.5 and 8.3 years.
In the AGA group, of the 10 children that had short stature at age 10 years (7 of who were ELBW) 2 had reached a normal height at 14 years (1 had received rhGH therapy at age 8.9 years) and 8 (6 of them ELBW) continued to have short stature (1 started rhGH therapy at age 7.8 years, and 7 were not eligible for treatment due to normal responses in growth hormone stimulation tests).
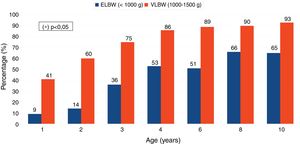
Table 2 presents the results of the multiple logistic regression analysis performed to study the association of neonatal characteristics with inadequate catch-up growth in height at ages 2, 4, and 10 years. We found that ELBW, SGA with only abnormal height and preterm birth before 28 weeks’ gestation were associated with inadequate catch-up growth in height at 2, 4, and 10 years of age. On the other hand, SGA with abnormal weight and height was associated with inadequate catch-up growth only through age 10 years, while preterm birth between 28 to 32 weeks’ gestation was associated with inadequate catch-up growth only at ages 2 and 4 years. Furthermore, multiple birth was not associated with inadequate catch-up growth at ages 2, 4 or 10 years.
Logistic regression analysis of factors associated with inadequate catch-up growth.
| Inadequate catch-up height gain | |||
|---|---|---|---|
| Age 2 yearsOR (95% CI) P | Age 4 years OR (95% CI) P | Age 10 years OR (95% CI) P | |
| Birth weight | |||
| VLBW (1000−1500 g), n = 133 | Reference group | Reference group | Reference group |
| ELBW (<1000 g), n = 37 | 8.9 (3.3–24.5) 0.001 | 5.9 (3.6–13.6) 0.001 | 5.3 (2.1–13.4) 0.001 |
| AGA group, n = 69 | Reference group | Reference group | Reference group |
| SGA group (weight/height), n = 41 | 1.6 (0.8–2.9) 0.150 | 1.5 (0.7–3.1) 0.300 | 2.6 (1.1–6.4) 0.038 |
| AGA group, n = 69 | Reference group | Reference group | Reference group |
| SGA group (only weight), n = 12 | 1.4 (0.7–2.7) 0.291 | 1.3 (0.6–2.9) 0.457 | 2.3 (0.9–5.5) 0.069 |
| AGA group, n = 69 | Reference group | Reference group | Reference group |
| SGA group (only height), n = 16 | 2.0 (1.3–1.7) 0.048 | 1.9 (1.2–4.0) 0.033 | 2.8 (1.1–6.8) 0.024 |
| Type of pregnancy | |||
| Single, n = 98 | Reference group | Reference group | Reference group |
| Multiple, n = 72 | 0.9 (0.5–1.5) 0.620 | 0.9 (0.4–1.9) 0.862 | 1.4 (0.6–3.6) 0.431 |
| Gestational age at birth | |||
| 32–37 weeks (LPT), n = 66 | Reference group | Reference group | Reference group |
| <28 weeks (EPT), n = 72 | 2.5(1.1–5.9) 0.035 | 7.2(2.6–19.8) 0.001 | 4.5(1.3–14.9) 0.015 |
| 28–32 weeks (VPT), n = 32 | 2.6(1.1.6.4) 0.033 | 4.2(1.6–10.8) 0.003 | 1.9(0.7–5.3) 0.242 |
AGA, appropriate for gestational age; ELBW, extremely low birth weight; EPT, extremely preterm; LPT, late preterm; SGA, small for gestational age; VLBW: very low birth weight; VPT, very preterm.
Foetal development and growth are complex processes based on continuous and harmonious cellular proliferation and differentiation. The literature describes multiple factors (maternal, foetal, placental and environmental) that have a deleterious impact on the foetus and trigger a series of functional and structural adaptive changes that result in restricted foetal growth (in what is known as the “thrifty phenotype hypothesis”), accompanied by several changes in hormone sensitivity and/or secretion associated with an increased risk of developing metabolic and/or endocrine disorders in adult life.12,13 Nevertheless, after birth, most infants born to term with a history of intrauterine growth restriction exhibit an accelerated compensatory growth (catch-up growth), especially in the first year of life, that allows approximately 90% to exceed the threshold of 2 SDs below the mean in the reference population, or, in other words, to reach a normal height.2–4 However, when this compensatory growth does not take place, they are not likely to achieve a normal final height in adulthood. This is one of the indications for rhGH therapy approved by the United States Food and Drug Administration (FDA), the European Medicines Agency (EMA) and the Growth Hormone Research Society, whose aim is to accelerate the initial compensatory growth and/or to maintain a normal growth velocity.3,14,15
Advances in obstetric and perinatal care in recent decades have achieved a substantial decrease in the mortality of VLBW infants; however, given the potential sensorineural morbidity in this population, these patients are usually included in follow-up programmes whose purpose is the early detection of neurodevelopmental problems.1,16 The optimization of these programmes has facilitated the standardization of dietary and nutritional recommendations, and allowed growth monitoring in the first years of life. It also allows the analysis, such as the one performed by our group, of the evolution of anthropometric variables in VLBW infants.
Our study shows that catch-up height gain in VLBW infants is either lesser or slower compared to infants born full-term and SGA.4–10 In fact, at ages 2, 4 and 10 years, 50.6%, 21.1% and 12.9% of children in our sample, respectively, still had short stature; therefore, while a similar proportion of VLBW infants achieved a normal height compared to full-term SGA infants at age 2, between ages 4 and 10 years barely 8.2% of VLBW infants achieved a normal height. Although these data may seem contradictory, the results are somewhat consistent with those reported by different authors that had already warned of a potential delay in the catch-up growth of VLBW infants.17–23 However, none of these authors have analysed the impact of catch-up weight gain, which is concurrent with catch-up height gain and, based on the obtained data, seems to play a determinant role.8,9 In fact, almost all children that had achieved a normal height by the check-ups at ages 2, 4 and 10 years had a normal weight in the preceding check-up. Thus, VLBW infants should be subject to strict nutritional monitoring, possibly with prescription of nutritional supplements, with the aim of achieving complete catch-up growth in weight as early as possible.
The findings of our study have immediate clinical repercussions. First, the comparison of the patterns of catch-up height gain in AGA and SGA groups showed only small differences in the age range under study, except at age 10. However, at age 10, while only 1 out of the 10 children did not reach a normal height in the AGA group, approximately 1 in 5 individuals in the SGA group continued to have short stature. This means that the lower rate or slower pace of catch-up growth in VLBW infants is slightly further reduced or delayed in SGA infants. On the other hand, it is also important to highlight that between ages 2 and 4 years, 1 in 3 children achieved a normal height in both the AGA and the SGA groups. This finding suggests that applying the recommendation of the EMA and the Growth Hormone Research Society of postponing initiation of rhGH therapy until age 4 years would be more appropriate than applying the recommendation of the FDA, which proposes initiation of treatment at age 2 years.
The analysis of catch-up growth in ELBW infants deserves special consideration. On one hand, we found that most children that had not reached a normal height by age 10 years in both the AGA and the SGA groups were patients born with ELBW. On the other hand, there was a remarkable number of children in the AGA group who, in agreement with the current recommendations of the FDA, the EMA and the Growth Hormone Research Society, did not receive hormone therapy when the response to the growth hormone stimulation test was normal. This may largely explain why children in the AGA group with short stature at age 10 years (most of who were VLBW) continued to have short stature at age 14 years and, presumably, in adulthood. Given that current guidelines do not consider the possibility of starting growth hormone therapy in individuals born AGA and with normal GH secretion, we should consider whether these criteria should be modified in the case of children born with VLBW and, specially, those with ELBW. The multiple logistic regression analysis confirmed that ELBW and EPT infants were at higher risk of inadequate catch-up height gain at 2, 4, and 10 years of age, associated with an increased risk of short stature in adulthood. These findings support the hypothesis that they could benefit from GH treatment, regardless of whether their birth weight and/or length was appropriate for gestational age or not.6,24–26
The growth pattern of children born preterm has specific characteristics. Approximately 85% and 53% of VLBW and ELBW infants, respectively, will have reached a normal height by 4 years of age. However, those with short stature at age 4 years are not likely to reach a normal height in childhood. Catch-up weight gain seems to be an important factor for catch-up height gain, and therefore we recommend a rigorous nutritional follow-up in these children. If despite this follow-up these children do not exhibit improved catch-up height gain, they may be eligible for rhGH therapy.
Declaration of Competing InterestThe authors declare no conflicts of interest.
Author contributionsTDT and ISG participated in the study design and the analysis of the data, and wrote the first draft of the manuscript. FGV, MJCG and SBZ participated in the collection and analysis of data. All authors contributed to the writing of the manuscript and approved its final version.
Please cite this article as: Durá-Travé T, et al. Crecimiento recuperador y factores asociados en niños de muy bajo peso al nacer. An Pediatr (Barc). 2020;93:282–288.