Body mass index-for age (BMI) and tri-ponderal mass index-for-age (TMI) values of healthy non-underweight, non-obese millennial children have not been reported until now. We aimed to obtain these values.
Subjects and methodsLongitudinal growth study (1995–2017) of 1,453 healthy non-underweight, non-obese millennial children, from birth (n=477) or from 4 years of age (n=976) to 18 years in girls and 19 years in boys (25,851 anthropometric measurements).
ResultsIn each sex, mean BMI-for-age values increased from birth to one year, declined until 5 and increased from then onwards. Mean TMI-for-age values decreased abruptly during the first 6 years of age and slowly thereafter, in both sexes. Although, at some ages, mean BMI-for age values differed statistically between sexes, differences were scant and of poor clinical significance. The same occurred for TMI-for-age values. BMI-for-age cut-off values to define underweight status (−2 SD) were similar to those proposed by Cole and the WHO for both sexes. However, BMI-for-age cut-off values to define obesity (+2 SD) were lower in both sexes (1.0–5.3) than those proposed by Cole and similar to those proposed by the WHO until 12 in girls and 14 in boys and lower (1.0–4.8) from these ages onwards.
ConclusionsBMI-for-age and TMI-for-age values of healthy non-underweight, non-obese millennial children are provided. No clinically relevant differences were observed between sexes. These values may be used to measure underweight status and obesity in present pediatric populations and to evaluate the relationship between BMI-for-age and TMI-for-age in a clinical setting.
Hasta el momento no se han comunicado valores del índice de masa corporal (IMC) ni del índice de masa triponderal (IMT) de niños sanos sin malnutrición ni obesidad de la generación del milenio. Nuestro objetivo fue obtener estos valores.
Sujetos y métodosEstudio longitudinal de crecimiento (1995-2017) en 1.453 niños sanos sin malnutrición ni obesidad de la generación del milenio desde el nacimiento (n = 477) o los 4 años de edad (n = 976) hasta los 18 años en mujeres y los 19 años en varones (25.851 mediciones antropométricas).
ResultadosEn ambos sexos, los valores medios del IMC según la edad aumentaron entre el nacimiento y el año de edad, luego decrecieron hasta los 5 años de edad y finalmente aumentaron a partir de dicha edad. Los valores del IMT según la edad descendieron abruptamente en los 6 primeros años de vida y lentamente a partir de esa edad en ambos sexos. Aunque a algunas edades los valores medios del IMC difirieron de manera significativa entre los sexos, esas diferencias fueron pequeñas y de escasa relevancia clínica. Lo mismo ocurrió con los valores del IMT según la edad. Los puntos de corte del IMC según la edad obtenidos para definir la malnutrición (−2 DE) fueron similares a los propuestos por Cole y la OMS en ambos sexos. En cambio, los puntos de corte del IMC según la edad obtenidos para definir la obesidad (+2 DE) fueron menores en ambos sexos (1,0-5,3) en comparación con los propuestos por Cole y similares a los propuestos por la OMS hasta los 12 años en niñas y los 14 en niños, e inferiores (1,0-4,8) a los de la OMS a partir de dichas edades.
ConclusionesPresentamos valores del IMC y el IMT según la edad de niños sanos sin malnutrición ni obesidad de la generación del milenio. No se observaron diferencias significativas entre los 2 sexos. Estos valores podrían emplearse para evaluar la malnutrición y la obesidad en poblaciones pediátricas actuales y para estudiar la relación entre el IMC y el IMT (según la edad) en la práctica clínica.
Body mass index (BMI) (weight/height2) is used to measure underweight status and obesity in children and adolescents.1–8 However, exactly which BMI-for-age reference values should be used is a matter of debate. Today's BMI-for-age reference data are from cross-sectional growth studies which included obese and non-obese children,8–15 or were based on surveys carried out the last century, except for WHO reference values for the first five years of life.16–20 Thus, there is a lack of data coming from present healthy non-underweight and non-obese pediatric populations, which can be used as reference values.
Recently, it has been reported that the tri-ponderal mass index (TMI) (weight/height3)1,21 estimates body fat levels more accurately than BMI in children aged 8–17 years and it has been suggested to replace BMI z score values with TMI values.22
We aimed to obtain BMI-for-age and TMI-for-age (birth to 18 years of age in girls and 19 years of age in boys) reference values of healthy non-underweight and non-obese millennial children included in the Barcelona longitudinal growth study (1995–2017). In addition, as pubertal growth (height and weight gain rates) significantly differs according to age at pubertal growth spurt onset (PGSO),23–25 we also aimed to learn if the same occurs for BMI-for age and TMI-for age values.
Subjects and methodsThe study group comprised 1,908 healthy children of the middle-to-upper socioeconomic district of Barcelona. Over the study period, 132 children were ruled out for obesity (physical examination and BMI >2.0 SDS of age- and sex-matched controls12 and 323 were lost. Thus, 1,453 (743 girls, 710 boys) who reached adult height between January 2012 and March 2017 completed the study and data from their 25,851 length/height and weight measurements (12,818 in girls; 13,033 in boys) were analyzed. Adult height (growth velocity <1cm/year in two, 6–12 months, consecutive intervals) was reached by the age of 17 in all girls and by the age of 19 in all boys.25
Population A (239 girls, 238 boys) was followed at four pediatric practices and data from their length/height and weight measurements were recorded from birth to 18 years of age in girls and 19 years of age in boys; birth weight and length were adequate for their gestational age.26 Population B (504 girls; 472 boys) was followed at four schools and data from their height and weight measurements were recorded from 4 years of age to 18 years in girls and 19 years in boys. No chronic diseases, chronic drug therapies or underweight (BMI values <−2.0 SDS, age- and sex-matched controls12 were documented in either population.
Length/height and weight were recorded every 6–12 months by four researchers in population A and once a year by one of the four in population B, as reported previously.12,24 Length was measured during the first two years of life with a rigid infantometer, after which rigid wall-mounted stadiometers were used in population A and a portable rigid stadiometer in population B. Stadiometers were calibrated similarly throughout the study. Weight was recorded with a baby scale for the first 18 months of age and with a digital floor scale thereafter (population A in underwear; population B in T-shirt and skirt/trousers, the estimated weight of the T-shirt and skirt/trousers was subtracted from the overall weight). Measurements were taken to the nearest 0.1 centimeter (cm) for height and 0.1 kilogram (kg) for weight. BMI (kg/m2) and TMI (kg/m3) were calculated for each anthropometric measurement.
The anthropometric growth program “Auxolog” based on data from our previous longitudinal growth study24,27 was used to construct BMI-for-age and TMI-for-age growth charts for each child. Children were considered very-early, early, intermediate, late and very-late matures according to their age at pubertal growth spurt onset.24,25 In each sex, mean BMI-for-age and TMI-for-age values were calculated for the whole population and for each of the five pubertal maturity groups.
EthicsThe study was approved by the Ethics Committee of the University Children's Hospital Vall d’Hebron, Barcelona. Informed consent was obtained from children and their parents or legal guardians.
Statistical analysisResults are expressed as mean±SD. Student’ t-test was used for comparisons of mean anthropometric-for-age values between sexes, and one-sample Student’ t-test for comparisons of mean anthropometric-for-age values of the whole population with each one of the five pubertal maturity groups in both sexes. SAS® 9.3 software (SAS Institute Inc., Cary, NC, USA) was used to analyze the data.
ResultsFor both sexes, in the whole population and in each of the five pubertal maturity groups, mean BMI-for-age values were similar and did not differ statistically between populations A and B (data not shown). The same occurred for mean TMI-for-age values (data not shown). Thus, for each sex, joint data of both populations were analyzed as a single population.
According to age at PGSO the 743 girls were considered: very-early matures (8–9 years, n=119), early matures (9–10 years, n=157), intermediate matures (10–11 years, n=238), late matures (11–12 years, n=127) and very-late matures (12–13 years, n=102). According to age at PGSO the 710 boys were considered: very-early matures (10–11 years, n=110), early matures (11–12 years, n=139), intermediate matures (12–13 years, n=225), late matures (13–14 years, n=133) and very-late matures (14–15 years, n=103).
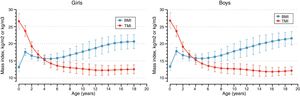
Body mass indexIn both sexes, mean BMI-for-age values of the whole population increase from birth to 1 year of age, decline thereafter until 5 years of age and increase progressively from then on to 18 years in girls and 19 years in boys (Fig. 1). Girls and boys had similar BMI-for-age values, although statistically-significant differences were observed at some ages (p<0.01 at 1, 4, 15, 16, 17 and 18 years). The greatest differences were observed at 18 years of age (0.7; 3.3%) (Table 1).
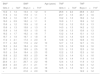
Body mass index-for-age (BMI) and tri-ponderal mass index-for-age (TMI) values (mean±SD).
| BMIa | BMIa | Age (years) | TMIb | TMIb |
|---|---|---|---|---|
| Girls n=743c | Boys n=710c | Girls n=743c | Boys n=710c | |
| 13.2±1.4 | 13.4±1.2 | 0 | 26.6±2.2 | 26.8±2.3 |
| 17.6±1.0 | 17.9±1.1 | 1 | 23.7±1.5 | 23.7±1.6 |
| 16.5±1.0 | 16.7±1.1 | 2 | 19.2±1.3 | 19.2±1.4 |
| 16.0±0.9 | 16.2±1.1 | 3 | 16.9±1.1 | 16.9±1.2 |
| 15.6±1.2 | 15.9±1.2 | 4 | 15.2±1.2 | 15.3±1.3 |
| 15.6±1.3 | 15.8±1.3 | 5 | 14.3±1.3 | 14.2±1.2 |
| 15.8±1.4 | 15.9±1.5 | 6 | 13.6±1.3 | 13.6±1.3 |
| 16.2±1.7 | 16.2±1.6 | 7 | 13.2±1.4 | 13.1±1.3 |
| 16.7±1.9 | 16.7±1.8 | 8 | 13.0±1.4 | 12.9±1.4 |
| 17.2±2.1 | 17.3±2.0 | 9 | 12.8±1.5 | 12.8±1.5 |
| 17.7±2.2 | 17.9±2.2 | 10 | 12.7±1.5 | 12.7±1.5 |
| 18.2±2.4 | 18.4±2.4 | 11 | 12.5±1.6 | 12.6±1.6 |
| 18.7±2.4 | 18.9±2.5 | 12 | 12.3±1.5 | 12.5±1.6 |
| 19.3±2.4 | 19.4±2.5 | 13 | 12.2±1.5 | 12.3±1.6 |
| 19.8±2.2 | 19.9±2.5 | 14 | 12.3±1.4 | 12.1±1.6 |
| 20.2±2.1 | 20.3±2.3 | 15 | 12.4±1.4 | 11.9±1.4 |
| 20.4±2.1 | 20.7±2.2 | 16 | 12.4±1.3 | 11.9±1.3 |
| 20.6±2.0 | 21.1±2.1 | 17 | 12.4±1.3 | 12.0±1.2 |
| 20.7±2.0 | 21.4±2.0 | 18 | 12.5±1.3 | 12.1±1.2 |
| – | 21.6±2.0 | 19 | – | 12.2±1.2 |
BMI-for-age cut-off values of the whole population to define underweight (−2 SD) were similar to those proposed by Cole TJ and the WHO for both sexes.16,20 However, BMI-for-age cut-off values to define obesity (+2 SD) were lower in both sexes than those proposed by Cole TJ (1–18 years),19 similar to those proposed by the WHO up to the age of 12 in girls and 14 in boys and lower from these ages onwards.17,18,20 Differences ranged from 1 to 5.3 with Cole TJ values and from 1 to 4.8 with WHO values.
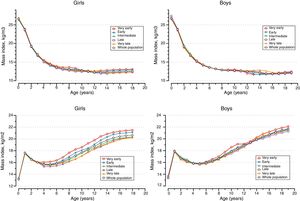
In both sexes, mean BMI-for-age values for each one of the five pubertal maturity groups were similar to those of the whole population (Fig. 2), although statistically-significant differences (range: 0.3–0.8, p<0.05 to p<0.001) were observed at some ages (data not shown). The greatest differences were observed between the very-early group and the whole population: in girls from 8 to 14 years (0.8; 4.2%) p<0.001, and in boys at 18 years (0.7; 3.7%) p<0.001.
Tri-ponderal mass indexIn both sexes, mean TMI-for-age values of the whole population decreased abruptly during the first six years of age and slowly from then on to 18 years in girls and 19 years in boys (Fig. 1). TMI-for-age values were similar in both sexes, although statistically significant differences (p=0.032 at 12 and 14 years and p<0.001 at 15, 16, 17 and 18 years) were observed. The greatest differences (0.5; 4%) were found at 15, 16, 17 and 18 years of age (Table 1).
In both sexes, mean TMI-for-age values for each one of the five pubertal maturity groups were similar to those of the whole population (Fig. 2), although statistically significant differences (range: 0.2–0.5, p<0.05 to p<0.001) were observed at some ages (data not shown). The greatest differences (0.5; 4.0%) were observed between the very-early group and the whole population at 8 years of age in girls and at 14 and 15 years of age in boys.
DiscussionCurrent BMI reference data to measure underweight status and obesity in children and adolescents came from cross-sectional growth studies which included obese and non-obese subjects,8–15 or were based on surveys carried out in the 19th century, except for WHO reference values for the first five years of life.16–20 Thus, there is a lack of data coming from present healthy millennial non-underweight and non-obese pediatric populations, which can be used as reference values to measure underweight and overweight status and obesity in the present pediatric populations.
Although TMI-for-age values1,21,22 are not currently used to measure underweight status and obesity in children and adolescents, a recent work has underlined that TMI values estimate body fat levels more accurately than BMI in non-Hispanic white children aged 8–17 years and recommended the use of TMI values instead of BMI z score values. However, as the authors pointed out, this work needs to be extended to other racial/ethnic groups and then replicated in large cross-sectional and longitudinal studies.22 Age-and-sex reference data of healthy non-underweight and non-obese millennial children have not been reported until now.
Herein, we report BMI-for-age and TPI-for-age values of 1453 healthy non-underweight and non-obese children, followed in a longitudinal study from birth (n=477) or from 4 years of age (n=976) to adult height, which was reached between January 2012 and March 2017 and in whom the anthropometric measurements were taken by only four researchers using similarly adjusted equipment The study was designed with the aim of reducing the anthropometric values dispersion observed in growth studies owing to the heterogeneity of the populations evaluated, the number of researchers involved and the equipment used.
Although a bias in our results can completely not be rule out, they represent the BMI-for-age and TMI-for-age values distribution of 1,453 healthy non-underweight and non-obese millennial children in whom 25,851 anthropometric measurement were recorded and in whom prepubertal and adult height25 were similar to those of the current BMI reference data used to measure underweight status and obesity in children and adolescents.8–19 This suggests that our data may be considered as a reference to measure underweight status and obesity in present pediatric populations. Their clinical use may confirm or deny this assumption.
Mean BMI-for age values tended to differ between sexes, at some ages; however, differences were scant and of poor clinical significance. The same occurred for TMI-for-age values. This suggests that the differences observed in weight-for-age values between both sexes were mainly related to the corresponding differences in height-for-age values25, and that this resulted in similar BMI-for-age and TMI-for-age values, which concur with the fact that non-underweight and non-obese children were included in our study. Our data also suggest that BMI-for-age values could be evaluated using the same reference-for-age values for both sexes. The same occurred for TMI-for-age values.
While our BMI-for-age cut-off values to define underweight status (−2 SD) were similar to those proposed by Cole TJ and the WHO for both sexes16–18 our BMI-for-age cut-off values to define obesity differed in pubertal and adolescent years from those proposed by Cole TJ19 and the WHO.17,18,20 Whether differences among the populations evaluated (present day vs. last century), secular growth9–15 and pubertal onset acceleration25,28–30 or other methodological aspects could explain the differences among these studies would be a matter of discussion.
In both sexes, pubertal growth spurt onset occurs over a five years-period23–25 and it is a critical milestone determining growth rate (height and weight gains) of pubertal period, Tanner's stages development and, in girls, age at menarche and growth from menarche to adult height. Although, at some ages, mean BMI-for-age values tended to differ between the whole population and the very-early maturity pubertal group, differences were scant and of poor clinical significance. Each pubertal maturity group had a BMI-for-age pattern similar to that of the whole population. The same occurred for mean TMI-for-age values. This suggests that, in both sexes, the differences observed in weight-for-age values among the five pubertal maturity groups were mainly related to the corresponding differences in height-for-age values25, and that this resulted in similar BMI-for-age values, which support the fact that non-underweight and non-obese children were included in our study. The same occurred for TMI-for-age values.
In summary, BMI-for-age and TMI-for-age reference values of healthy non-underweight and non-obese millennial children are provided for the first time, as far as we know. No pertinent and not clinically relevant differences were observed between sexes for BMI-for-age and for TMI-for age values. These values may be helpful for clinical evaluation of thinness and obesity during infancy, childhood and adolescence in present pediatric populations, and may contribute to confirm or deny the suggested use of TMI-for-age values instead of BMI-for-age z score values in a clinical setting.
AddendumCharts for BMI-for-age and TMI-for-age values calculated by the LMS method will be available (centiles and SDS values) and downloaded free of charge from the web site: http://www.millennialsgrowth.com (available February 2018) (Cole TJ. The LMS method for constructing normalized growth standards. Eur J Clin Nutr 1990;44:45–60).
FundingThis research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Conflict of interestsThere is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
We would like to thank the children, parents, schools and teachers who made this study possible. We would also like to thank the Scientific Societies (Spanish and Catalan Pediatric Societies, Spanish Pediatric Endocrinology Society) and Institutions which back this work. Juan Bosch-Castañé MD and Ariadna Campos PhD are acknowledged for their contribution to the work. Christine O’Hara and Fidelma Greaves are acknowledged for useful help with the English version of the manuscript.
Please cite this article as: Carrascosa A, Yeste D, Moreno-Galdó A, Gussinyé M, Ferrández Á, Clemente M, et al. Índice de masa corporal e índice de masa triponderal de 1.453 niños no obesos y sin malnutrición de la generación del milenio. Estudio longitudinal de Barcelona. An Pediatr (Barc). 2018;89:137–143.