Children’s diffuse lung diseases, also referred to as interstitial lung diseases, are a group of more than 200 uncommon entities involving the interstitial bed, alveolar structure and exchange membrane, with an estimated prevalence of less than 1 case per 100 000 children.1 These diseases share clinical and radiological characteristics, which makes aetiological diagnosis challenging. When the aetiology is unknown, they are grouped under the umbrella of children's interstitial lung disease (chILD).2
We present the case of a female neonate born at term with adequate weight for gestational age following an uncomplicated pregnancy with prenatal care. The birth was spontaneous and not assisted, with delivery in water in a birthing tub in a private secondary care hospital. Immediately after the birth, during which the infant’s head was submerged, the baby had a coughing fit before the first cry. Subsequently, she developed progressive respiratory distress, ultimately requiring respiratory support with continuous positive airway pressure for 5 days. The chest X-ray in the first hours of life showed infiltrates in the middle and lower lobes of the right lung.
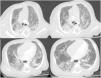
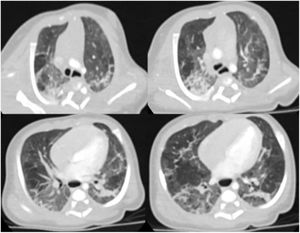
If diffuse lung disease is suspected, as was the case in this patient, the Sociedad Española de Neumología Pediátrica (Spanish Society of Paediatric Pulmonology) recommends expanding the evaluation, starting with performance of a computed tomography (CT) scan of the chest.3 In this case, on account of the persistence of tachypnoea and hypoxaemia, a chest CT scan was performed at 26 days post birth, which evinced features compatible with interstitial lung pattern (Fig. 1).
Given the suspicion of diffuse lung disease, the assessment was completed with performance of fibreoptic bronchoscopy with bronchoalveolar lavage and genetic testing for pulmonary disease, which evinced no abnormalities.
From 1 month post birth, the patient showed progressive improvement, becoming free of respiratory symptoms and with full resolution of radiological abnormalities. Her supplemental oxygen needs decreased gradually to its full withdrawal at 1 month of life.
The rapid resolution of clinical and radiological features rules out other aetiologies of diffuse lung disease, which, combined with the history of waterbirth and cough before the first cry, suggests a diagnosis of exclusion of probable interstitial lung disease secondary to aspiration pneumonitis in the context of waterbirth.
Previous publications have associated waterbirth with the development of neonatal respiratory distress and aspiration interstitial pneumonitis. The main hypothesis is that during waterbirth, the diving reflex may be abolished in compromised foetuses and newborns, with an impact chiefly on the lungs.4,5
In the neonatal period, diffuse lung diseases frequently manifest with respiratory distress and an alveolar-interstitial pattern in the chest radiograph. They may also manifest with cough, tachypnoea, progression to severe respiratory distress and faltering growth.6
The prognosis is good, with favourable outcomes with near-full resolution of symptoms within 2 years post birth. Some cases require prolonged respiratory support or steroid therapy.
The case presented here evinces a probable aetiology that has emerged recently and should be taken into account in the differential diagnosis of diffuse lung disease in children. Further studies are required to assess the risk of aspiration pneumonia associated with waterbirth and its potential long-term clinical repercussions.
Previous presentation: This study has been presented as a poster with short communication at the XLIII Annual Meeting of the Sociedad Española de Neumología Pediátrica, May 6–7, 2022, Jerez de la Frontera, Spain.