Familial Mediterranean fever (FMF) is the most prevalent autoinflammatory disease (AD) with a known genetic basis. All ADs involve alterations in innate immunity with inflammasome dysfunction. The inheritance pattern of FMF is autosomal recessive, although there are descriptions of a few mutations that show an autosomal dominant behaviour. The mutations are located in the MEVF gene, which encodes the pyrin protein, also known as marenostrin. There is a high incidence of FMF in populations along the Mediterranean coast (Jews, Arabs, Armenians and Turks). Onset occurs before 20 years of age in 80% of the cases. Attacks are characterised by fever and serositis or synovitis and last 1–3 days. The most widely criteria used for its diagnosis are the Tel Hashomer criteria (Table 1), based on which diagnostic criteria for children have been proposed. The first-line treatment is colchicine, both to avoid the occurrence of attacks and to prevent amyloidosis, or even partially revert it once it has established. Amyloidosis is the most frequent long-term complication.1
Tel Hashomer criteria for the diagnosis of familial Mediterranean fever.
| Major | Minor | Supportive criteria |
|---|---|---|
| Typical attacksa: | 1–3 incomplete attacks in 1 or more of the following: | 1. Family history of FMF |
| 1. Peritonitis (generalised) | 1. Abdomen | 2. Ethnic origin associated with FMF |
| 2. Pleuritis (unilateral) or pericarditis | 2. Chest | 3. Age <20 years at disease onset |
| 3. Monoarthritis (hip, knee, ankle) | 3. Joint | 4–6 features of attacks: |
| 4. Fever alone | 4. Exertional leg pain | 4. Severe: requiring bed rest |
| 5. Favourable response to colchicine | 5. Spontaneous remission | |
| 6. Symptom-free interval | ||
| 7. Transitory elevated acute-phase reactants (leukocytes, ESR, SAA and/or fibrinogen) | ||
| 8. Episodic proteinuria/haematuria | ||
| 9. Unproductive laparotomy or removal of white appendix | ||
| 10. Consanguinity of parents |
The diagnosis requires at least 1 major criterion or 2 minor criteria, or at least 1 minor criterion plus 5 or more supportive criteria, or at least 1 minor criterion and 4 criteria of the first 5 supportive criteria.
ESR, erythrocyte sedimentation rate; FMF, familial Mediterranean fever; SAA, serum amyloid A.
In FMF, arthritis is usually acute, oligoarticular and non-erosive, and affects large joints in the lower limbs, especially knees and ankles.1,2 In this paper, we present two children with FMF in whom arthritis was the main clinical feature.
Case 1The patient was a 5-year-old Caucasian girl that presented with bilateral inguinal pain of 4 days of duration and low-grade fever. There was no history of trauma.
The most relevant finding of the physical examination was pain, with the patient assuming an antalgic position with the right hip flexed in external rotation. Mobility was limited in both hips. There was a faint erythematous exanthem at the upper region of the lower limbs.
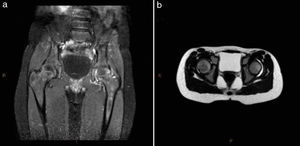
The patient was admitted for suspected septic arthritis of the hip, and empirical antibiotic treatment with cefotaxime and clindamycin was initiated. An ultrasound scan was performed that revealed bilateral effusion in the coxofemoral joints. At admission, complete blood count was normal, C reactive protein (CRP) level was 172mg/L and erythrocyte sedimentation rate (ESR) was 94mm/h. Arthrocentesis was performed to collect joint fluid, which had 32,000cells/mm3 with 90% of polymorphonuclear leukocytes. Joint fluid and blood cultures were negative. Magnetic resonance imaging did not reveal involvement of the bone or surrounding soft tissues (Fig. 1). Chest radiography, echocardiography, antistreptolysin O titre, peripheral blood smear and funduscopic exam were all normal. Rheumatoid factor, antinuclear antibodies and the Mantoux test were negative. Parvovirus, Coxiella and Brucella serology tests were negative. An intermittent fever of up to 38°C persisted in the early days, and subsequently the patient remained afebrile with improvement of hip mobility and pain, so she was discharged with oral ibuprofen and transitioned to outpatient follow-up. A year later, she developed arthritis of the left hip again, with elevated CRP (75mg/L) and intermittent low-grade fever in a self-limited course that lasted 10 days. Later on, she experienced joint inflammations that subsided after 24–48h in the ankle, proximal interphalangeal (PIP) joint and hip. Genetic testing for FMF was requested, detecting the heterozygous mutation p.A744S in exon 10 of the MEVF gene.
Case 2Caucasian girl, 13 years old, that since age 6 experienced intermittent inflammation in carpal, PIP and metacarpophalangeal joints as well as cervicalgia. Although the patient did not meet the criteria for juvenile idiopathic arthritis (JIA) because inflammation did not last more than 6 weeks, treatment with oral corticosteroids and methotrexate was initiated, with little improvement. Several relatives on the mother's side had a diagnosis of seronegative rheumatoid arthritis. Given the family history and the intermittent joint symptoms, we requested a genetic test that detected the heterozygous mutation p.E148Q in exon 2 of the MEVF gene, and the heterozygous mutation p.V726A in exon 10 of the same gene.
Familial Mediterranean fever may present as episodes of joint inflammation and be initially confused with septic arthritis or later in its course with JIA,3 as we observed in the cases we are presenting. Usually it can be distinguished in that arthritis is episodic, accompanied by fever, and leaves no sequelae, although in some cases arthritis of the hip can be chronic and destructive (5%).2 Family history, ethnicity, the detection of mutations and a favourable response to colchicine support the diagnosis of FMF.4
In published case series, arthritis has been the presenting complaint in 16% of patients with FMF, and 31–59% have had joint involvement during the course of the disease. In 70%, joint involvement was monoarticular, in 26% oligoarticular and in 4% polyarticular.2,5,6 The most frequently affected joint was the knee (63%), followed by ankles (42%), elbows (15%), wrists (17%), small joints of the hand (5–10%) and sacroiliac joints (1%).5,6
We would like to emphasise the importance of correctly diagnosing patients with arthritis as a presenting feature of FMF to avoid unnecessary tests and treatments, and to allow prompt initiation of appropriate treatment.
Please cite this article as: Camacho-Lovillo S, García-Martínez AC. Artritis como forma de presentación de fiebre mediterránea familiar. An Pediatr (Barc). 2015;83:130–132.