Polyarteritis nodosa (PAN) is a rare vasculitis that affects small and medium vessels. Its clinical manifestations are varied, ranging from mild skin changes to multisystemic forms.1 New diagnostic criteria were established in 2008,2 with diagnosis requiring histopathological abnormalities (necrotising vasculitis) or angiographic abnormalities (aneurism, stenosis or occlusion) with at least one of the following:
- 1.
Skin involvement: livedo reticularis, subcutaneous nodules, cutaneous infarction with ulcerations or minor ischaemic changes.
- 2.
Myalgia.
- 3.
Arterial hypertension (AHT): arterial systolic/diastolic pressure above 95th percentile for height.
- 4.
Peripheral sensitive neuropathy or mononeuritis multiplex of motor nerves.
- 5.
Renal involvement: proteinuria, haematuria or kidney function impairment.
Regarding the treatment randomised controlled clinical trials have not been conducted in the paediatric population. Conventional treatment includes systemic corticosteroids and cyclophosphamide for induction therapy and azathioprine for maintenance, but the literature has reported cases of patients refractory to treatment that have had good outcomes with mycophenolate, infliximab or rituximab.
We describe the cases of two girls suffering from refractory PAN that were treated with infliximab.
Case 1Girl aged 6 years with a 15-day history of artralgia, ankle arthritis and purpuric lesions (Fig. 1A–C). Laboratory findings included anaemia and thrombocytosis (haemoglobin [Hb], 11g/L; platelets, 495×109/L); C reactive protein (CRP), 236mg/L; erythrocyte sedimentation rate (ESR), 88mm; and tested negative for anti-neutrophil cytoplasmic antibodies (ANCAs). The skin biopsy results were compatible with PAN. The patient's condition worsened, as she developed fever, arthritis in knees and elbows, subcutaneous nodules (Fig. 1D) and arterial hypertension, without renal involvement. Although her skin symptoms improved with prednisone and subcutaneous methotrexate in doses of 15mg/m2/week, after 10 weeks the rest of the symptoms remained. She was treated consecutively with monthly immunoglobulin therapy, subcutaneous etanercept (0.8mg/kg/week), intravenous cyclophosphamide (500mg/m2/month) and oral azathioprine (2mg/kg/day). Each treatment regimen was maintained for two months and well tolerated by the patient, and discontinued due to ineffectiveness. After one year, treatment with infliximab was initiated (dosage, 5mg/kg at weeks 0, 2 and 6 and subsequently every 8 weeks), with a decrease in the Paediatric Vasculitis Assessment Score (PVAS) from 8 to 0 in one month, which allowed the discontinuation of prednisone at 4 months. From this point, the patient remained asymptomatic and without adverse effects attributable to the treatment. Treatment with infliximab was discontinued after three years.
Skin lesions in case 1. (A) Painful swelling in left ankle with purpuric lesions in the anterior surface. (B) Livedo reticularis with haemorrhagic suffusion in the external lateral surface of the right ankle. (C) Isolated purpuric lesions in the buttocks. (D) Skin nodule in the fifth finger of the right hand.
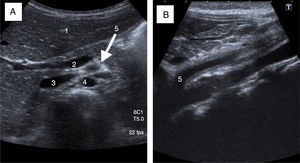
A 5-year-old girl of Moroccan descent, presenting with fever and abdominal pain of one month's duration, whey-faced, anaemia (Hb: 8.1g/L), thrombocytosis (platelets, 582×109/L); CRP, 178mg/L; ESR, 101mm; the patient tested negative for ANCAs. Abdominal ultrasound showed a thickening of the superior mesenteric artery wall with a normal but narrowed lumen compatible with arteritis (Fig. 2), confirmed by computed tomography angiography. The screening for infectious diseases was negative and other vascular diseases were ruled out. The symptoms resolved spontaneously in one week. Four months later, the patient had a similar episode, familial Mediterranean fever was excluded and treatment with prednisone was initiated. Six months later the patient developed painful erythematous nodules in the lower limbs, the biopsy of which confirmed the presence of necrotising vasculitis. Although subcutaneous methotrexate was added to the regimen (15mg/m2/week), the patient had two more episodes within 12 months, so treatment with oral azathioprine was initiated (2mg/kg/week), to which the patient responded favourably and without adverse effects. After eight months without prednisone, she had several flares of disease, so therapy was switched to intravenous infliximab (5mg/kg) given at weeks 0, 2, 6 and subsequently every 8 weeks. The PVAS decreased from 5 to 0 in one month. At present, after 24 months of treatment, the patient has only experienced post-infusion headaches and two mild episodes that resolved with prednisone.
Superior mesenteric artery (SMA) arteritis assessed by ultrasound (case 2). (A) Sagittal view: hyperechoic halo around the SMA due to thickening of its wall. 1: liver parenchyma; 2: spleno-portal axis; 3: inferior vena cava; 4: aorta; 5: SMA. (B) Coronal view: 2mm thickening of SMA from its origin in the aorta to its bifurcation (4.3cm).
Polyarteritis nodosa is rare in childhood, and its incidence peaks at 10 years. The most common sites of involvement are the skin, joints, peripheral nerves, gastrointestinal tract and kidneys.1 Gastrointestinal involvement, while reported in 23–60% of patients3 in isolation or at presentation (case 2), is rare.
Diagnosis requires compatible biopsy results,2 so it can be delayed in patients with lesions that are hard to access (case 2). Angiography is an alternative option in these patients, although it was not performed in the case presented here.
The lack of clinical trials and the variability of clinical manifestations make it difficult to choose a treatment. While anti-TNFα agents have revolutionised the treatment of various autoimmune diseases, their efficacy in the treatment of vasculitis has not been demonstrated.4 The largest case series in the paediatric age group corresponds to a study by Eleftheriou et al.5 that comprised 25 patients with vasculitis (11 with PAN). Of the PAN patients, 8 received infliximab, and their mean vasculitis activity score decreased from 8 to 3. The PVAS6 scale has been recently validated for the routine assessment of disease outcome and response to treatment.
A new autoinflammatory syndrome caused by a PAN-like vasculopathy has been recently described that is characterised by early infarctions and caused by mutations in the gene which encodes adenosine deaminase 2 (ADA2), in which treatment with anti-TNF agents was shown to be effective. Specific genetic testing has yet to be performed in our two patients to rule out this disease, which would account for their excellent response to infliximab.
The prognosis of PAN depends on the degree of visceral involvement, but overall it is better in children than in adults, with mortality ranging between 1.1% and 10%.
To conclude, while there is little data on the efficacy of infliximab in children, and multicentre studies still need to be conducted, infliximab can be used as an alternative therapy in refractory cases.
The authors thanked Dr. Purificación Moreno, who was in charge of the initial followup of these patients.
Please cite this article as: Núñez Cuadros E, Galindo Zavala R, Díaz Cordovés-Rego G, Vera Casaño V, Urda Cardona AL. ¿Son realmente útiles los anti-tnfα en vasculitis sistémicas? Experiencia en panarteritis nodosa. An Pediatr (Barc). 2015;83:350–352.