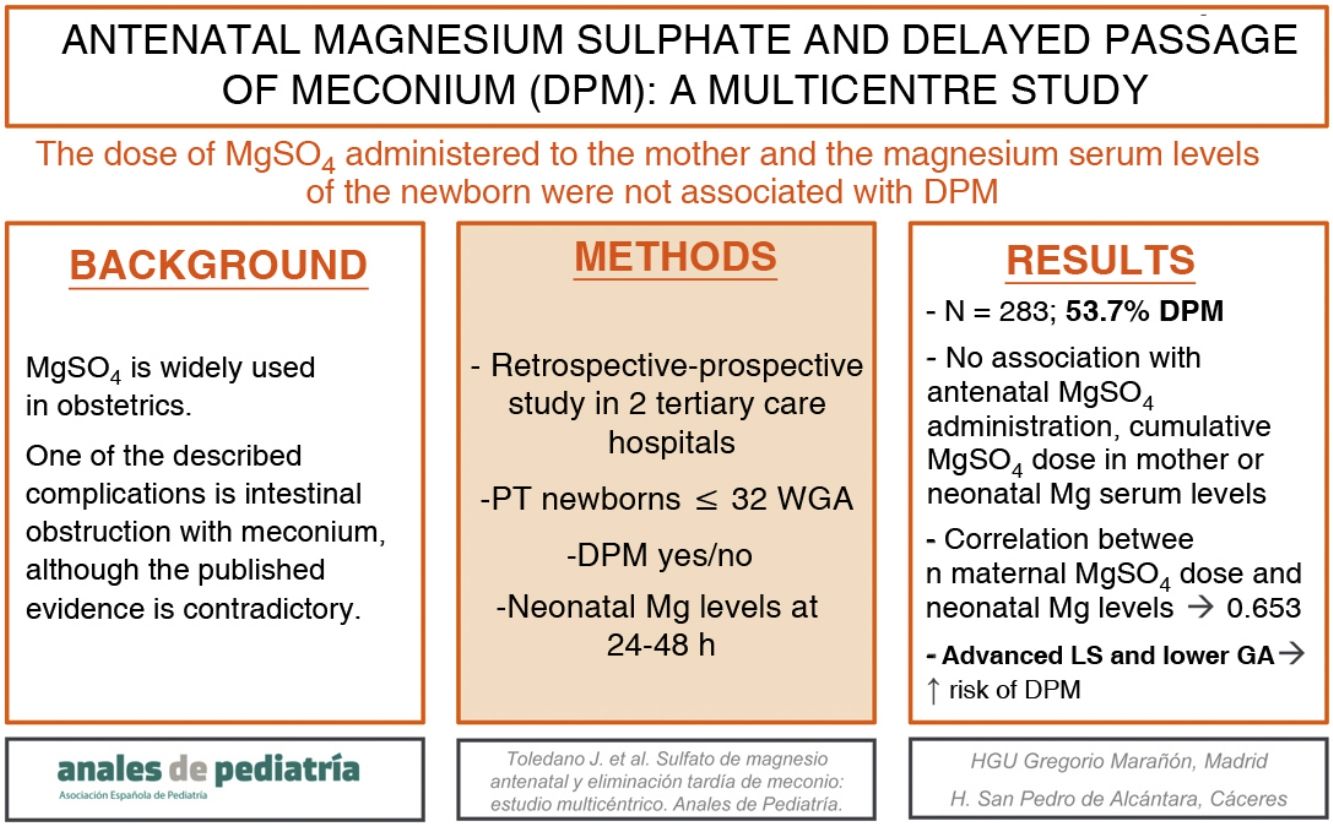
The published evidence on the association between magnesium sulphate (MgSO4) and delayed passage of meconium (DPM) is contradictory.
ObjectivesTo determine whether there is an association between the administration of MgSO4 to the mother and DPM in the neonate, and to analyse serum magnesium levels in neonates in relation to the cumulative dose of MgSO4 administered to the mother.
Population and methodsRetrospective and prospective descriptive and analytical study conducted in patients delivered at or before 32 weeks of gestation in 2 tertiary care hospitals. Delayed passage of meconium was defined as failure to pass meconium within 48 h of birth and/or need for rectal stimulation on 2 or more occasions to pass stool and/or interval of at least 48 h between the first and second bowel movements.
ResultsThe study included 283 patients (204 retrospectively and 79 prospectively), of who 152 (53.7%) experienced DPM. Delayed passage of meconium was not associated with antenatal MgSO4 administration, the cumulative maternal MgSO4 dose or neonatal serum magnesium levels.
Older gestational age (OR, 0.8; confidence interval [CI], 0.69–0.93; P = 0.003) was an independent protective factor against DPM, while the need for advanced resuscitation (OR, 2.24; CI 1.04–4.86; P = 0.04) was a risk factor for DPM.
ConclusionThe neonatal serum levels of magnesium reached with the doses of MgSO4 administered to mothers were not associated with DPM. Lower gestational age and the need for advanced resuscitation were predictors associated with an increased risk of DPM.
La relación entre sulfato de magnesio (MgSO4) y el retraso en la evacuación de meconio presenta resultados controvertidos en la literatura.
ObjetivosDeterminar si existe relación entre la administración de MgSO4 a la madre y la eliminación tardía de meconio (ETM) en el neonato y conocer los niveles de magnesio en sangre en estos, con respecto a la dosis acumulada de MgSO4 administrada a la madre.
Población y métodosEstudio descriptivo-analítico, en pacientes ≤ 32 semanas de edad gestacional, con diseño retrospectivo-prospectivo, llevado a cabo en dos hospitales de tercer nivel asistencial.
Se definió la ETM como retraso en la evacuación meconial ≥ 48 horas y/o necesidad de estimulación rectal en ≥ 2 ocasiones para realizar deposición y/o retraso ≥ 48 horas entre la primera y segunda deposición.
ResultadosSe reclutaron 283 pacientes (204 retrospectiva y 79 prospectivamente), de los cuales 152 (53,7%) presentó ETM.
No se encontró relación entre la administración de MgSO4 a la madre, ni la dosis acumulada de MgSO4 en esta, ni los niveles de magnesio en sangre del neonato con la presencia de ETM.
La mayor edad gestacional (OR 0,8, IC 0,69−0,93, p = 0,003) resultó factor protector independiente de la ETM y la necesidad de reanimación avanzada (OR 2,24, IC 1,04−4,86, p = 0,04) factor de riesgo.
ConclusionesLos niveles alcanzados de magnesio en sangre del neonato con las dosis de MgSO4 administradas a las madres, no se relacionan con la ETM. La menor edad gestacional y la necesidad de reanimación avanzada predicen mayor riesgo de ETM.
Magnesium sulphate (MgSO4) is a widely used medicine in obstetrics units. For decades, it has been employed as a tocolytic and for prophylaxis and treatment of convulsive seizures associated with preeclampsia.1 Several studies have evinced an association between antenatal administration of MgSO4 and a reduction in the incidence and severity of cerebral palsy and severe motor dysfunction at 2 years post birth, and, at present, one of its more frequent indications in obstetric care is the neuroprotection of infants born between 24 and 31+6 weeks of gestation.1–7 The mechanisms by which MgSO4 can prevent cerebral palsy have not been well established, but it is believed that it may involve its ability to minimise hypoxic/ischaemic brain injury by blocking n-methyl-d-aspartate (NMDA) receptors, hindering the passage of calcium to the intracellular space. It could also reverse the destructive action of oxygen radicals and excitatory amino acids.8–13
Several authors have described the potential deleterious effects in the neonate of antenatal exposure to MgSO4, including hypotonia, respiratory depression, an increased need of neonatal resuscitation and intubation,14,15 cardiac failure,16 lower 1-min and 5-min Apgar scores,12,14 intraventricular haemorrhage17 or a higher rate of admission to the neonatal intensive care unit.18 However, other studies have not found an association between antenatal exposure to MgSO4 and these adverse events.19–22
One of the most controversial potential complications of MgSO4 described in the literature is meconium obstruction, and the evidence to date has been contradictory. From the time Sokal et al.23 described delayed meconium passage causing intestinal obstruction in 2 neonates of less than 38 weeks of gestational age born to mothers treated with MgSO4 in 1972, attempts have been made to establish the association between these 2 events, but the results have been heterogeneous,24–26 and several studies published since have not found evidence of this association.20 Thus, the objectives of our study were to assess the association between the administration of MgSO4 to the mother and meconium passage in the neonate, and to measure serum magnesium levels in neonates in relation to the cumulative dose of MgSO4 received by mothers.
Sample and methodsWe conducted a descriptive and analytical study in preterm neonates born at or before 32 weeks of gestation. The study was structured in 2 phases: an initial single-centre retrospective phase, carried out from January 2016 to December 2017 (the results of which have already been published27); and a prospective phase, between October 2019 and September 2020, in which we included infants admitted to 2 tertiary care hospitals. The goal of the prospective phase was to increase the statistical power and external validity of the findings of the initial phase and to analyse the cumulative dose of MgSO4 administered to the mothers in relation to the serum levels of magnesium measured in the newborns.
We excluded patients transferred from other hospitals more than 48 h post birth, patients with known chromosomal diseases or major congenital anomalies and, in the prospective phase, patients for whom we were unable to obtain informed consent or serum magnesium levels were not measured (in the first 48 h post birth).
When it came to the sample size, we applied the calculation performed in the retrospective phase,27 in which we estimated that a sample of 201 patients would suffice to detect significant differences of 23% (28%–55%), with a power of 81% and an α of 0.05.
We defined delayed passage of meconium (DPM) as absence of meconium passage within 48 h of birth and/or need of rectal stimulation twice or more to assist passage and/or an interval of 48 h or greater between the first and second bowel movements, and grouped patients in the sample based on whether or not they had DPM.27
We reviewed electronic health records to collect data on maternal characteristics (age, hypothyroidism, diabetes), clinical characteristics of the pregnancy (singleton/multiple, preeclampsia, chorioamnionitis, antenatal administration of steroids and MgSO4) and the birth (vaginal/caesarean delivery, type of anaesthesia, Apgar scores and resuscitation level, defining advanced resuscitation as intubation or cardiac massage) and newborn characteristics and outcomes (weeks of gestation, birth weight, history of intrauterine growth restriction [IUGR, defined as an estimated foetal weight below the 10th percentile], meconium passage, sepsis [with microbiological confirmation by positive blood culture or clinical sepsis treated with a 5-day course of antibiotherapy], necrotising enterocolitis [Bell stage II or greater], days to full enteral feeding and death). In the prospective phase, we also collected the MgSO4 dose administered to the mother and neonatal serum levels of magnesium in the first 24 and 48 h post birth, measured in the laboratory of the corresponding hospital. Magnesium levels were measured in blood samples obtained for other purposes as ordered by the physician in charge, and did not involve collection of greater blood volumes, within 24 h of birth and, if an additional sample was obtained between 24 and 48 h post birth, the magnesium serum levels were measured again. Serum magnesium levels were not taken into account and did not guide the approach to the management of the patients, which was the same in both phases of the study. We compared all these variables in the group of patients with DMP and the group without DMP.
Maternal treatment with intravenous MgSO4 adhered to hospital protocol, which in turn was based on the recommendations of the Sociedad Española de Ginecología y Obstetricia (Spanish Society of Gynaecology and Obstetrics): loading dose of 4.5 g over 30 min followed by maintenance dose of 1–2 g/h until delivery or up to a maximum of 24 h.28
In the statistical analysis, we expressed qualitative variables as percentages and quantitative variables as mean and standard deviation (SD) or median and interquartile range, based on whether the data followed a normal distribution. We compared qualitative data by means of the χ2 test or the Fisher exact test, and quantitative data with the Mann-Whitney U test. We considered P values of less than 0.05 statistically significant. To identify factors potentially involved in DPM, we fitted a multivariate logistic regression model in which we introduced significant variables as covariates, and expressed the results as odds ratios (ORs) and 95% confidence intervals (CIs). We expressed the association between the cumulative dose of MgSO4 administered to the mother and the magnesium levels in the newborn using the Spearman rho.
The study was approved by the Ethics Committee of Research with Medicines of our hospital.
ResultsIn the period under study, a total of 324 newborns were delivered at or before 32 weeks’ gestation (216 in the retrospective phase and 108 in the prospective phase); of which the final sample included 283 (12 lost in the retrospective phase due to absence of data for the DPM outcome and 29 in the prospective phase due to lack of informed consent or lack of measurement of magnesium serum levels in the newborn in the first 48 h post birth), of who 152 (53.7%) had DPM. Table 1 summarises the result for pregnancy, perinatal and neonatal variables in both groups.
Results for pregnancy, perinatal and neonatal variables in each of the groups.
| DPM (n = 152) | No DPM (n = 131) | P | |
|---|---|---|---|
| Maternal agea | 33 (30−37) | 34 (30−37) | 0.929 |
| Hypothyroidismc | 15/149 (10.1%) | 20/129 (15.5%) | 0.173 |
| Maternal diabetesc | 11/148 (7.4%) | 13/128 (10.2%) | 0.423 |
| Multiple pregnancyc | 63/152 (41.4%) | 40/130 (30.8%) | 0.063 |
| Preeclampsiac | 27/150 (18%) | 23/130 (17.7%) | 0.947 |
| No steroids or incomplete coursec | 51/150 (34%) | 28/129 (21.7%) | 0.023 |
| Chorioamnionitisc | 21/150 (14%) | 22/128 (17.2%) | 0.464 |
| Caesarean deliveryc | 96/152 (63.2%) | 78/129 (60.5%) | 0.643 |
| General anaesthesiac | 16/140 (11.4%) | 17/123 (13.8%) | 0.243 |
| Gestational age (weeks)a | 28 + 0 (26 + 0–30 + 2) | 29 + 5 (28 + 0–31 + 0) | <0.001 |
| Weight (g)a | 985 (761−1296) | 1279 (1.000−1.520) | <0.001 |
| IUGRc | 24/152 (15.8%) | 14/131 (10.7%) | 0.209 |
| Deathc | 22/152 (14.5%) | 6/131 (4.6%) | 0.005 |
| 1-min Apgara | 6 (4−8) | 7 (5−8) | 0.005 |
| 5-min Apgara | 8 (7−9) | 8 (8−9) | 0.003 |
| ALSc | 52/151 (34.4%) | 21/131 (16%) | <0.001 |
| FiO2 in delivery room (%)a | 40 (30−56) | 30 (28−45) | 0.01 |
| Birth pHa | 7.28 (7.19−7.33) | 7.3 (7.22−7.35) | 0.047 |
| Birth calcium (mmol/L)b | 1.31 ± 0.12 | 1.31 ± 0.14 | 0.895 |
| Formula or mixed feedingc | 51/148 (34.5%) | 48/128 (37.5%) | 0.599 |
| Hours to initiation of enteral feedsa | 24 (10−48) | 12 (6−24) | 0.001 |
| Time to discontinuation of PN (days)a | 12 (8−20) | 8 (6−11) | <0.001 |
| NECc | 40/152 (26.3%) | 10/131 (7.6%) | <0.001 |
| Sepsis < 72 hc | 13/150 (8.7%) | 5/131 (3.8%) | 0.142 |
| Sepsis > 72 hc | 12/31 (38.7%) | 6/48 (12.5%) | 0.007 |
| Inotropes in first 72 hc | 34/150 (22.7%) | 12/131 (9.2%) | 0.002 |
| IMV in first 72 hc | 7/22 (31.8%) | 5/42 (11.9%) | 0.089 |
| Days of PICCa | 9 (7−13) | 7 (6−10) | 0.126 |
ALS, advanced life support, defined as intubation or cardiac massage; DPM, delayed passage of meconium; FiO2, fraction of inspired oxygen; IMV, invasive mechanical ventilation; IUGR, intrauterine growth restriction; NEC, necrotising enterocolitis; PICC, peripherally inserted central catheter; PN, parenteral nutrition.
Normally distributed quantitative data with homogeneous variance: expressed as mean ± standard deviation.
Qualitative variables expressed as counts and percentage over the total of the column. For cells where there were missing data and the cell total did not correspond to the total of the column, the absolute frequency is expressed as count/total values for the cell and the relative frequency as the percentage of the total values for the cell.
Patients were classified into the DPM group for a delay of 48 h or more in passing meconium (91/152; 59.87%), requiring an enema or rectal stimulation twice or more to pass meconium (87/152; 57.23%) and/or an interval of 48 or more hours between the first and second bowel movements (58/152; 38.16%). Seventy patients met 2 or more of these criteria.
We did not find an association between the presence of DPM and the antenatal administration of MgSO4, the cumulative dose of MgSO4 administered to the mother or serum levels of magnesium in the newborn (Table 2). The analysis included 76 measurements of magnesium serum levels taken in the first 24 h post birth and 23 other measurements taken before 48 h post birth. The Spearman correlation coefficient for the association between the cumulative MgSO4 dose given to the mother and neonatal magnesium serum levels was 0.653 (P < 0.001).
Results of variables related to antenatal MgSO4 in each group.
| DPM (n = 152) | No DPM (n = 131) | P | |
|---|---|---|---|
| Antenatal MgSO4c | 106/148 (71.6%) | 92/128 (71.9%) | 0.963 |
| Cumulative dose of MgSO4 (g)a | 9.5 (7.5−12.5) | 9.5 (7.125−14.5) | 0.761 |
| Neonatal Mg levels at 24 h (mg/dL)b | 2.777 ± 0.664 | 3.007 ± 0.734 | 0.170 |
| Neonatal Mg levels at 48 h (mg/dL)a | 2.665 (2.43−3.15) | 2.5 (2.3−2.7) | 0.266 |
DPM, delayed passage of meconium; Mg, magnesium; MgSO4, magnesium sulphate.
Normally distributed quantitative data with homogeneous variance: expressed as mean ± standard deviation.
Qualitative variables expressed as counts and percentage over the total of the column. For cells where there were missing data and the cell total did not correspond to the total of the column, the absolute frequency is expressed as count/total values for the cell and the relative frequency as the percentage of the total values for the cell.
The multivariate logistic regression model, in which DPM was the dependent variable and gestational age, antenatal steroid therapy, the need of advanced resuscitation and the 5-min Apgar were introduced as covariates, only 2 of the latter were significantly associated with DPM. We found that a greater gestational age (OR, 0.8; 95% CI, 0.69−0.93; P = 0.003) was an independent protector against DPM, while the need for advanced resuscitation (OR 2.24; 95% CI, 0.04–4.86; P = 0.04) was an independent predictor of DPM.
Lastly, we fitted one binary logistic regression model that did not evince a correlation between the cumulative dose of MgSO4 given to the mother and the need of advanced resuscitation in the newborn (OR, 0.91; 95% CI, 0.80–1.04) and a second model that also did not evince an association between neonatal magnesium serum levels within 24 h of birth and the need of advanced resuscitation (OR, 0.99; 95% CI, 0.46–2.12).
DiscussionOur study analysed the association between antenatal exposure to MgSO4 and the development of meconium obstruction in newborns delivered at or before 32 weeks of gestation, and found no association. We also found no association of DMP with either the cumulative dose of MgSO4 given to the mother or neonatal magnesium serum levels.
One of the potential complications of MgSO4 described in the literature that is most controversial is meconium obstruction, due to both the contradictory results published to date and to the lack of consensus on the definition of this outcome. Clatworthy et al.29 were the first to describe meconium plug syndrome as intestinal obstruction due to the inability of the colon to rid itself of the meconium residue. However, other terms have since been used to refer to this condition, such as syndrome of retained meconium, meconium disease or inspissated meconium syndrome, among others. Furthermore, the intestinal obstruction due to meconium comprehends a broad spectrum of diseases that include meconium ileus, transient functional ileus of the sick newborn infant, and meconium plug syndrome. At the same time, some authors differentiate between meconium obstruction of prematurity from the aforementioned conditions, defining it as the presence of obstructive symptoms several days after having passed some initial meconium in very low birth weight infants.30 In this case, we defined DPM as absence of meconium passage within 48 h of birth and/or need of rectal stimulation twice or more to assist passage and/or an interval of 48 h or greater between the first and second bowel movements, adhering to the definition used in the retrospective phase of the study, described in a previous publication.27
Studies conducted to date have reported contradictory results as regards the association between antenatal maternal treatment with MgSO4 and meconium obstruction in the newborn. Sokal et al.23 were the first to describe DPM causing intestinal obstruction in 2 neonates of less than 38 weeks of gestational age born to mothers treated with MgSO4. Since then, several authors have studied the association between the administration of MgSO4 and the presence of meconium obstruction, with inconclusive results.24,25 A prospective study conducted by Lloreda-García et al20 in newborns delivered before 32 weeks’ gestation also found no difference in the frequency of newborns that had not passed meconium at 48 and 72 h post birth between the control group and the antenatal MgSO4 group, which was similar to our results. However, a recent study conducted by Sung et al.26 in 226 newborns delivered before 25 weeks’ gestation did find a higher incidence of meconium ileus in the period in which MgSO4 was administered for neuroprotection compared to the period before this protocol was implemented and after the period after it had been discontinued due to the increase in intestinal complications.
In our study, we also evaluated other factors that could affect meconium passage, and found a statistically significant association with lower gestational age, lower birth weight, absence of a completed course of antenatal steroid therapy, lower Apgar scores, need of advanced resuscitation and greater FiO2 requirements.
Arnoldi et al.31 studied the factors associated with DPM in a sample of neonates with birth weights of less than 1500 g, and found that 81% had the first bowel movement after 48 h post birth. They also found that patent ductus arteriosus, mechanical ventilation and uteroplacental insufficiency were significantly associated with delayed passage. As occurred in our study, they found an increasing probability of DMP with decreasing birth weight and gestational age. However, we did not find differences based on the need of invasive mechanical ventilation in the first 72 h post birth.
Kim et al.32 analysed the incidence of meconium obstruction and associated risk factors in a retrospective case series and did not find differences based on the administration of MgSO4. However, in contrast to our study, in which we found that the lack of a completed course of antenatal steroid therapy was associated with DPM, these authors did not find a difference between the control group and the group with meconium obstruction independently of the administered doses of antenatal steroids.
We also assessed the association between the cumulative dose of MgSO4 received by the mother and neonatal magnesium levels, and found a positive correlation with a Spearman R of 0.65; that is, the greater the cumulative dose of MgSO4 in the mother, the greater the serum magnesium levels in the newborn the first 24 h post birth. García Alonso et al.13 also analysed this association in a prospective study that included 42 neonates born before 29 weeks’ gestation, with antenatal maternal treatment with MgSO4 in 28 cases with a mean dose of 10.09 g and a mean neonatal serum magnesium level of 2.68 mg/dL that was significantly higher compared to the control group. However, the authors found a weaker correlation compared to our study, with an R2 of 0.436. Kim et al32 also measured magnesium levels in the first 48 h of life in newborns whose mothers had received MgSO4 during gestation, and found serum magnesium levels of 3.7 mg/dL (SD, ± 0.7) in patients with DPM and 3.8 mg/dL (SD, ± 1.3) in controls.
Antenatal exposure to MgSO4 has also been associated with decreased cardiac function16 and high neonatal serum magnesium levels with poorer Apgar scores.12,14 Therefore, we sought to determine whether there is an association between the dose of MgSO4 administered to the mother or neonatal serum magnesium levels in the first 24 h post birth and the need of advanced resuscitation, and did not find one. These outcomes were consistent with the previous literature, as several studies have also not find this association.13,19,22
One of the strengths of our study is its multicentric design. In addition, contrary to other works in the current literature, data were collected prospectively and included neonatal magnesium serum levels in the first 24–48 h post birth.
However, there are also limitations that need to be taken into account. One of them is that some of the data were collected retrospectively, which entails a risk of bias. Furthermore, since there is no standardised or consistent definition of meconium obstruction of prematurity or delayed passage of meconium in infants born before 32 weeks’ gestation the current literature, it is difficult to design studies on the subject and compare them with the previous evidence. Also, we did not include other symptoms that could be associated with DPM in the analysis, such as feeding intolerance or severe abdominal distension. Lastly, magnesium serum levels were only measured in patients in whom collection of a blood sample was indicated for clinical reasons, which resulted in the loss of several eligible patients and a low number of serum magnesium values for the 48 h post birth timepoint.
ConclusionBased on our findings, it is reasonable to conclude that neonatal serum levels of magnesium, developed in the context of maternal treatment with MgSO4 at the dosage established in current hospital protocols, are not associated with DPM. On the other hand, lower gestational age and the need for advanced resuscitation were associated with an increased probability of this complication.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
Previous presentation: The manuscript was presented as an oral communication of the Sociedad Española de Neonatología at the XXVIII Congress of Neonatology and Perinatal Medicine -VIII Congress of Neonatal Nursing, held online in October 25–29, 2021.