Salmonella enteritidis is considered the leading cause of foodborne illness by toxicoinfection in children in developed countries. It usually causes mild and self-limiting disease. However, it may lead to complications and in rare cases to extraintestinal organ involvement. In adults, pancreatitis has been described as a potential complication of Salmonella infection.
We present a series of cases of acute pancreatitis in the context of infection by Salmonella enteritidis that occurred in the summer months of 2015. This is the first published case series on this complication in the paediatric population.
The series consists of four clinical cases of salmonellosis in children admitted to a tertiary care hospital due to moderate to severe dehydration. Table 1 summarises the clinical features of the cases. Salmonella enteritidis was isolated from stool cultures in all four cases. There was evidence of pathological elevation of pancreatic enzymes in all patients, but only three experienced an acute exacerbation of abdominal pain in the epigastric region that was poorly controlled with intravenous (IV) analgesia (paracetamol and metamizole) accompanied by oral feeding intolerance. These three patients received antibiotic therapy with third-generation cephalosporins or ampicillin, and pain management with IV meperidine and bowel rest. The patient that had elevated pancreatic enzyme levels but had not experienced a worsening of symptoms or changes in abdominal pain was treated with IV fluids and did not receive antibiotics, and oral feeding was reintroduced early on after IV rehydration. None of the patients developed bacteraemia or any other severe extraintestinal complications, except for prerenal acute kidney injury that resolved after improving hydration. All patients had good outcomes, with resolution of the gastrointestinal illness and a progressive decrease of pancreatic enzyme levels.
Clinical and epidemiological characteristics of cases of pancreatitis caused by Salmonella enteritidis.
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| Age | 13 years | 9 years | 9 years | 13 years |
| Time elapsed since onset of AGE | 3 days | 3 days | 12h | 2 days |
| History of consumption of contaminated food | Yes Chicken/mayonnaise/omelette | Yes Chicken/mayonnaise/omelette | Yes Chicken | Yes Omelette |
| Renal function | Prerenal acute kidney failure | Normal | Prerenal acute kidney failure | Prerenal acute kidney failure |
| Ions at admission | Na+ 129mmol/L K+ 2.9mmol/L | Na+ 129mmol/L K+ 2.7mmol/L | Na+ 127mmol/L K+ 3.6mmol/L | Na+ 129mmol/L K+ 2.9mmol/L |
| Other laboratory abnormalities | Metabolic acidosis Hypoalbuminaemia | – | Hyperglycaemia Hypoalbuminaemia | Mild hypoalbuminaemia |
| Changes in abdominal pain | Epigastric, non-radiating pain | No changes in abdominal pain (periumbilical) | Epigastric, non-radiating pain | Epigastric, non-radiating pain |
| Other symptoms | Anorexia, nauseas, vomiting, abdominal distension | – | Anorexia, vomiting | Anorexia, nausea, vomiting |
| Tachycardia, hypotension, fever, dyspnoea, shock | No | No | No | No |
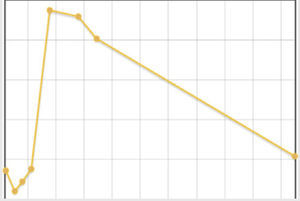
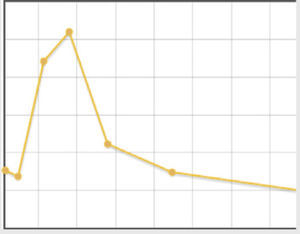
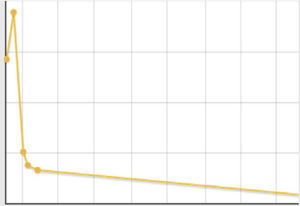
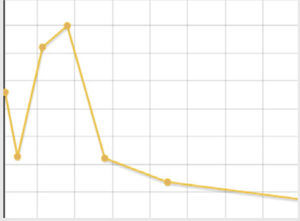
| Hyperamylasaemia and day of admission. Evolution of amylase levels | 323U/L on day 12. Peak: day 9, 446U/L | 123U/L on day 5. Peak: day 5, 123U/L | 169U/L on day 5. Peak: day 5, 169U/L | 137U/L on day 2. Peak: day 6, 521U/L |
| Hyperlipasaemia and day of admission. Evolution. | 617U/L on day 4. Peak: day 9, 570U/L | – | 207U/L on day 5. Peak: day 5, 207U/L | 228U/L on day 2. Peak: day 6, 699U/L |
| Abdominal ultrasound | Inflammation of pancreatic parenchyma Free intraperitoneal fluid | Not performed | Normal | Normal Diffuse bowel wall thickening. Free intraperitoneal fluid. |
| Salmonella enteritidis serotype | Salmonella enteritidis D9, sensitivea | Salmonella enteritidis D9, sensitivea | Salmonella enteritidis D9, ciprofloxacin resistant | Salmonella enteritidis C7, sensitivea |
| Antibiotic treatment | IV cefotaxime, 5 days | No antibiotic treatment | IV ampicillin, 7 days+oral amoxicillin, 3 days | IV cefotaxime, 5 days |
Based on the current literature, the diagnostic criteria for acute pancreatitis are clinical manifestations (mainly epigastric pain and vomiting) and laboratory abnormalities (amylase and lipase levels at least 3-fold the normal value, with a predictive positive value of 94%) compatible with the disease, as pancreatic abnormalities were not detected by ultrasound imaging in most of the described cases. Three of the patients in our series underwent an ultrasound examination, which detected inflammation of the pancreatic parenchyma in only one. The prognosis is good with appropriate antibiotic treatment and bowel rest.1
Although pancreatitis is a very rare complication of salmonellosis, some studies have analysed the potential causal relationship between the two diseases.2 Some authors have described an increased risk of developing pancreatitis in association with right-sided colitis, which could be considered a predictor.2
Table 2 summarises the most recent published studies (in the last 15 years) on this rare complication, although only one case was described in the paediatric age group.3 This disease may be underdiagnosed in everyday clinical practice, since its symptoms (abdominal pain and vomiting) may overlap with those characteristic of enteritis.3 The studies currently available propose ruling out this complication in cases with worsening epigastric pain that cannot be explained by enteritis and elevated pancreatic enzyme levels.
Review of the literature on pancreatitis due to infection by Salmonella enteritidis in the past 15 years.
| Publication | Study design. N | Objective | Results | Conclusion | ABT |
|---|---|---|---|---|---|
| Tossiti et al. (2001)5 | Prospective N=507 adults with acute gastroenteritis | Determine the incidence of hyperamylasaemia in AGE | • Incidence of hyperamylasaemia=10.2% • S. enteritidis: microorganism most frequently associated with hyperamylasaemia (22.2%) | • Significant enzyme level elevation • Pancreatitis not diagnosed | No |
| Moreno Cuerda et al. (2005)3 | Clinical case N=1 (adolescent aged 16 years with AGE due to S. enteritidis) | Case description | • Elevated pancreatic enzyme levels with symptoms and sonographic signs consistent with pancreatitis in a patient with AGE due to S. enteritidis | • Case of pancreatitis secondary to salmonellosis | Ceftriaxone |
| Pezzilli et al. (2003)6 | Prospective N=60 adults • 30 cases of salmonellosis (25: S. enteritidis, 5: S. typhimurium) • 30 healthy controls | Determine the prevalence of hyperamylasaemia/pancreatitis in adults with salmonellosis | • Prevalence of hyperamylasaemia (6.7%) Increase not significant (P=.2) • Prevalence of hyperlipasaemia (16.7%) Significant increase (P<.001) • No clinical or imaging correlation | • Significant increase in lipase levels during the course of salmonellosis, with no clinical impact. | No |
| Choung et al. (2014)2 | Descriptive N=1069 adults diagnosed with acute enteritis | Assess the prevalence and clinical significance of elevated pancreatic enzyme levels during acute enteritis | • Prevalence of elevated enzyme levels: 2.99% • Higher prevalence in cases with positive blood cultures • Microorganism most frequently associated with elevated enzyme levels during enteritis: Salmonella spp., specially S. typhimurium (amylase P=48; lipase P=.041) • Increased prevalence of elevated enzymes in cases with right-side colitis (amylase P=.002, lipase P=.029) | • The increase in levels of pancreatic enzymes in the course of enteritis was associated with right-sided colitis, symptom severity and positive blood cultures, and Salmonella was the microorganism isolated most frequently | No |
| Del Giorno et al. (2014)4 | Clinical trial (animal) | Demonstrate the impact of Salmonella infection on the pancreas in vivo and in vitro | • Colonisation of the pancreas by S. typhimurium both in vivo and in vitro | • The model demonstrated that Salmonella can cause pancreatic inflammation secondary to the enteric disease • Persistent pancreatic infection carries an increased risk of future ductal adenocarcinoma | – |
| Mofredj et al. (2014)1 | Case series (adults) 6 cases of pancreatitis due to Salmonella spp. | Description of cases: clinical manifestations, abnormal laboratory results, abnormal imaging, treatment, isolated serotype. | • 6 cases of pancreatitis secondary to enteritis due to Salmonella. Serotypes: S. enteritidis/typhimurium/typhi/paratyphi • Found abnormal laboratory results in association with clinical manifestations suggestive of pancreatitis • Normal ultrasound in 4/6 cases. Abnormal CT in 5/6 cases. • Good outcomes following antibiotic treatment | • Cases of pancreatitis secondary to enteritis due to Salmonella, diagnosed based on clinical manifestations, laboratory tests and imaging, with good outcomes following antibiotic treatment. | Ceftriaxone/ levofloxacin |
ABT, antibiotherapy; AGE, acute gastroenteritis; N, sample size.
Whether pancreatitis is part of the same gastrointestinal inflammatory process or should be considered an extraintestinal complication is currently under discussion. Different experimental animal models4 have demonstrated the association between gastroenteritis due to Salmonella and acute pancreatitis, and the potential dissemination of the bacterium to the liver and spleen. It is uncertain whether this is a true extraintestinal complication5 or rather a nonspecific inflammation of no clinical relevance6 in response to the underlying enteritis,4 which poses the dilemma of whether it should be treated or not. The indications for antibiotic therapy in cases of salmonellosis in children include bacteraemia, invasive extraintestinal forms of disease or the presence of risk factors (infants aged less than 3 months, asplenia, neoplasias, immunodeficiencies, haemoglobinopathies or inflammatory intestinal diseases). Under any other circumstances, antibiotherapy is not recommended because it would prolong bacterial shedding and convalescent carriage. In our series, antibiotics were only prescribed to patients that met the clinical and laboratory criteria for acute pancreatitis, fulfilling the definition of extraintestinal involvement established in current recommendations, consistent with those of the authors in the literature review. While we found no references in the literature describing an association of specific Salmonella enteritidis serotypes with pancreatitis, serotype D9 was isolated in 75% of the cases in this series.
Further research is needed to determine the true incidence of pancreatic involvement in children with salmonellosis and allow the individualised management of the disease. A potential pancreatic complication should be suspected in patients that develop vomiting associated with an acute epigastric pain that cannot be accounted for by the existing enteritis.
Please cite this article as: Pérez-Moreno J, Carrascón González-Pinto L, González Martínez F, Toledo del Castillo B, Rodríguez Fernández R. Pancreatitis aguda como complicación de gastroenteritis por Salmonella, una asociación poco habitual. An Pediatr (Barc). 2016;85:269–272.