Boy aged 8 years with a history of obesity and diagnosis of primary immune thrombocytopenia (PIT) 15 months prior. After the disease became steroid-dependent and following a transient response to immunoglobulin in the first year of follow-up, the patient had been received eltrombopag (75mg/day) for the past 3 months with little response. He had received immunoglobulin doses 10 days prior, achieving a count of 176 000 platelets/μL at 48h.
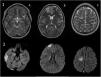
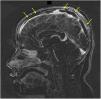
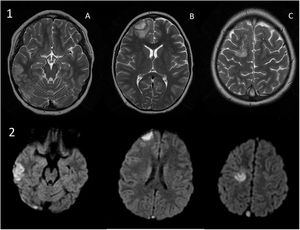
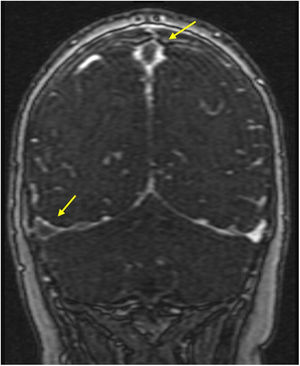
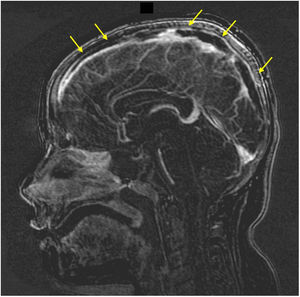
The patient presented with headache, vomiting, diplopia and paraesthesia in the left arm. The examination revealed high blood pressure, bradycardia, somnolence and weakness of the left upper extremity. The blood tests showed a platelet count of 177 000 platelets/μL and normal coagulation, and the cranial computed tomography (CT) scan detected acute foci of subdural and intraparenchymal bleeding. The evaluation was expanded with magnetic resonance [MR] imaging of the brain, which revealed areas of ischaemia secondary to venous sinus thrombosis (Figs. 1–3), prompting discontinuation of eltrombopag and initiation of heparin, which achieved a favourable response.
a) Axial view, T2-weighted image: signal hyperintensity compatible with cortical haematoma and oedema in the right temporal (A) and frontal (B) regions (B). Signal hyperintensity compatible with oedema in the right superior frontal gyrus (C). b) Axial views in diffusion-weighted imaging: restricted diffusion in the respective lesions.
The aetiological evaluation, which ruled out primary thrombophilia, yielded a positive result for antiphospholipid antibodies at high titres, which was confirmed 12 weeks later, leading to diagnosis of PIT secondary to antiphospholipid syndrome.
Although haemorrhage was historically the most feared complication of PIT, in recent years there has been growing awareness of the risk of thrombosis in these patients, especially those with a chronic course of disease.1 This risk is associated with both PIT itself, be it primary or secondary, as well as some of the used treatments (thrombopoietin analogues, steroids, etc).2 Thus, before initiating these treatments, it is recommended to assess the patient for the presence of other prothrombotic factors (obesity, hormonal methods of birth control, family history etc).3 In addition, in patients with chronic PIT or suggestive symptoms, it is essential to screen for potential autoimmune comorbidities, always including antiphospholipid syndrome.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.