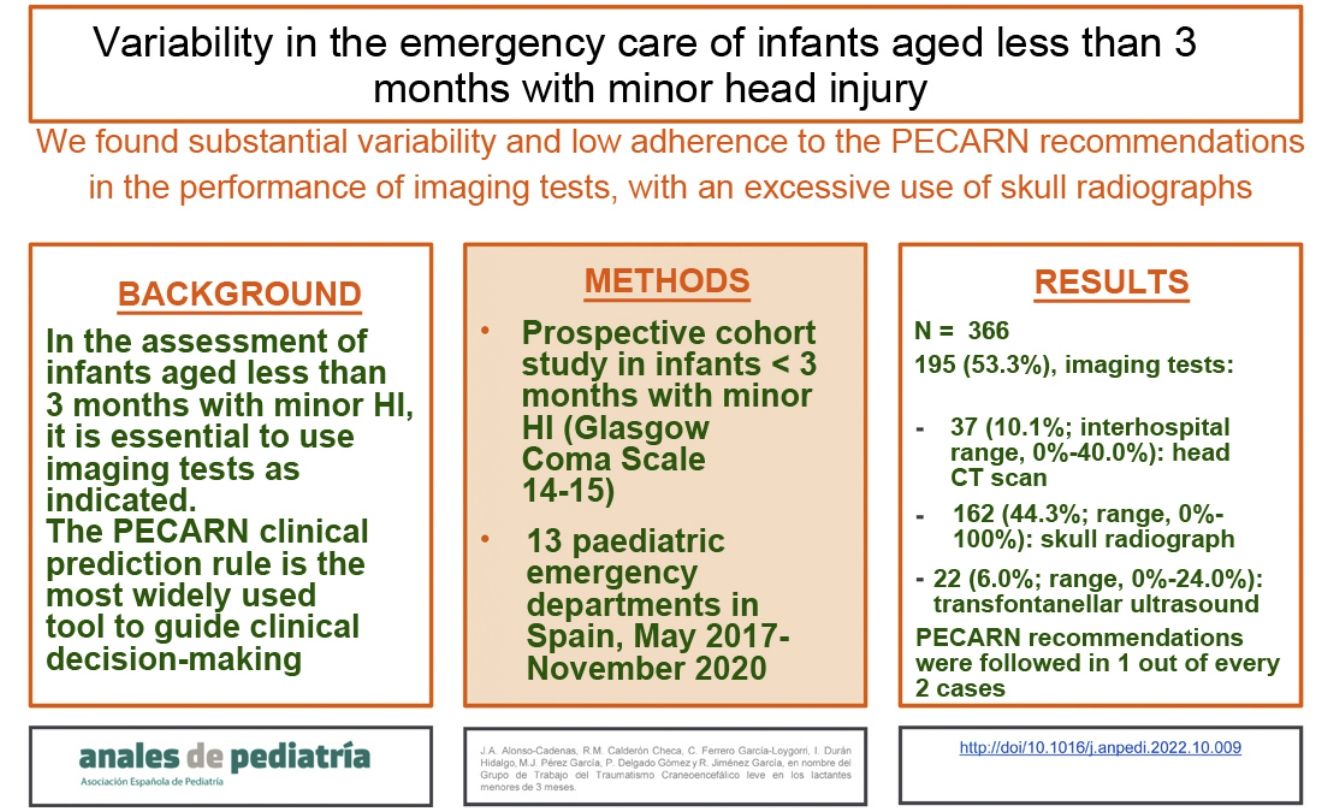
In the assessment of infants younger than 3 months with minor traumatic head injury (MHI), it is essential to adapt the indication of imaging tests. The Pediatric Head Injury/Trauma Algorithm (PECARN) clinical prediction rule is the most widely used to guide clinical decision making.
ObjectivesTo analyse the variability in the performance of imaging tests in infants under 3 months with MHI in paediatric emergency departments (PEDs) and the adherence of each hospital to the recommendations of the PECARN rule.
Population and methodsWe conducted a prospective multicentre observational study in 13 paediatric emergency departments in Spain between May 2017 and November 2020.
ResultsOf 21 981 children with MHI, 366 (1.7%) were aged less than 3 months; 195 (53.3%) underwent neuroimaging, with performance of CT scans in 37 (10.1%; interhospital range, 0%–40.0%), skull X-rays in 162 (44.3 %; range, 0%–100%) and transfontanellar ultrasound scans in 22 (6.0%; range, 0%–24.0%). The established recommendations were followed in 25.6% (10/39) of infants classified as high-risk based on PECARN criteria (range, 0%–100%); 37.1% (36/97) classified as intermediate-risk (range, 0%–100%) and 57.4% (132/230) classified as low-risk (range, 0%–100%).
ConclusionWe found substantial variability and low adherence to the PECARN recommendations in the performance of imaging tests in infants aged less than 3 months with MHI in Spanish PEDs, mainly due to an excessive use of skull X-rays.
En la valoración de los lactantes menores de 3 meses con un traumatismo craneoencefálico (TCE) leve es imprescindible adecuar la indicación de pruebas radiológicas. La regla de predicción clínica (RPC) PECARN es la más utilizada para ayudar en la toma de decisiones clínicas.
ObjetivosEvaluar la variabilidad en la realización de pruebas radiológicas en los menores de 3 meses con un TCE leve en los servicios de urgencias pediátricos (SUP) y la adherencia de cada hospital a las recomendaciones de la RPC PECARN.
Población y métodosEstudio de cohortes prospectivo en <3 meses con un TCE leve que consultaron en 13 SUP españoles entre mayo de 2017 y noviembre de 2020.
ResultadosSe atendieron 21.981 pacientes con un TCE leve, de los que 366 (1,7%) eran menores de 3 meses. Se realizaron pruebas de imagen al 53,3% (195): TC craneal a 37 [10,1% (rango entre hospitales 0%-40,0%)], radiografía de cráneo a 162 [44,3% (rango 0%-100%)] y ecografía transfontanelar a 22 [6,0% (rango 0%-24,0%)]. Se siguieron las recomendaciones PECARN en el 25,6% (10/39) de los lactantes con criterios de alto riesgo (rango 0%-100%); el 37,1% (36/97) de los de riesgo intermedio (rango 0%-100%) y el 57,4% (132/230) de los de bajo riesgo (rango 0%-100%).
ConclusionesExiste gran variabilidad, con un bajo cumplimiento de las recomendaciones PECARN, en la realización de pruebas radiológicas en los menores de 3 meses que consultan por un TCE leve en los SUP españoles, a expensas fundamentalmente de un exceso en el empleo de radiografías de cráneo.
Variability of care is defined as the systematic presence of variations in the use of a medical or surgical procedure or its outcomes, once the possibility that these differences can be attributed to the patients is ruled out1. Clinical variations unrelated to the course of disease are unwarranted.
The greatest challenge in the assessment of patients with minor head injury (HI) (defined as a Glasgow Coma Scale score of 14–15) is differentiating patients at risk of intracranial lesions (ICLs) from those at low risk and avoiding unnecessary diagnostic procedures. Computed tomography (CT) of the head is the gold for detection of an ICL, but the decision whether to use this imaging technique must weigh the importance of identifying an ICL that, while unlikely, could lead to important complications, against the risks involved in performing the test, the exposure to radiation and/or the need of sedation. It is well known that there is substantial variation in the use of CT of the head in children with minor HI in paediatric emergency departments (PEDs)2,3.
Clinical prediction rules (CPRs) have been developed with the aim of reducing variability in the ordering of head CT for assessment of paediatric minor HI, such as the Pediatric Emergency Care Applied Research Network (PECARN)4 rule, which is the most widely used. The PECARN rule differentiates between children aged 2 years or more and younger children2. The younger age group includes infants aged less than 3 months, a particularly vulnerable group to which the same recommendations used in all other age groups currently apply, despite a lack of studies on the particular characteristics of this paediatric subset5,6. The PECARN rule proposes a diagnostic algorithm for children under 2 years in which the indication of head CT depends on the findings of the physical examination of the patient.
The aim of our study was to assess variation in the performance of neuroimaging tests in infants aged less than 3 months with minor HI in PEDs and the adherence of each hospital to the recommendations of the PECARN rule.
Material and methodsWe conducted a prospective cohort study including infants aged less than 3 months assessed within 24h of suffering a minor HI (Glasgow coma scale score of 14–15) in 13 Spanish PEDs between May 2017 and November 2020. The exclusion criteria were: multiple trauma, underlying neurologic disease that interfered with the clinical evaluation, bleeding diathesis, non-accidental injury, refusal to participation and incomplete data. All infants were followed up through a telephone call in the 4 weeks that followed the encounter.
The study included secondary care and tertiary care hospitals (5 and 8, respectively). All of them had a specific protocol for the management of paediatric minor HI, including the possibility of performing an emergency CT of the head, and staffed qualified to deliver sedation as needed for the imaging procedure. The assessment in the PED was conducted by doctors specialised in paediatrics.
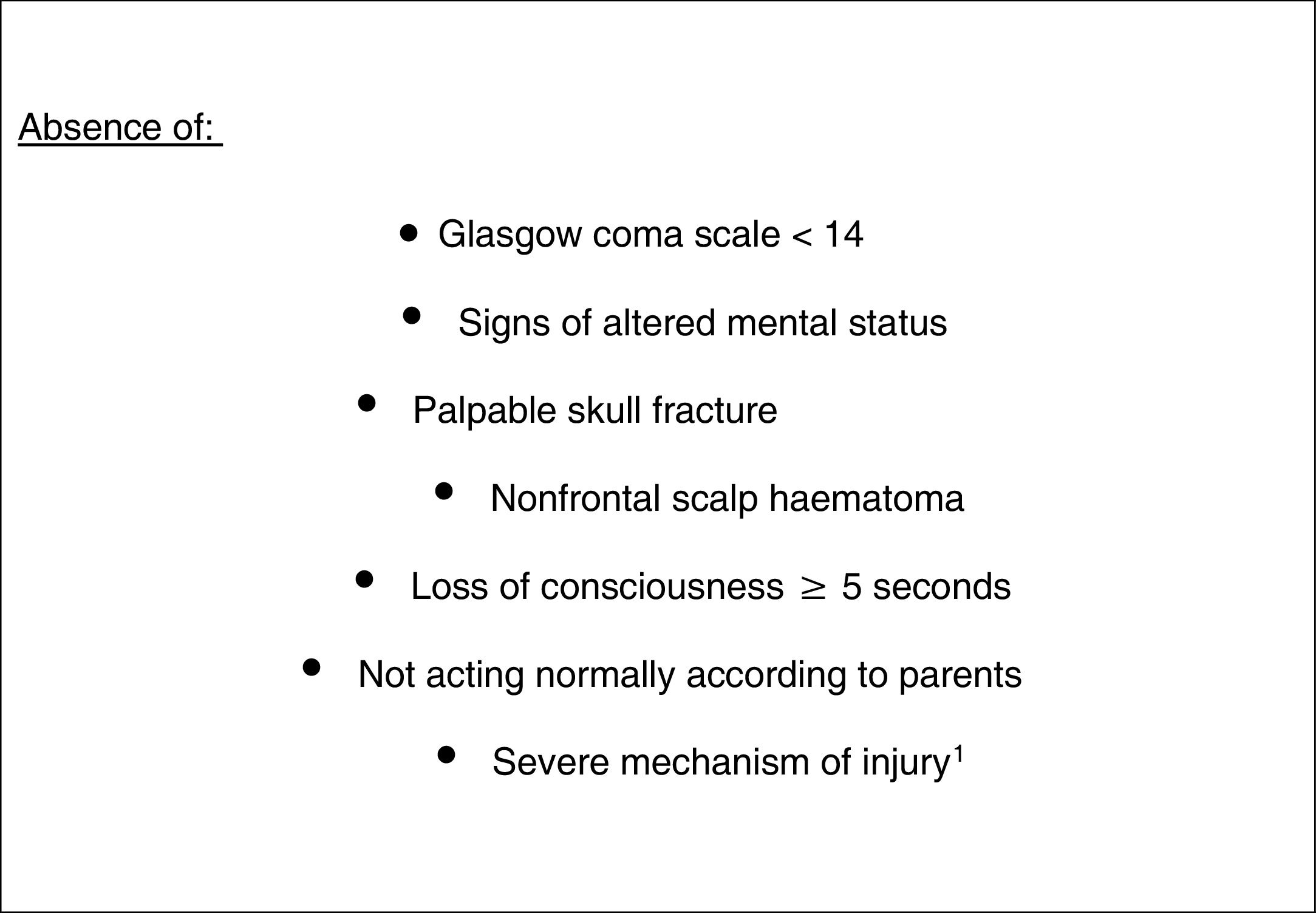
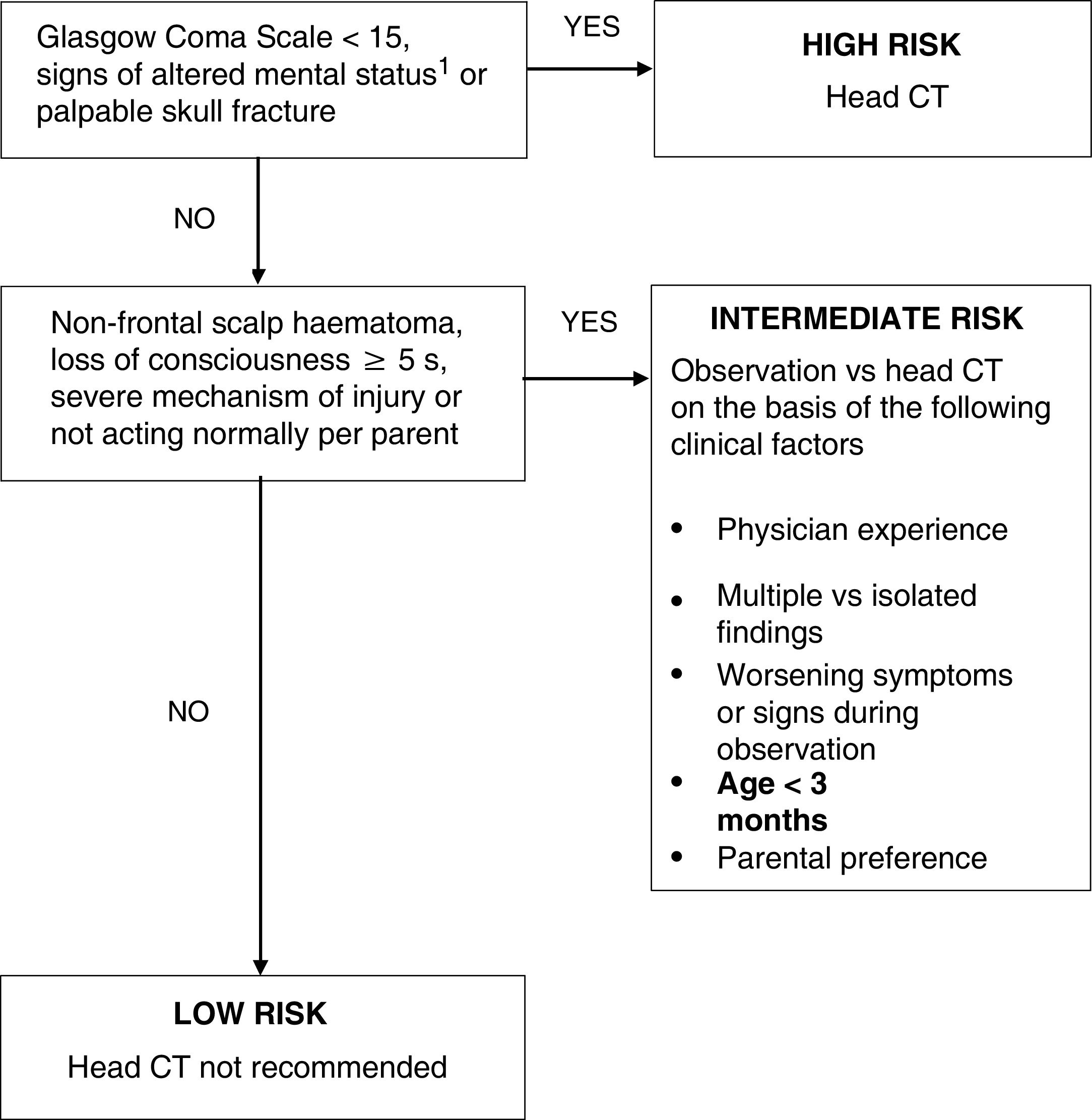
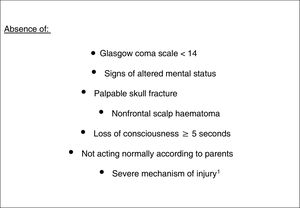
Imaging tests were ordered by the doctors in charge of the patients as they deemed necessary based on their clinical judgment and the care protocols of their hospitals. At a later time, we assessed whether their decisions adhered to the recommendations of the PECARN rule for children aged less than 2 years4. Fig. 1 presents the PECARN criteria and Fig. 2 the algorithm proposed in their cohort for the performance of imaging tests.
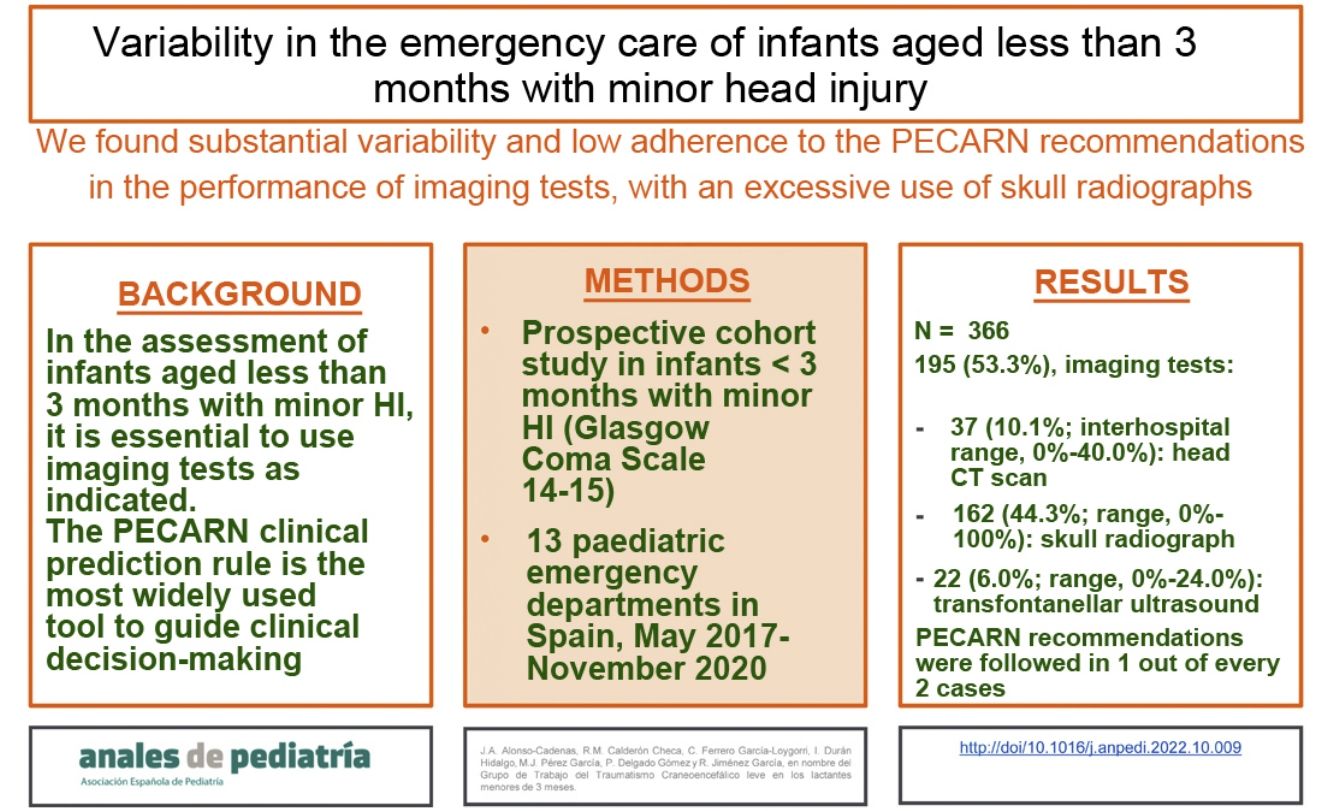
Criteria of the PECARN to define low risk in children aged less than 2 years (absence of the findings).
1Fall >0.9m, head struck by high-impact blunt object, motor vehicle collision with patient ejection, death of another passenger, or rollover; pedestrian struck by a motorized vehicle.
Diagnostic algorithm recommended by PECARN in patients aged less than 2 years with minor head injury.
1Agitation, somnolence, slow responses, asthenia. 2Fall >0.9m, head struck by high-impact blunt object, motor vehicle collision with patient ejection, death of another passenger, or rollover; pedestrian struck by a motorized vehicle. CT, computed tomography.
The results of imaging tests (head CT, skull radiograph, transfontanellar head ultrasound) were interpreted by paediatric radiologists.
The data were collected prospectively by researchers in each participating centre and entered into a single encoded database whose access was restricted to the principal investigator. We analysed clinical and sociodemographic variables: age, sex, mechanism of injury, symptoms in the history-taking and signs in the physical examination, performed imaging tests, radiological findings and outcomes of interest (clinically significant ICL, radiological ICL and isolated skull fracture).
The outcomes of interest were: (i) clinically significant ICL, defined as death resulting from traumatic brain injury or hospital admission with a stay of 2 nights or longer for minor HI with signs/symptoms associated with radiological ICL; (ii) radiological ICL, defined as presence of any acute abnormal intracranial finding or skull fracture traversing the full thickness of the skull associated with trauma; and (iii) isolated skull fracture, defined as a fracture detected in imaging of any kind (CT, skull X-ray or ultrasound) without significant depression.
We used the following care quality indicators for minor HI (Sociedad Española de Urgencias Pediátricas [SEUP])7:
- •
Frequency of performance of head CT for mild HI: number of head CT scans performed in patients with minor HI (care standard, <5%).
- •
Frequency of performance of skull X-ray for HI of any severity: number of skull X-rays performed in patients with minor HI (care standard, <5%).
The analysis was performed with the software STATA version17 (StataCorp). We summarised qualitative data as absolute and relative frequencies and quantitative data as mean, median and range.
The study was approved by the Ethics Committee of the coordinating hospital under file number R-0064/16, in addition to the ethics committees of each participating hospital. We obtained informed consent from each of the parents or legal guardians of the included patients.
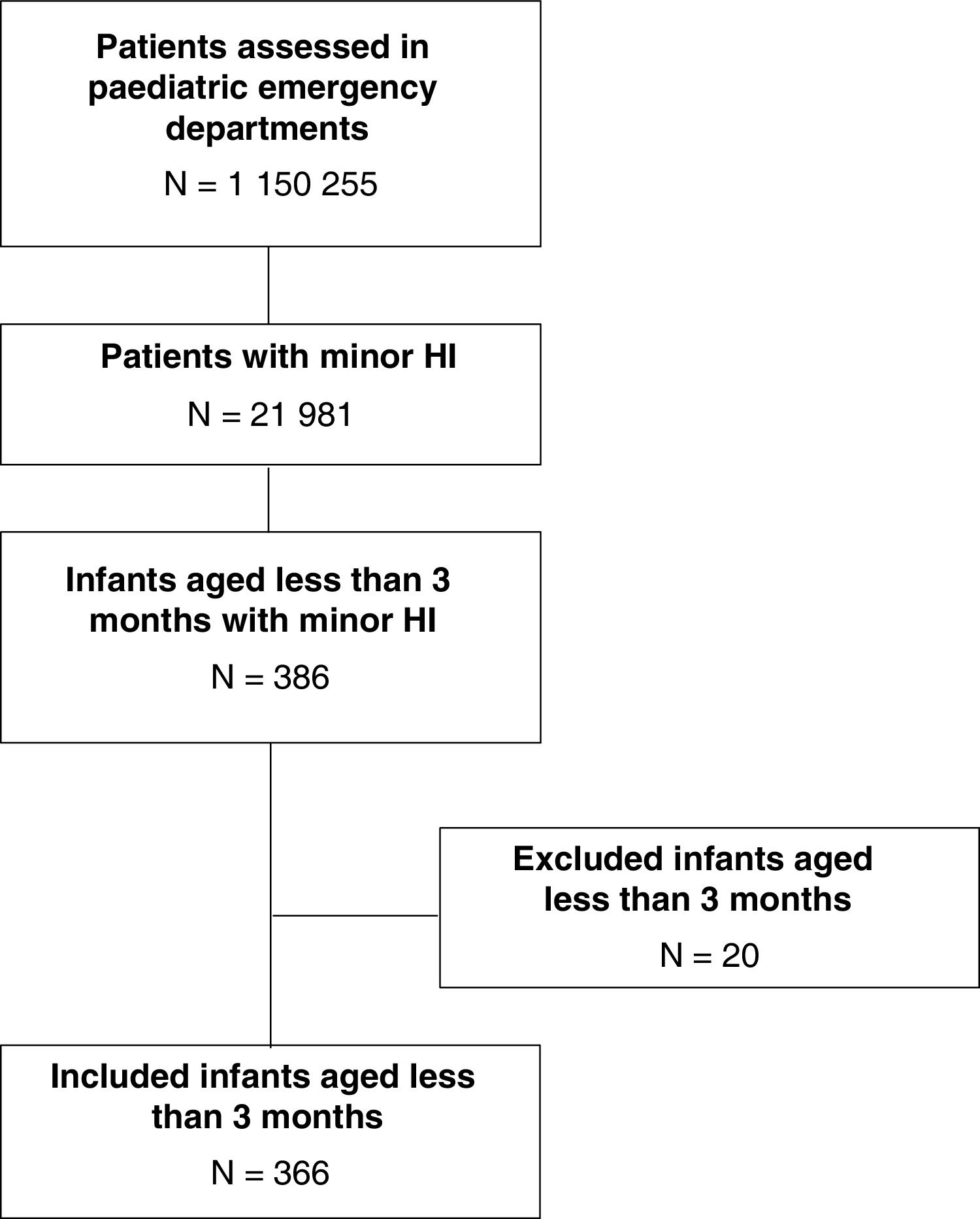
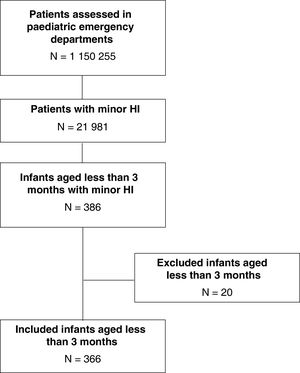
ResultsDuring the study period, 1 150 225 patients underwent assessment in the participating PEDs; 21 981 presented with minor HI, of who 386 were aged less than 3 months. We excluded 20 cases (11 due to incomplete data, 6 due to lack of informed consent and 3 due to non-accidental minor HI). The remaining 366 patients (1.7%) were included in the analysis (Fig. 3).
The median age was 49.3 days (interquartile range, 29.4–69.3) and 209 patients (56.5%) were male.
Most cases of minor HI (295/366; 80.6%) were associated with falls, most frequently from stationary surfaces (beds, changing stations, baby rockers) (135/295; 45.8%) or a pushchair (92/295; 31.2%). The second most frequent mechanism was impact with an object (71/366; 19.4%).
Most infants were asymptomatic (317; 86.6%) and free of abnormal signs in the physical examination (210; 57.4%).
Imaging tests were performed in 53.3% of patients (195): a head CT scan in 37 (10.1%), a skull X-ray in 162 (44.3%) and a transfontanellar ultrasound in 22 (6%). Twenty-three infants (6.3%) were assessed with more than one imaging test.
Only one patient had a clinically significant ICL (0.3% of the total; 95% CI, 0–1.5) and 12 had radiological ICLs (3.3% of the total; 95% CI, 1.7–5.7). All these patients (13) had an associated skull fracture. An isolated skull fracture was detected in 20 patients (5.5% of the total; 95% CI, 3.4–8.3).
Table 1 presents data on the imaging tests performed in the total sample and in each participating hospital.
Imaging tests performed in the total sample and in each participating hospital.
| Hospital | Number of patientsNa | Head CTn (%) | Skull X-rayn (%) | Transfontanellar USn (%) |
|---|---|---|---|---|
| Total | 366 | 37 (10.1%) | 162 (44.3%) | 22 (6%) |
| A | 92 | 5 (5.4%) | 78 (84.8%) | 0 |
| B | 78 | 2 (2.6%) | 27 (34.6%) | 2 (2.6%) |
| C | 59 | 13 (22%) | 11 (18.6%) | 3 (5.1%) |
| D | 50 | 3 (6%) | 30 (60%) | 12 (24%) |
| E | 26 | 3 (11.5%) | 1 (3.8%) | 3 (11.5%) |
| F | 16 | 3 (18.8%) | 2 (12.5%) | 0 |
| G | 12 | 2 (16.7%) | 4 (33.3%) | 1 (8.3%) |
| H | 8 | 1 (12.5%) | 0 | 0 |
| I | 6 | 0 | 6 (100%) | 0 |
| J | 5 | 2 (40%) | 0 | 0 |
| K | 5 | 0 | 3 (60%) | 0 |
| L | 5 | 0 | 0 | 1 (20%) |
| M | 4 | 0 | 0 | 0 |
CT, computed tomography; US, ultrasound.
N, total number of patients in the row; n, number of imaging tests performed in the row; %, percentage of the tests performed in each column relative to the number of patients in the row.
We found ample variation in the proportion of performance of head CT scans, from 2.6% in hospital B to 40% in hospital J. In a more detailed analysis that took into account whether the test was indicated based on the PECARN rule, only 3 of these scans were not indicated due to low risk (1 in hospital A, 1 in hospital C and 1 in hospital D).
Skull radiography was used extensively, except in 5 hospitals (hospitals E, H, J, L and M), 4 of which did not perform any (hospitals H, J, L and M). In the rest of hospitals, the proportion of cases assessed with skull radiography ranged from 12.5% (hospital F) to 100% (hospital I).
Of all the patients assessed with skull X-rays (162), 18 (11.1%) had a skull fracture. Fifteen of these patients (83.3%) also underwent a CT scan of the head, 4 had a radiological ICL and 1 had a clinically significant ICL that required urgent surgery. All had favourable outcomes.
Table 2 summarises the use of skull radiographs in asymptomatic infants with evidence of cephalohaematoma in the physical examination. Overall, a skull X-ray had been performed in 75% of these patients (42), and the percentage ranged from 50% (hospital G) to 100% (hospitals A, E, I and J).
Skull radiographs performed in asymptomatic infants with detection of scalp haematoma in the physical examination.
| Hospital | Asymptomatic infants with scalp haematoma in physical examinationN | Asymptomatic infants with scalp haematoma in physical examination assessed with a skull X-rayn (%) |
|---|---|---|
| Total | 56 | 42 (75%) |
| A | 11 | 11 (100%) |
| B | 12 | 8 (66.7%) |
| C | 11 | 6 (54.5%) |
| D | 10 | 9 (90%) |
| E | 3 | 3 (100%) |
| F | 2 | – |
| G | 2 | 1 (50%) |
| H | 1 | – |
| I | 3 | 3 (100%) |
| J | 1 | 1 (100%) |
| K | 0 | – |
| L | 0 | – |
| M | 0 | – |
N, total number of patients in the row; n, number of patients with a skull X-ray performed in the row; %, percentage of infants with a skull X-ray performed relative to the total infants in the row.
Transfontanellar ultrasound was the least used imaging test, although in some hospitals amounted to 20% (hospital L) or 24% (hospital D) of the total imaging tests.
Infants meeting PECARN criteria for high riskWe found adherence to the recommendations in the approach to 25.6% of the infants that met the high-risk criteria (10/39), which was performance of a head CT scan; the use of this test in these patients ranged from 0% (hospitals A, B and E) to 100% of cases (hospital H). A skull radiograph was taken in 35.9% (22/39) (range, 0% [hospital E] to 66.7% [hospitals A and D]). None of the high-risk patients were discharged directly after the examination (Table 3).
Recommended approach according to the PECARN rule and actual approach in each participating hospital in the set of infants that met the high-risk criteria.
| Hospital | Recommended approacha | Approach taken in infants in whom recommendations were not followedb | ||
|---|---|---|---|---|
| Head CTn/N (%) | Observationn/N (%) | Skull X-rayn/N (%) | Ultrasoundn/N (%) | |
| Total | 10/39 (25.6%) | 6/39 (15.4%) | 22/39 (35.9%) | 3/39 (5.1%) |
| A | 0/6 (0%) | 0/6 (0%) | 6/6 (66.7%) | 0/6 (0%) |
| B | 0/11 (0%) | 4/11 (36.4%) | 7/11 (63.6%) | 1/11 (9.1%) |
| C | 7/11 (63.6%) | 0/11 (0%) | 4/11 (36.4%) | 1/11 (9.1%) |
| D | 1/3 (33.3%) | 0/3 (0%) | 2/3 (66.7%) | 1/3 (33.3%) |
| E | 0/1 (0%) | 1/1 (100%) | 0/1 (0%) | 0/1 (0%) |
| F | 1/4 (25%) | 1/4 (25%) | 2/4 (50%) | 0 (0%) |
| G | 1/2 (50%) | – | 1/2 (50%) | – |
| H | 1/1 (100%) | – | – | – |
| I | – | – | – | – |
| J | – | – | – | – |
| K | – | – | – | – |
| L | – | – | – | – |
| M | – | – | – | – |
CT, computed tomography. N, total number of patients in the row; n, number imaging tests performed in the row; %, percentage of tests performed in each column relative to the number of patients in the row.
Performance of a head CT scan is recommended in case of a Glasgow Coma Scale score of 14, palpable signs of skull fracture or changes in behaviour; observation rather than a head CT scan is recommended in case of scalp haematoma (parietal, occipital or temporal), loss of consciousness ≥5s, not acting normally (per parent) or high-energy trauma.
The recommended approach in the PECARN rule (head CT scan vs observation) was carried out in 37.1% of cases (ranging from 4.5% [hospital A] to 100% [hospitals F, H, J and M]). A head CT scan was carried out in 6 out of 97 cases (6.2%) (1 in hospital A, 1 in hospital C, 2 in hospital E and 2 in hospital K) and observation in 30 out of 97 cases (30.9%). A skull X-ray was performed in 49.5% of cases (48/97) (Table 4).
Recommended approach according to the PECARN rule and actual approach in each participating hospital in the set of infants that met the intermediate-risk criteria.
| Hospital | Recommended approacha | Approach taken in infants in whom recommendations were not followedc | ||
|---|---|---|---|---|
| Head CT/observationbn/N (%) | Discharge homen/N (%) | Skull radiographn/N (%) | Ultrasoundn/N (%) | |
| Total | 36/97 (37.1%) | 4/97 (4.1%) | 48/97 (49.5%) | 14/97 (19.6%) |
| A | 1/22 (4.5%) | 0/22 (0%) | 21/22 (95.5%) | 0/22 (9.1%) |
| B | 4/12 (33.3%) | 3/12 (25%) | 5/12 (41.7%) | 1/12 (8.3%) |
| C | 11/17 (64.7%) | 1/17 (5.9%) | 5/17 (29.4%) | 0/17 (0%) |
| D | 3/22 (13.6%) | – | 14/22 (63.6%) | 9/22 (40.9%) |
| E | 5/8 (62.5%) | – | – | 3/8 (37.5%) |
| F | 2/2 (100%) | – | – | – |
| G | 2/3 (66.7%) | – | 1/3 (33.3%) | – |
| H | 2/2 (100%) | – | – | – |
| I | 0/1 (0%) | – | 1/1 (100%) | – |
| J | 3/3 (100%) | – | – | – |
| K | 1/2 (50%) | – | 1/2 (50%) | – |
| L | 1/2 (50%) | – | – | 1/2 (50%) |
| M | 1/1 (100%) | – | – | – |
CT, computed tomography. N, total number of patients in the row; n, number of imaging tests performed in the row; %, percentage of tests performed in each column relative to the number of patients in the row.
The PECARN rule recommendations for discharging the patient home were met in 57.4% of the infants (132/230), with adherence ranging from 0% (hospital I) to 100% (hospitals F, H, J, L and M). Three head TC scans were performed when not indicated (in 1.3% of low-risk infants), although one of them evinced a millimetric epidural haematoma that did not require neurosurgical intervention. In addition, 92 skull X-rays were ordered (in 40% of low-risk infants) (Table 5). The use of radiography varied widely between hospitals. Hospitals F, H, J, L and M did not perform any, while hospital I did one in every low-risk patient (5/5). Second in frequency was hospital A, which recruited the largest number of patients, with a proportion of 79.7% (51/64). Lastly, there were 5 transfontanellar ultrasound examinations (in 2.2% of low-risk infants). The hospitalization rate was 2.6% (6/230), and 3 of the admitted patients had an outcome of interest (1 radiological ICL and 2 isolated skull fractures).
Recommended approach according to the PECARN rule and actual approach in each participating hospital in the set of infants that met the low-risk criteria.
| Hospital | Recommended approacha | Approach taken in infants in whom recommendations were not followedb | |||
|---|---|---|---|---|---|
| Discharge homen/N (%) | Head CTn/N (%) | Skull X-rayn/N (%) | Ultrasoundn/N (%) | Admissionn/N (%) | |
| Total | 132/230 (57.4%) | 3/230 (1.3%) | 92/230 (40%) | 5/230 (2.2%) | 6/230 (2.6%) |
| A | 13/64 (20.3%) | 1/64 (1.6%) | 51/64 (79.7%) | 0/64 80%) | 2/64 (3.1%) |
| B | 40/55 (72.7%) | 0/55 (0%) | 15/55 (27.3%) | 0/55 (0%) | 0/55 (0%) |
| C | 26/31 (83.9%) | 1/31 (3.2%) | 2/31 (6.5%) | 2/31 (6.5%) | 1/31 (3.2%) |
| D | 8/25 (32%) | 1/25 (4%) | 14/25 (56%) | 2/25 (8%) | 1/25 (4%) |
| E | 16/17 (94.1%) | 0/17 (0%) | 1/17 (5.9%) | 0/17 (0%) | 0/17 (0%) |
| F | 10/10 (100%) | 0/10 (0%) | 0/10 (0%) | 0/10 (0%) | 0/10 (0%) |
| G | 5/7 (71.4%) | 0/7 (0%) | 2/7 (28.6%) | 1/7 (14.3%) | 1/7 (14.3%) |
| H | 5/5 (100%) | 0/5 (0%) | 0/5 (0%) | 0/5 (0%) | 0/5 (0%) |
| I | 0/5 (0%) | 0/5 (0%) | 5/5 (100%) | 0/5 (0%) | 1/5 (20%) |
| J | 2/2 (100%) | 0/2 (0%) | 0/2 (0%) | 0/2 (0%) | 0/2 (0%) |
| K | 1/3 (33.3%) | 0/3 (0%) | 2/3 (66.7%) | 0/3 (0%) | 0/3 (0%) |
| L | 3/3 (100%) | 0/3 (0%) | 0/3 (0%) | 0/3 (0%) | 0/3 (0%) |
| M | 3/3 (100%) | 0/3 (0%) | 0/3 (0%) | 0/3 (0%) | 0/3 (0%) |
CT, computed tomography. N, total number of patients in the row; n, number of imaging tests performed in the row (save for first column, which corresponds to patients managed correctly); %, percentage of tests performed in each column relative to the number of patients in the row.
The dataset evinced substantial variation in the clinical management and performance of imaging tests between hospitals. We considered that the approach adhered to the PECARN recommendations in nearly half the cases, with a greater adherence in the approach to infants at low risk of ICL
Ensuring the appropriate use of CT of the head in infants aged less than 3 months must be made a priority. In our series, we found that the use of this imaging test did not adhere to recommendations in either patients at low risk (performed when not indicated) or patients at high risk (not performed when indicated).
More than half of participating hospitals performed a head CT scan in more than 5% of the patients, which was not in compliance with the quality of care criterion established by the SEUP for cases of minor HI7, although this threshold was not established specifically for this age group.
Skull X-rays are useful to diagnose skull fractures, but not to identify ICLs. Yet, the frequency with which they were performed in our sample (nearly in half the infants) was excessive, despite current knowledge that this imaging test is not indicated in the case of minor HI on account of its low predictive value8 and low diagnostic yield in the identification of radiological lesions9–12. The only indication for skull radiography accepted by some authors is significant nonfrontal cephalohematoma in asymptomatic infants13–16, to be followed by a head CT scan in infants in which it identifies a fracture. In our sample, a skull radiograph was performed in 2 out of 3 of these infants. This indication has been revised in recent years, and it is now recommended to replace it by a head CT scan in the subset of patients with large cephalohaematomas17,18, and observation for several hours following the minor HI event in all other infants with this type of lesion. Most hospitals in our study performed skull X-rays in more than 5% of cases, exceeding the care quality threshold established by the SEUP7. The fact that infants younger than 3 months are a vulnerable group of patients who are also difficult to evaluate probably makes it more likely that doctors will order imaging tests, even if they are asymptomatic.
Only hospitals L and M fulfilled the 2 quality criteria, although they were the hospitals that contributed the fewest number of patients and they diverged greatly from hospitals that contributed more patients. Of the 5 hospitals that contributed the largest numbers of cases, the one that performed best was hospital E, with relative frequencies of 11.5% for head TC scans and 3.8% for skull X-rays.
Ultrasound is another imaging option in infants with minor HI. In our study, all ultrasound examinations were transfontanellar scans, but the detection of ICL may require a relatively large acoustic window that the fontanelle may not always provide, and this approach also has limitations when it comes to the assessment of the areas around the cerebral convexity, which may lead to underdetection of ICLs19. Point-of-care ultrasound is now an option, although its role in the assessment of these patients has yet to be determined20–22.
Overall, we found a low adherence to the recommendations of the PECARN rule (Fig. 2), which were only followed in 1 out of every 2 infants. In our opinion, this should be improved because their application could help limit the performance of head CT scans to infants at high risk of complications, including all infants at high risk and infants with intermediate risk and more than 1 risk factor or whose condition worsens while under observation in the emergency department. Radiography should be avoided altogether, as it cannot detect brain lesions.
In this study, all participating hospitals followed the low-radiation protocol in the performance of head CT scans and a head CT scan was done in all patients in whom it was indicated, even if they needed sedation, without restricting its indication. If this technique cannot be performed in a given centre, we recommend transferring the patient to a different hospital and ensuring the performance of the head CT scan.
Chief among the limitations of the study is the uneven number of patients recruited in each hospital, which makes it difficult to compare all participating centres adequately. Another limitation is that not all hospitals had the same characteristics. Some were tertiary level and others secondary level hospitals, although all PEDs were staffed with paediatricians. Furthermore, not every infant underwent a CT scan of the head and, as a result, our results may underestimate the risk of ICL or isolated skull fracture, although all infants were followed up by phone, which allowed a precise evaluation of clinically significant ICLs.
ConclusionThere is ample variation and a low adherence to the PECARN recommendations in the performance of imaging tests in infants younger than 3 months presenting with minor HI in Spanish PEDs, chiefly due to the excessive use of skull X-rays. Optimising the use of imaging tests in this age group must be prioritised, promoting the correct identification of infants at higher risk of ICL in whom a head CT scan is actually indicated and eliminating the use of skull radiographs.
FundingThe study was funded through an annual grant of the Sociedad Española de Urgencias de Pediatría (SEUP) for 4000 euro, awarded in 2017.
Conflicts of interestThe authors have no conflicts of interest to declare.
The epidemiological data of this study were previously published in another article: Alonso-Cadenas JA, Ferrero García-Loygorri C, Calderón Checa RM, Durán HidalgoPérez GarcíaRuiz González S, De Ceano-Vivas M, Delgado Gómez P, Antoñón Rodríguez M, Moreno Sánchez R, Martínez Hernando J, Muñoz López C, Ortiz ValentínJiménez-García R. Epidemiology of minor blunt head trauma in infants younger than 3 months. Eur J Pediatr. 2022, 181:2901−8.