Central venous catheter (CVC) insertion in neonates and small infants is a challenging and high risk procedure. Ultrasound (US) guided cannulation increases the success rate and reduces procedural-related complications. The internal jugular vein is the most frequent site for US-guided CVC insertion. However this approach is technically demanding in neonates and small infants. US-guided supraclavicular cannulation of the brachiocephalic vein (BCV) is a new approach that may be advantageous in case of difficult central venous catheterization. We present our preliminary experience with this technique in a case series of neonates and small infants.
MethodsCase series of neonates and small infants weighing less than 5kg, in whom US-guided supraclavicular cannulation of the BCV was attempted. A longitudinal “in plane” supraclavicular approach to the BCV was performed using a 12Hz linear or a 8Hz microconvex transducer. All cannulations were performed by the same operator, a paediatrician with previous experience in US-guided central venous catheterization.
ResultsThe study included 6 patients with a median (range) weight of 2.1 (0.94–4.1)kg and age of 1.9 (0.6–4) months. Two cases required 2 punctures, while cannulation was achieved at the first attempt in the remaining 4 cases. There were no procedural or catheter-related complications. CVCs were withdrawn after 9 (6–15) days.
ConclusionsThe US-guided supraclavicular approach to the BCV is a feasible and safe alternative in neonates and very small infants. More studies are needed to define the role of this new venous access before its routine application in daily practice.
La inserción de catéteres venosos centrales (CVC) en neonatos y lactantes pequeños es una técnica difícil y de riesgo. La canalización guiada por ecografía (ECO) aumenta la tasa de éxito y reduce las complicaciones. El acceso más habitual es el de yugular interna; sin embargo, en neonatos y lactante pequeños es técnicamente más difícil que a otras edades. Presentamos nuestra experiencia preliminar con una nueva técnica de canalización venosa central aplicable a neonatos y lactantes pequeños: el acceso supraclavicular del tronco braquiocefálico (TBC) guiado por ECO.
MétodosSerie de casos de neonatos y lactantes de peso inferior a 5kg en los que se ha intentado la canalización guiada por ECO del TBC mediante abordaje supraclavicular. Se utilizó un abordaje longitudinal en plano del TBC desde la fosa supraclavicular con un transductor lineal de 12Hz o microcónvex de 8Hz. Todas las canalizaciones fueron realizadas por el mismo operador, un pediatra con experiencia previa en la canalización guiada por ECO.
ResultadosSe incluyó a 6 pacientes con una mediana (rango) de peso de 2,1 (0,94-4,1) kg y edad de 1,9 (0,6-4) meses. En 2 casos se requirieron 2 intentos, canalizándose el TBC en un intento en los 4 restantes. No se observaron complicaciones relacionadas con el procedimiento ni con la permanencia del catéter, siendo los CVC retirados al cabo de 9 (6-15) días.
ConclusiónEl acceso supraclavicular al TBC guiado por ecografía es una alternativa factible y segura en neonatos y lactantes muy pequeños. Son necesarios más estudios antes su utilización rutinaria en la práctica clínica.
Cannulation of central veins is an essential procedure in critically ill children. However, among small neonates and infants, due to the smaller size of vessels and the proximity to other structures (especially in the access to the internal jugular vein and the subclavian), it is a complex technique with greater risk of immediate mechanical complications (multiple attempts, arterial puncture, pneumothorax).1 Traditionally, a series of external anatomical references has been used for location and for the venous puncture, depending on the chosen vein and approach (blind technique).2 Currently, the use of ultrasound (US) is recommended to locate the vascular structures and to guide the venous puncture, both in adults and in children, since it has been shown to increase the rate of success and reduce the number of puncture attempts and immediate mechanical complications.3–6
Less experience is available in US-guided central vein cannulation in small neonates. The internal jugular vein approach is usually used. However, this has a lower success rate than at other ages due to the technical difficulty presented by the small size of the vessel, the scant room for manoeuvring, and the tendency of the internal jugular vein to collapse with breathing and with minimum pressure of the transducer. Currently, based on existing evidence, routine use cannot be recommended, although the methodology of the studies from which this conclusion was derived has been criticised by some authors.7,8
In recent years, a new approach has been suggested, consisting of cannulation of the brachiocephalic veins (BCV) from the supraclavicular area, which could offer advantages in these patients. BCV is the largest-size vein which may be accessed for percutaneous cannulation, and it is simple to visualise with US in small children due to its superficial location. It has the advantage of allowing an in-plane longitudinal approach with improved control of the needle, having achieved good results in paediatric anaesthesia.9–12 However, experience in this approach is very scarce with critically ill small neonates and infants,13 and therefore we believe it is of interest to submit our preliminary experience with a series of very small neonates and infants.
Patients and methodsType of study: series of consecutive casesPatients: neonates and infants with weight below 5kg who had BCV cannulation in the period between April 2014 and January 2015. No patient was excluded.
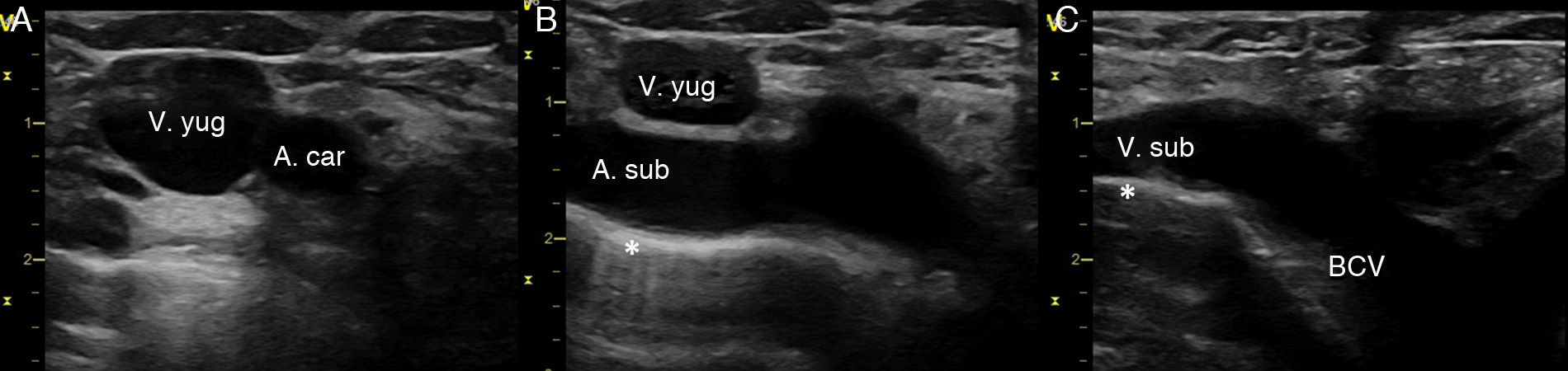
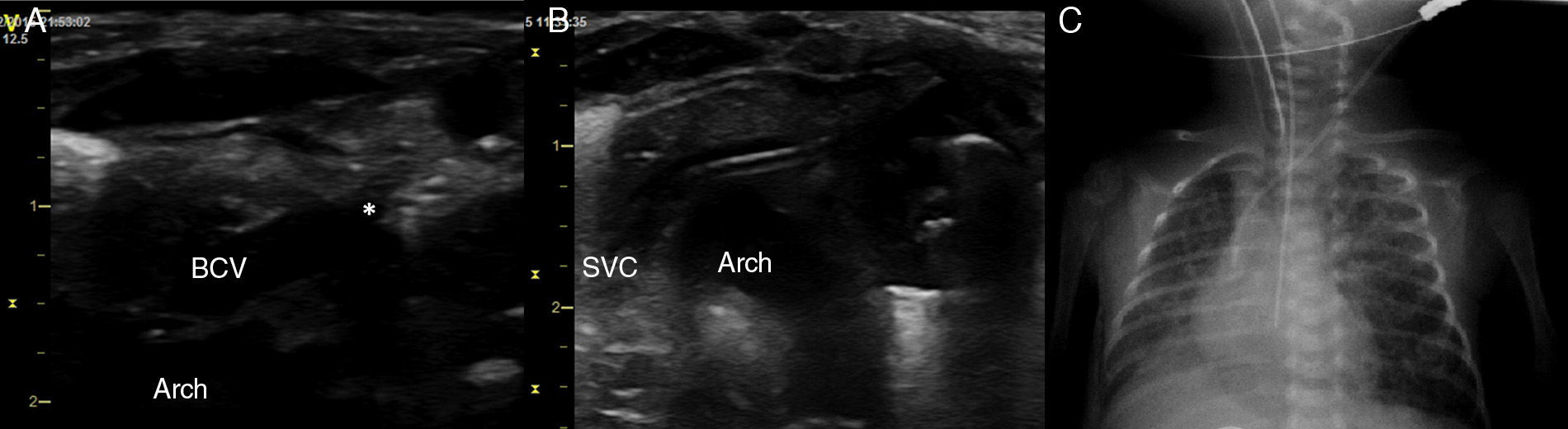
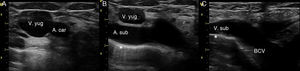
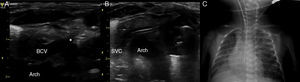
Procedure: the indications were made by the medical team in charge of each patient, considering their clinical condition and available vein access points. It was performed under analgosedation using the conventional Seldinguer technique under sterile conditions. The infant was placed in the Trendelenburg position at −30°, with a roll under the shoulders and the head rotated to 45° contra-laterally to the cannulation side. A portable ultrasound was used (Vivid i General Electrics, Haifa, Israel), equipped with a 12Hz linear probe and an 8Hz micro-convex. A 2D and colour-Doppler exploration of the jugular veins, subclavian, and BCV were conducted to define the anatomy, the size of the vessels and their permeability. To visualise the BCV, the cross-section of the internal jugular and carotid were obtained first, the transducer was slid downwards following the internal jugular vein until the supraclavicular fossa, and was tilted forwards (or anteriorly) to visualise the subclavian vein and the BCV on their long axes (Fig. 1). To define a safe trajectory for the needle, first the subclavian artery, and then the subclavian vein and the BCV, must be identified by means of the tilt manoeuvre (Fig. 1). In addition, the pleura must also be identified, and also the aortic arch when the left BCV is cannulated (Figs. 1 and 2). Then, the skin in punctured with a 22 gauge introducer needle directly in plane from the lateral side of the supraclavicular fossa. This is directed towards the vessel, avoiding the other structures (Fig. 2A). When blood can be aspirated, a flexible metal guidewire is introduced and the venous cannulation is completed as usual. In our cases, we used a straight 0.46mm diameter guidewire. The position of the guidewire, dilator and catheter may be confirmed by ultrasound during the procedure (Fig. 2B). The catheter size is chosen based on the size of the vessel, so that the external diameter of the catheter measures no more than one third of the BCV lumen. In our series, we used 3 French/6cm and 4 French/8cm bilumen central venous catheters (CVC). After cannulation, CVC placement was confirmed with X-rays (Fig. 2C).
Ultrasound exploration of the right BCV. (A) Transverse plane of the right internal jugular and carotid. (B) Sliding the transducer, following the internal jugular, the subclavian artery is identified. (C) Tilting the transducer anteriorly, the longitudinal axis of the subclavian vein is obtained, and its continuation to the BCV. Indicating the pleura.
Cannulation of left BCV. (A) Longitudinal plane of left BCV. (B) CVC placement control during the procedure. Note the close relation between the left BCV and the aortic arch. (C) Final position of the CVC in the upper part of the SVC. *Indicates the tip of the needle penetrating the vessel.
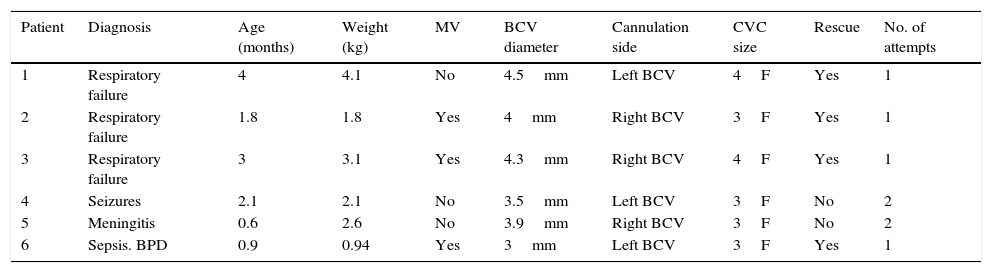
A total of 6 patients with a median weight (range) of 2.1 (0.94–4.1) kg and median age of 1.9 (0.6–4) months (Table 1) were included. In 4 of them, the technique was prescribed since it was impossible to cannulate any other central venous access (including the jugular vein by means of ultrasound-guided technique), whereas in the remaining 2 the procedure was elective after having explored the other veins with the ultrasound. In 3 patients, the right BCV was cannulated, and in the other 3, the left BCV. Cannulation was successful at the first attempt in 4 patients, whereas for the other 2 patients, 2 attempts were needed. The CVC were maintained for 9 (6–15) days, taking samples for culture at the time of removal. No complications related to cannulation or the permanence of the catheter were observed; patients did not present signs of infection related to the catheter and the cultures of the catheter tip were negative.
Characteristics of patients included.
| Patient | Diagnosis | Age (months) | Weight (kg) | MV | BCV diameter | Cannulation side | CVC size | Rescue | No. of attempts |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Respiratory failure | 4 | 4.1 | No | 4.5mm | Left BCV | 4F | Yes | 1 |
| 2 | Respiratory failure | 1.8 | 1.8 | Yes | 4mm | Right BCV | 3F | Yes | 1 |
| 3 | Respiratory failure | 3 | 3.1 | Yes | 4.3mm | Right BCV | 4F | Yes | 1 |
| 4 | Seizures | 2.1 | 2.1 | No | 3.5mm | Left BCV | 3F | No | 2 |
| 5 | Meningitis | 0.6 | 2.6 | No | 3.9mm | Right BCV | 3F | No | 2 |
| 6 | Sepsis. BPD | 0.9 | 0.94 | Yes | 3mm | Left BCV | 3F | Yes | 1 |
MV: mechanical ventilation; BPD: Bronchopulmonary dysplasia.
Central venous cannulation is an essential procedure to monitor and treat severely ill children, although it is not without its complications.2 In children, the femoral access is usually chosen as the less technically demanding and complication-free approach.14 Today, however, clinicians agree that no particular venous access is ideal for all paediatric patients, and that the approach must be chosen after assessing the technical indications, the characteristics of the patients, and the results of a US exploration of the patient's venous system. Guidelines recommend ultrasound-guided access whenever available.3
Small neonates and infants present the most complex and risky central venous cannulation, and only the safest, most effective techniques should be used.15 The femoral vein presents anatomical variations with regard to its position relative to the femoral artery, and is very small in the small newborn and infant (approximately 50% smaller than the internal jugular vein),16 which can carry a high risk of arterial puncture and difficulties in introducing the guidewire and catheter. As for the thoracic veins, the internal jugular may be hard to cannulate, since it collapses with breathing and with minimum pressure of the transducer. The use of US to locate vascular structures and to guide puncture has reduced the incidence of complications in femoral access.15,17 However, its usefulness in jugular access has not been conclusively demonstrated7,15,18 possibly due to limited space to manoeuvre with the probe, which in most cases calls for an out-of-plane approach with no direct control of the tip of the needle.1 Cannulation of the subclavian vein by anatomical references is associated with higher rates of pneumothorax and haemothorax, and so is not recommended as the access of choice in children.19 The use of US to cannulate the subclavian may improve the results by allowing direct visualisation of the vascular structures, the needle and the pleura during the procedure. However, US is ineffective during the traditional subclavicular approach, since the clavicle is a barrier to the ultrasound and it may prevent needle control during the procedure. Moreover, passing the guidewire and the catheter under the clavicle may cause them to kink, which may occasionally prevent cannulation in spite of having correctly punctured the vessel.
The supraclavicular approach to the BCV has been described recently, and might offer advantages with regard to classic access points, particularly in small neonates and infants. The BCV is the largest vein in children under 6 years and it may be approached supraclavicularly with the aid of US. This allows the operator to visualise the vein on the long axis without obstacles to the ultrasound, and introduce the needle “in-plane”, with direct visualisation of the trajectory at all times (Fig. 1). Unlike the internal jugular, the size of the BVC does not vary with breathing or with external compression or movement of adjacent tissues, which facilitates the introduction of the needle. Furthermore, unlike the internal jugular, cannulation of the BVC may be performed from the patient's side without “competing” with airway management devices, which is very important in critical infants and neonates, where space for manoeuvring in the sterile field is scarce. Furthermore, it has been proven useful in patients with haemorrhagic diathesis, since the supraclavicular puncture area may be compressed, which facilitates haemostasis.20
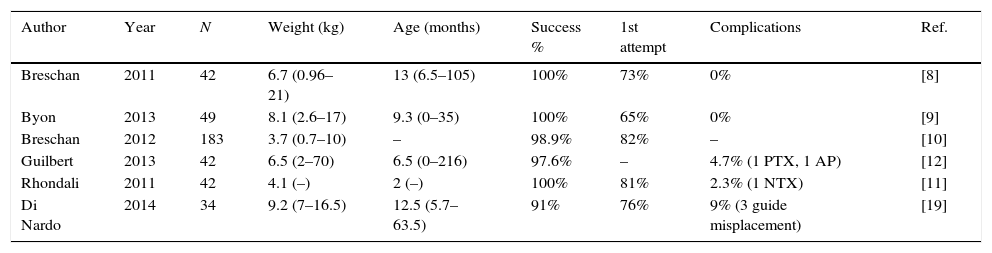
So far, several studies in paediatric patients have been published where this approach was applied, with excellent results (Table 2). Our series, although limited in number, includes smaller patients than most other publications (mean age 1.9 months and mean weight 2.1kg), with our results matching those previously published with regard to success rate in cannulation (66% in the first attempt and 100% in the second attempt) and complications (0%) (Table 2). The newborn with lowest weight in the series is worth mentioning, a pre-term with gestational age of 25 weeks, weighing 940g, and 28 days of life at the time of cannulation, who was subject to invasive mechanical ventilation and presented hospital-acquired infection due to Staphylococcus aureus. He did not have any vascular access after multiple failed attempts of central and peripheral cannulation (including femoral and jugular access through dissection, performed by the vascular surgeon). In this patient, access to the left BCV (measuring 3mm) was achieved at the first attempt, which allowed his sepsis to be treated.
Previous studies of cannulation of brachiocephalic vein in children using the supraclavicular approach.
| Author | Year | N | Weight (kg) | Age (months) | Success % | 1st attempt | Complications | Ref. |
|---|---|---|---|---|---|---|---|---|
| Breschan | 2011 | 42 | 6.7 (0.96–21) | 13 (6.5–105) | 100% | 73% | 0% | [8] |
| Byon | 2013 | 49 | 8.1 (2.6–17) | 9.3 (0–35) | 100% | 65% | 0% | [9] |
| Breschan | 2012 | 183 | 3.7 (0.7–10) | – | 98.9% | 82% | – | [10] |
| Guilbert | 2013 | 42 | 6.5 (2–70) | 6.5 (0–216) | 97.6% | – | 4.7% (1 PTX, 1 AP) | [12] |
| Rhondali | 2011 | 42 | 4.1 (–) | 2 (–) | 100% | 81% | 2.3% (1 NTX) | [11] |
| Di Nardo | 2014 | 34 | 9.2 (7–16.5) | 12.5 (5.7–63.5) | 91% | 76% | 9% (3 guide misplacement) | [19] |
Results are shown as median and range.
PTX: pneumothorax; AP: arterial puncture.
Like any new technique, it is important to understand the critical points of this method and to take into consideration the learning curve. One of the critical points of the technique described is to maintain at all times visual control of the needle as it progresses towards the vessel, which requires a certain degree of dexterity and hand co-ordination, since the ultrasound plane has a thickness of barely 1mm and any movement, however small, may imply losing sight of the needle with the potential risk of immediate complications (arterial puncture, pneumothorax, injury to the thoracic duct and injury to the brachial plexus). Therefore, prior experience and training with US are essential before attempting this access.21,22 With regard to the choice of the side to cannulate, the left BCV offers some advantages over the right, since it has a more direct trajectory towards the superior vena cava, which is correlated to higher success rates in the first attempt and lower incidence of misplacement of guidewire or CVC.11
Our results are limited by the number of cases included and by the fact that all cannulations were conducted by one of the authors with experience in the use of US in neonates and infants. It would seem reasonable that professionals should acquire sufficient experience and skill in the use of US and central venous cannulation before attempting this new vascular access. At any rate, although results seem promising, BCV cannot be considered the new access of choice, since there are no comparative studies with other ultrasound-guided cannulation techniques. Until having this data, we believe the BCV access must be considered a rescue technique when all others fail, and also as an alternative technique if difficult vascular access is anticipated after ultrasound assessment of the venous anatomy and the particular characteristics of the patient.
ConclusionSupraclavicular access guided by ultrasound of the BCV may be a feasible and safe alternative in small neonates and infants with difficult vascular access, when the professional conducting it has experience in central venous cannulation guided by US.
Conflict of interestsThe authors state there is no conflict of interest.
Please cite this article as: Oulego-Erroz I, Alonso-Quintela P, Domínguez P, Rodríguez-Blanco S, Muñíz-Fontán M, Muñoz-Lozón A, et al. Canalización del tronco braquiocefálico guiada por ecografía en neonatos y lactantes. An Pediatr (Barc). 2016;84:331–336.