Teledermatology is a technique that is increasingly being developed. There are many studies that assess this discipline in the general population, but few studies analyse the paediatric population exclusively. The aims of this study are to describe the distribution of diseases consulted through teledermatology, the use of this technique to avoid face-to-face consultations, and the agreement between virtual and face-to-face diagnoses, in the paediatric population.
Material and methodsThe work consisted of an observational and retrospective study of the virtual consultations made between May 2011 and January 2015 through a store-and-forward teledermatology programme, involving patients from 0 to 15 years. We collected demographic data, as well as the diagnoses made by the paediatrician who made the virtual consultation, and by the dermatologists who assessed the virtual and the face-to-face consultations, the indication given by the dermatologist who assessed the virtual consultation (discharge or referral), reason for referral, and diagnostic agreement rate.
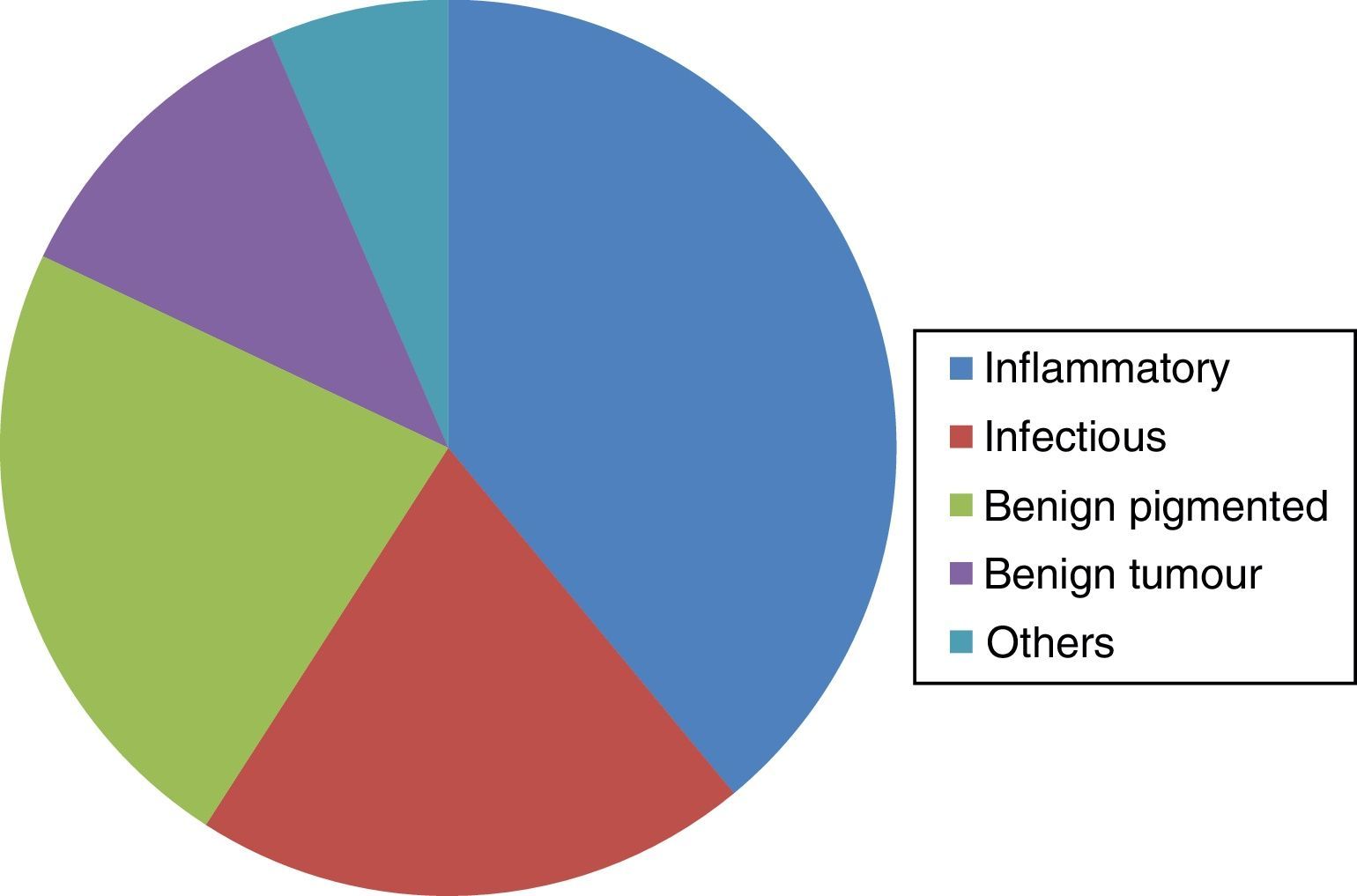
ResultsA total of 183 virtual consultations were analysed. The most frequent diagnoses were inflammatory diseases (39%), benign pigmented lesions (23%), and infectious diseases (20%). Almost half of the virtual consultations (48%) were referred to a face-to-face diagnosis. Diagnostic agreement between the dermatologist who evaluated the virtual consultation and the dermatologist who evaluated the face-to-face consultation was 89%, and 66% between the paediatrician who made the virtual consultation and the dermatologist who assessed it.
ConclusionsVirtual consultations have a similar disease distribution to conventional (face-to-face) referrals. Approximately half of the virtual consultations do not require a subsequent face-to-face visit. The agreement rate between the diagnoses given by both dermatologists (virtual and face-to-face diagnoses) is high.
La teledermatología es una técnica en expansión. Múltiples trabajos evalúan esta disciplina en la población general, siendo pocos los estudios que analizan la población pediátrica. Nuestro objetivo consistió en describir el tipo de patología consultada a través de esta técnica, su capacidad resolutiva y el grado de concordancia entre los diagnósticos virtuales y presenciales, en población pediátrica.
Material y métodosEl trabajo consistió en un estudio observacional retrospectivo de las consultas virtuales realizadas entre mayo de 2011 y enero de 2015 a pacientes de 0 a 15 años, mediante un sistema de teledermatología diferida. Se recogieron datos demográficos, diagnósticos indicados por el pediatra realizador de la teleconsulta y por los dermatólogos que evaluaron las consultas virtuales y presenciales, actitud a seguir indicada por el dermatólogo en la consulta virtual (alta/remisión a consulta), motivo de remisión y grado de acuerdo entre los diagnósticos emitidos.
ResultadosSe analizaron 183 teleconsultas. Los diagnósticos más frecuentes fueron patología inflamatoria (39%), lesiones pigmentadas benignas (23%) y patología infecciosa (20%). El 48% de las teleconsultas requirieron una visita presencial posterior. La concordancia diagnóstica entre el dermatólogo evaluador de la teleconsulta y el dermatólogo realizador de la consulta presencial fue del 89%, y entre el pediatra y el dermatólogo evaluador de la teleconsulta, del 66%.
ConclusionesLas patologías consultadas a través de teledermatología presentan una distribución similar a las consultas presenciales. Aproximadamente, la mitad de las teleconsultas no requiere evaluación presencial posterior. El grado de acuerdo entre el dermatólogo evaluador de la teleconsulta y el que realiza la consulta presencial es elevado.
Telemedicine is an expanding discipline. Because of the importance of images, dermatology is one of the specialities in which it has been most extensively implemented. In general terms there are 2 systems for conducting teledermatology: one by store-and-forward and the other in real time, in which doctors and patients communicate at the same time. Most studies show greater agreement between virtual and face-to-face diagnoses with real-time systems. However, store-and-forward systems are more feasible in day-to-day clinical practice, and are therefore the most widely used.1,2
There are many studies that evaluate various aspects of this technique, such as patient satisfaction, diagnostic agreement with in-person visits and ability to resolve the condition. In general, most of these studies assess all the consultations conducted, which primarily involve adult patients.3,4 There are few observations that focus solely on the paediatric population.
Our objective was to carry out a descriptive analysis of the types of disease that give rise to consultation by teledermatology, the ability of this form of consultation to resolve the condition and the rate of agreement between the diagnoses made by the various doctors assessing the same patient, focusing throughout on the paediatric population.
Material and methodsThe research consisted of a retrospective observational study of the teleconsultations made to patients in the paediatric age group through a store-and-forward teledermatology system in the Complejo Hospitalario de Pontevedra (EOXI Pontevedra-Salnés). Teledermatology was gradually introduced in Galicia from 2001 and began to operate in our hospital in May 2011. Therefore, the period of our study was from May 2011 to January 2015. The teleconsultations were from paediatric primary care, which in the Autonomous Committee of Galicia comprises children aged from 0 to 15 years inclusive. Through the SIGAP (Integrated Primary Care Management System) programme, paediatricians completed a questionnaire containing the basic items in the medical record (clinical history, personal and family history, physical examination, suspected diagnosis and treatments previously administered) and attached one or more clinical images. For each teleconsultation the same programme provided a space for the dermatologist's response, in which he or she indicated the diagnosis and the treatment plan to be followed. The teledermatology programme (SIGAP) is linked to the electronic medical records (IANUS programme), which facilitates follow-up of subsequent face-to-face consultations. The teleconsultations, from 15 health centres, were randomly assigned to 6 different dermatologists. The face-to-face consultations were scheduled with 8 dermatologists according to the availability of places on the waiting lists.
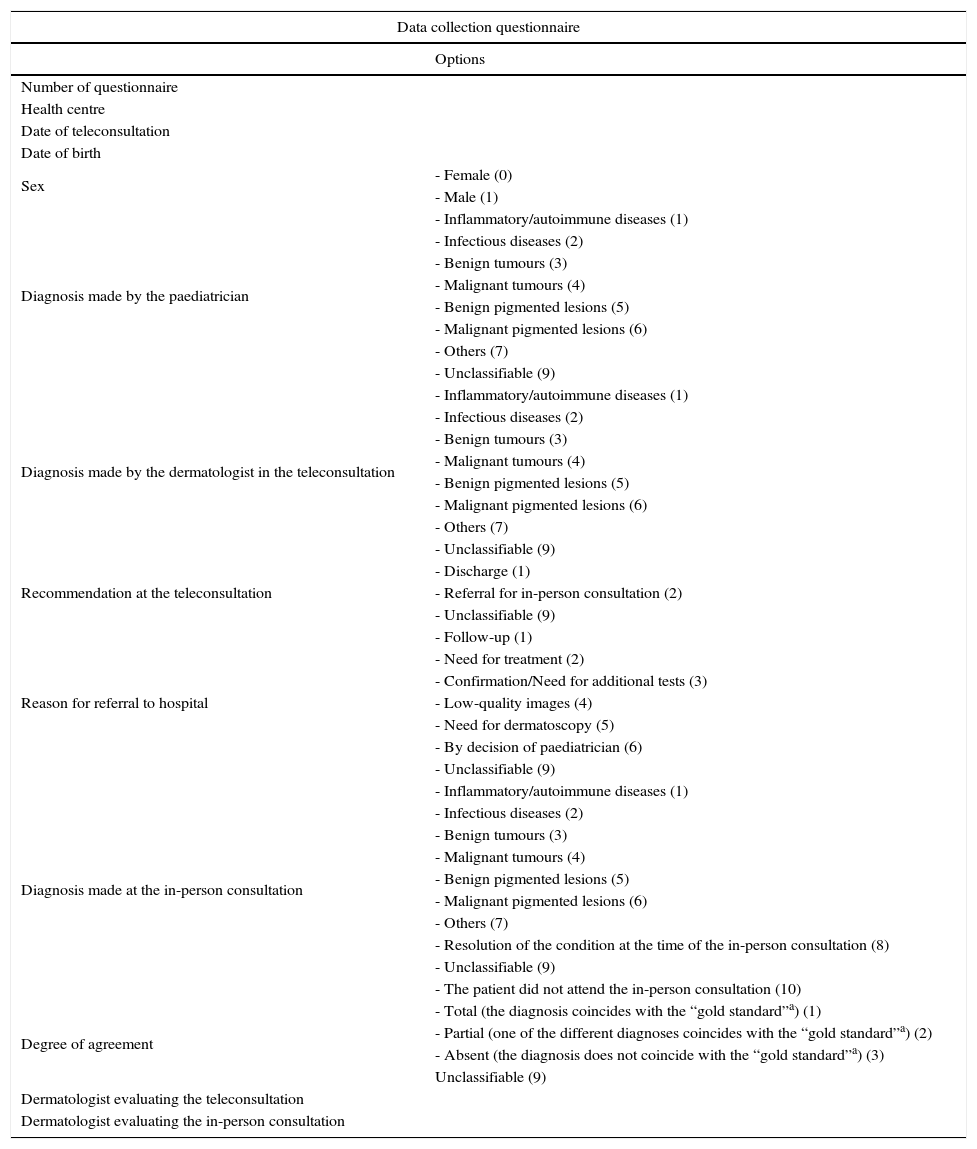
The following data were collected in the two computer programmes (SIGAP and IANUS): age and sex of the patient, health centre of origin, dermatologists who responded to the teleconsultation and the face-to-face consultation (if required), the diagnosis established by the paediatrician, by the dermatologist through the teleconsultation and by the dermatologist in the face-to-face consultation (if it took place), course of action recommended by the dermatologist through the teleconsultation, reason for deciding on referral for face-to-face consultation, and rate of agreement between the various diagnoses (between those given by the paediatrician and by the dermatologist through the teleconsultation and between those given by the dermatologist in the teleconsultation and by the dermatologist in the face-to-face consultation). The data collection form is shown in Table 1.
Data collection questionnaire.
| Data collection questionnaire | |
|---|---|
| Options | |
| Number of questionnaire | |
| Health centre | |
| Date of teleconsultation | |
| Date of birth | |
| Sex | - Female (0) |
| - Male (1) | |
| Diagnosis made by the paediatrician | - Inflammatory/autoimmune diseases (1) |
| - Infectious diseases (2) | |
| - Benign tumours (3) | |
| - Malignant tumours (4) | |
| - Benign pigmented lesions (5) | |
| - Malignant pigmented lesions (6) | |
| - Others (7) | |
| - Unclassifiable (9) | |
| Diagnosis made by the dermatologist in the teleconsultation | - Inflammatory/autoimmune diseases (1) |
| - Infectious diseases (2) | |
| - Benign tumours (3) | |
| - Malignant tumours (4) | |
| - Benign pigmented lesions (5) | |
| - Malignant pigmented lesions (6) | |
| - Others (7) | |
| - Unclassifiable (9) | |
| Recommendation at the teleconsultation | - Discharge (1) |
| - Referral for in-person consultation (2) | |
| - Unclassifiable (9) | |
| Reason for referral to hospital | - Follow-up (1) |
| - Need for treatment (2) | |
| - Confirmation/Need for additional tests (3) | |
| - Low-quality images (4) | |
| - Need for dermatoscopy (5) | |
| - By decision of paediatrician (6) | |
| - Unclassifiable (9) | |
| Diagnosis made at the in-person consultation | - Inflammatory/autoimmune diseases (1) |
| - Infectious diseases (2) | |
| - Benign tumours (3) | |
| - Malignant tumours (4) | |
| - Benign pigmented lesions (5) | |
| - Malignant pigmented lesions (6) | |
| - Others (7) | |
| - Resolution of the condition at the time of the in-person consultation (8) | |
| - Unclassifiable (9) | |
| - The patient did not attend the in-person consultation (10) | |
| Degree of agreement | - Total (the diagnosis coincides with the “gold standard”a) (1) |
| - Partial (one of the different diagnoses coincides with the “gold standard”a) (2) | |
| - Absent (the diagnosis does not coincide with the “gold standard”a) (3) | |
| Unclassifiable (9) | |
| Dermatologist evaluating the teleconsultation | |
| Dermatologist evaluating the in-person consultation | |
a “Gold standard”: the diagnosis established by the dermatologist at the teleconsultation, when analysing the agreement between this diagnosis and the one made by the paediatrician, or the diagnosis established by the dermatologist that conducted the face-to-face visit, when analysing the agreement between this diagnosis and the diagnosis made by the dermatologist that conducted the teleconsultation.
Cases in which a second teleconsultation was conducted with the same patient for technical reasons, because of computer errors or the absence of some element of the teleconsultation (lack of images, lack of clinical history) were regarded as redundant teleconsultations and were not taken into account for the final data analysis.
We grouped the diagnoses into seven disease categories: inflammatory conditions, infectious diseases, benign tumours, malignant tumours, benign pigmented lesions, malignant pigmented lesions and “other diagnoses”. Although this classification was arbitrary, it allowed us to have a larger number of patients in each group in order to make comparisons.
As regard the course of action to be determined by the dermatologist who conducted the teleconsultation, the possible options were “discharge” (care was prescribed without need for an in-person visit) or “referral for in-person consultation” (an instruction, whether some kind of care was prescribed or not, to request an appointment for face-to-face dermatological assessment, more or less urgently, depending on the diagnostic judgement). The reasons that led to a recommendation of referral for in-person consultation were classified into need for treatment, for follow-up or for confirmation of diagnosis and/or further tests, low-quality images and lack of dermatoscopic images. We also collected those cases in which “discharge” was recommended but the patients were referred for in-person consultation by the paediatrician.
We defined the degree of agreement as total if the diagnoses made for the same process by the paediatrician and the dermatologist assessing the teleconsultation, or by the dermatologist assessing the teleconsultation and the dermatologist who performed the face-to-face consultation were the same. The agreement was regarded as partial if several distinct diagnoses were made and at least one of them coincided with the “gold standard”. In the case of the diagnoses performed by the paediatrician and by the dermatologist assessing the teleconsultation, the “gold standard” was the one delivered by the dermatologist. In the cases of diagnoses made by the dermatologist who assessed the teleconsultation and by the one who conducted the in-person consultation, the “gold standard” was considered to be the one given by the latter and reinforced by the additional tests (dermatoscopy, taking samples for microbiological analysis, histology) if these were needed.
During the study period there was no paediatric dermatology specialty clinic in our service. However, all the dermatologists that assessed the virtual and face-to-face consultations had over 15 years’ experience or had a strong interest in paediatric dermatology, having completed rotations of several months’ duration in reference centres for this subspeciality.
The relevant release waivers for access to the patients’ clinical records were requested to carry out the study.
The data analysis was performed using the SPSS programme, version 22 (IBM Statistics, Chicago, USA).
ResultsWe obtained data from the hospital records on 218 teleconsultations. After eliminating the redundant consultations (n=28) and those for which the data were lost through computer errors (n=7), we finally evaluated 183 teleconsultations.
The mean age and standard deviation for the study population was 9±5 years, and 44% (81/183) of the patients were male.
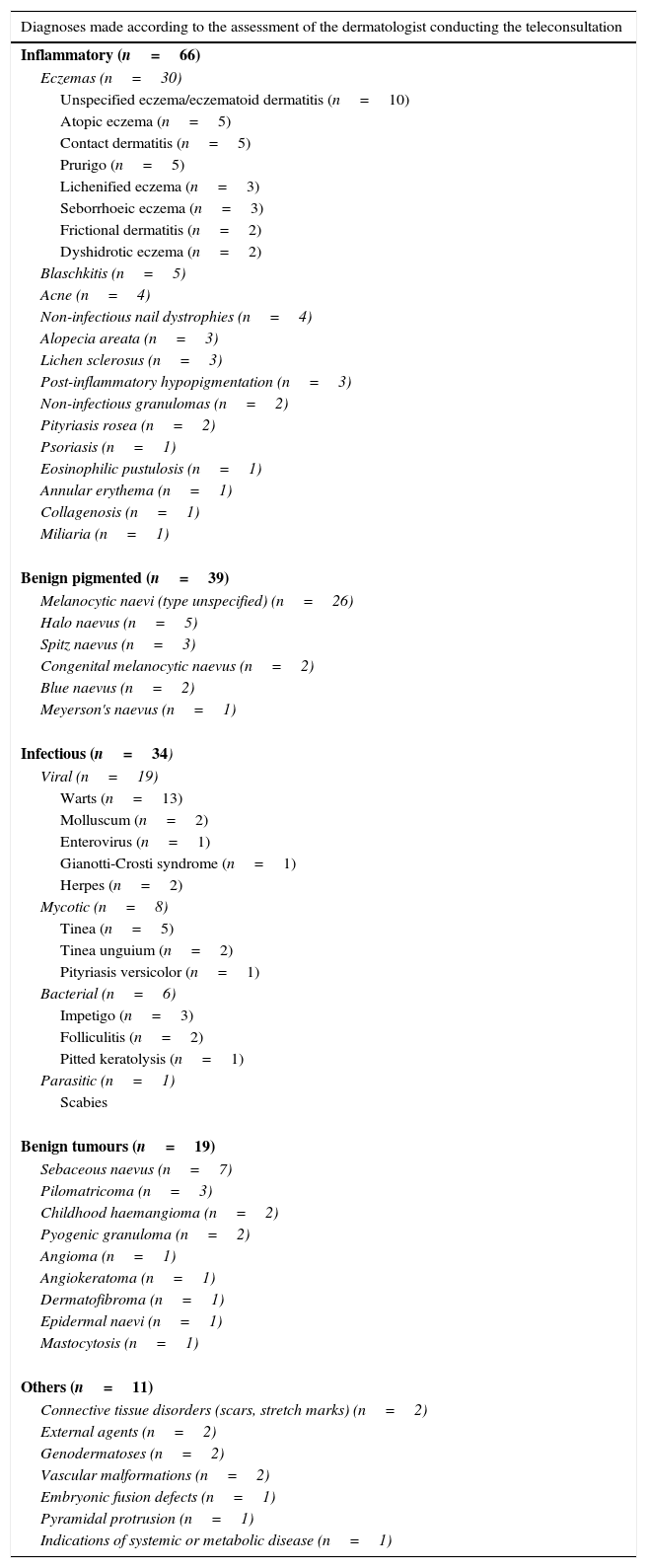
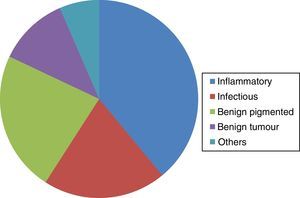
On the basis of the diagnosis made by the dermatologist in the teleconsultation, the most frequent diagnostic group was inflammatory conditions (39%; 66/169), followed by benign pigmented lesions (23%; 39/169) and infectious diseases (20%; 34/169) (Fig. 1). None of the consultations fell into the malignant pigmented lesions or malignant tumours groups. Table 2 indicates in detail the diseases assessed according to the diagnoses made by the dermatologist evaluating the teleconsultation. Of the paediatricians, 23% (42/183) did not indicate the suspected diagnosis on the teleconsultation form. In 9 of the 183 teleconsultations (5%) the evaluating dermatologist did not establish a diagnosis owing to the clinical history form not having been completed or to the poor quality of the image. In all these cases referral for face-to-face consultation or a second teleconsultation was recommended.
Diagnoses made according to the assessment of the dermatologist conducting the teleconsultation.
| Diagnoses made according to the assessment of the dermatologist conducting the teleconsultation |
|---|
| Inflammatory (n=66) |
| Eczemas (n=30) |
| Unspecified eczema/eczematoid dermatitis (n=10) |
| Atopic eczema (n=5) |
| Contact dermatitis (n=5) |
| Prurigo (n=5) |
| Lichenified eczema (n=3) |
| Seborrhoeic eczema (n=3) |
| Frictional dermatitis (n=2) |
| Dyshidrotic eczema (n=2) |
| Blaschkitis (n=5) |
| Acne (n=4) |
| Non-infectious nail dystrophies (n=4) |
| Alopecia areata (n=3) |
| Lichen sclerosus (n=3) |
| Post-inflammatory hypopigmentation (n=3) |
| Non-infectious granulomas (n=2) |
| Pityriasis rosea (n=2) |
| Psoriasis (n=1) |
| Eosinophilic pustulosis (n=1) |
| Annular erythema (n=1) |
| Collagenosis (n=1) |
| Miliaria (n=1) |
| Benign pigmented (n=39) |
| Melanocytic naevi (type unspecified) (n=26) |
| Halo naevus (n=5) |
| Spitz naevus (n=3) |
| Congenital melanocytic naevus (n=2) |
| Blue naevus (n=2) |
| Meyerson's naevus (n=1) |
| Infectious (n=34) |
| Viral (n=19) |
| Warts (n=13) |
| Molluscum (n=2) |
| Enterovirus (n=1) |
| Gianotti-Crosti syndrome (n=1) |
| Herpes (n=2) |
| Mycotic (n=8) |
| Tinea (n=5) |
| Tinea unguium (n=2) |
| Pityriasis versicolor (n=1) |
| Bacterial (n=6) |
| Impetigo (n=3) |
| Folliculitis (n=2) |
| Pitted keratolysis (n=1) |
| Parasitic (n=1) |
| Scabies |
| Benign tumours (n=19) |
| Sebaceous naevus (n=7) |
| Pilomatricoma (n=3) |
| Childhood haemangioma (n=2) |
| Pyogenic granuloma (n=2) |
| Angioma (n=1) |
| Angiokeratoma (n=1) |
| Dermatofibroma (n=1) |
| Epidermal naevi (n=1) |
| Mastocytosis (n=1) |
| Others (n=11) |
| Connective tissue disorders (scars, stretch marks) (n=2) |
| External agents (n=2) |
| Genodermatoses (n=2) |
| Vascular malformations (n=2) |
| Embryonic fusion defects (n=1) |
| Pyramidal protrusion (n=1) |
| Indications of systemic or metabolic disease (n=1) |
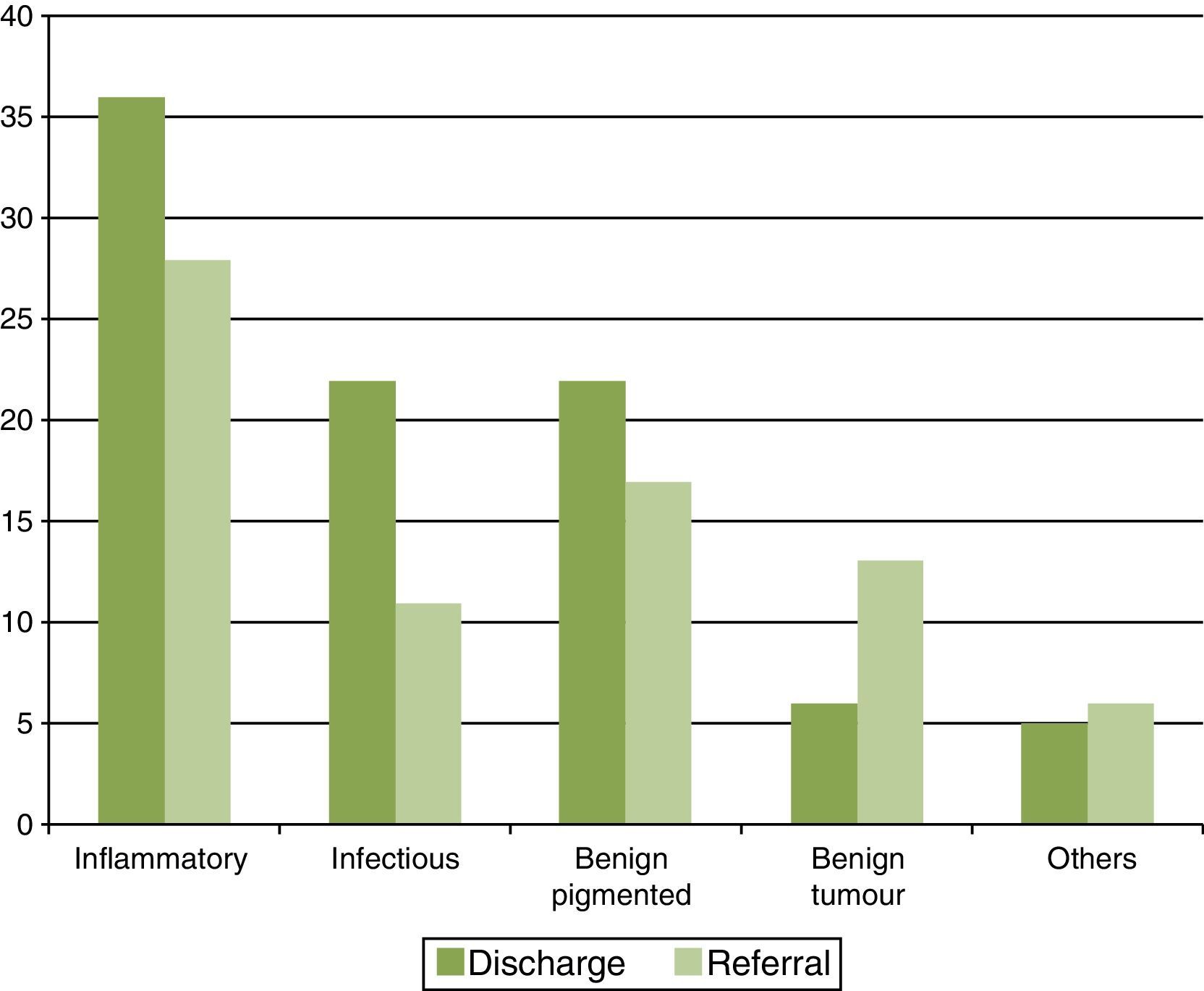
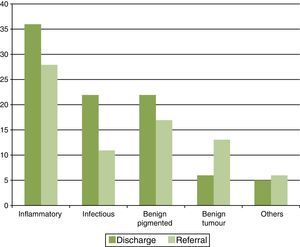
Slightly over half the teleconsultations (52%; 91/183) were resolved through the virtual programme, while 48% required an in-person visit (84/183). The percentages of discharges and referrals by disease group are shown in Fig. 2. The group with the highest percentage of cases in which referral was avoided was infectious diseases (67%), followed by the inflammatory conditions and benign pigmented lesions groups, which had equally high percentages of discharges (56%).
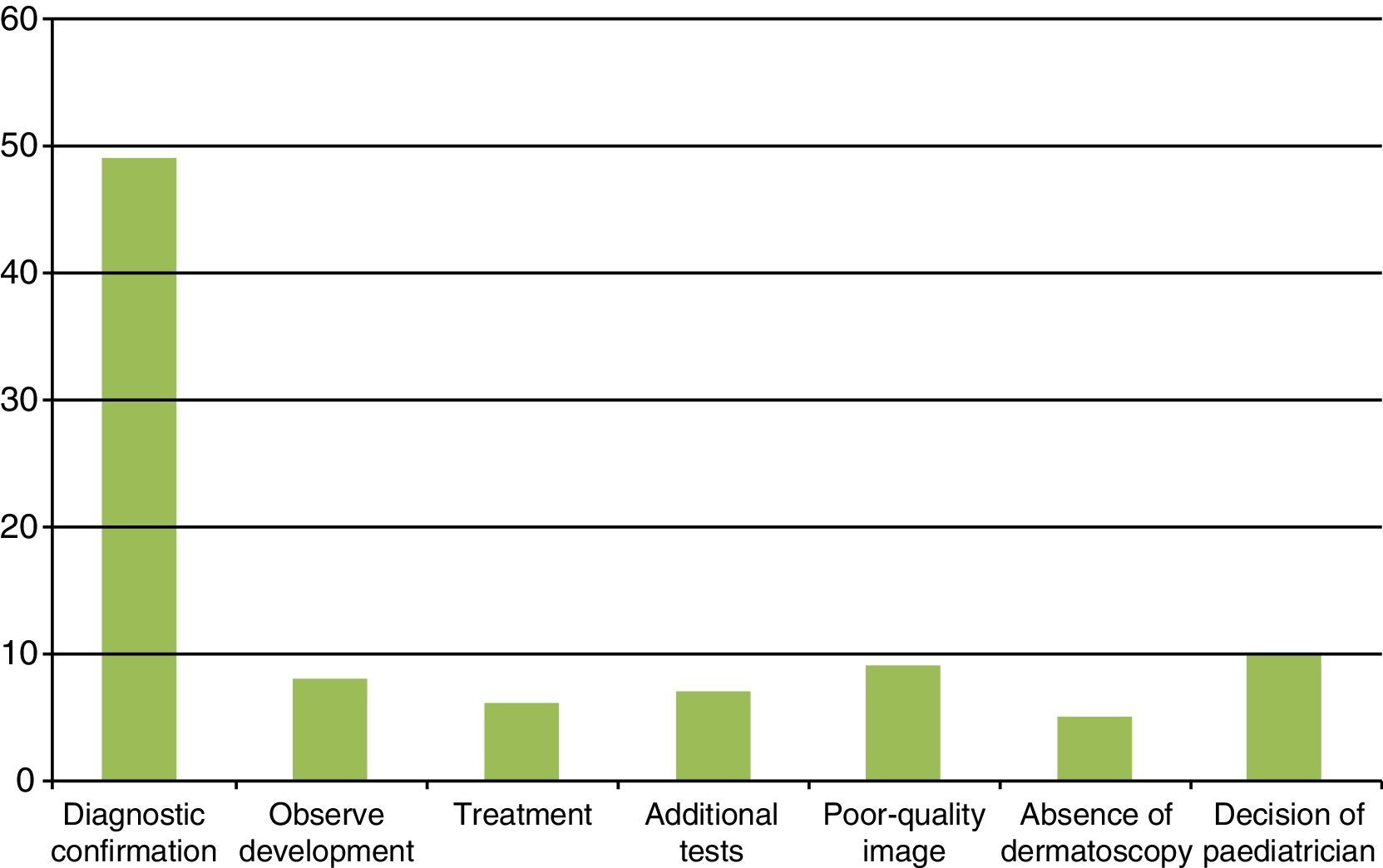
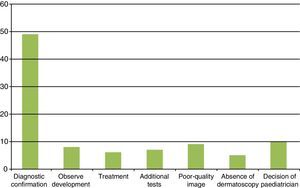
The most common reason that led the dermatologist conducting the teleconsultation to recommend an in-person consultation was the need for “diagnostic confirmation” in the face-to-face consultation (52%; 49/94). The distribution of this and the other reasons is shown in Fig. 3.
Diagnostic agreement was greater between the virtual diagnosis made by the dermatologist in the teleconsultation and the diagnosis established in the in-person dermatology consultation (total, 55% [36/65]; partial, 34% [22/65]; no correlation, 11% [7/65]) than between the diagnosis indicated by the paediatrician and that made by the dermatologist in the teleconsultation (total, 56% [75/133]; partial, 10% [13/133]; no correlation, 34% [45/133]).
DiscussionThere are few studies that evaluate the use of teledermatology in the paediatric age group. Moreover, these studies vary in the ages they cover and the objectives they assess.1,2,5–7
In general terms, as is the case when it is applied to the population in all age ranges, paediatric teledermatology has proved to be a useful tool as a filter, leading to a decrease in face-to-face consultations and shortening the times between referral and intervention. It facilitates increased access to specialist care and reduces the time patients spend travelling to hospital. Its potential for training has also been highlighted.2,7
It is difficult to compare the frequency of diseases in teledermatology consultations with that observed in face-to-face consultations due to the differences in diagnostic classifications between these two modes of working. In developed countries, atopic eczema, melanocytic naevi and viral warts tend to be the predominant reasons for in-person visits. Studies on Spanish paediatric patients observed that eczemas, of whatever origin, constituted the most frequent reason for in-person consultation in a paediatric dermatology specialty clinic, followed by infectious diseases (predominantly warts, molluscum infections and scabies), naevi and tumours (benign and malignant).3 More recently, another epidemiological study determined that the tumours group (represented primarily by melanocytic naevi) was in first place, followed by infections (predominantly viral warts) and eczemas (with atopic eczema as the most frequent group).4 In teledermatology, on the basis of the diagnosis made by the dermatologist in the teleconsultation, atopic eczema, naevi, common warts and molluscum infections are also the most common diagnoses.5,6 Similarly, in our study, the predominant groups were inflammatory conditions (mostly represented by eczemas), benign pigmented lesions, and infections (predominantly viral warts). These findings indicate that the reasons for consultation via teledermatology show a similar distribution of diseases to those referred through in-person visits.5
In the adult population, various national studies describe the type of diseases involved in teledermatology consultations. In one that included 917 patients, the highest frequency was observed in benign tumoral conditions (48%), followed by malignant tumoral conditions (32%); the remaining diagnostic groups (20%) were not specified. Seborrhoeic keratoses and melanocytic naevi, in the first group, and actinic keratoses followed by basocellular carcinoma, in the second, were the most common diagnoses.8 In a later study, but with a smaller number of patients (n=100), the predominant group was inflammatory conditions (22%), followed by tumoral diseases (20%) (with a higher percentage of benign tumours) and, further behind, infectious diseases (8%). The most prevalent diagnoses in each group were eczemas, melanocytic naevi and seborrhoeic keratoses, and viral warts, respectively.9
With regard to the percentage of referrals, Chen et al. observed the teleconsultations performed with 429 children under the age of 12 years. Only 6% were recommended to attend a face-to-face consultation and 1% were asked to have a second teleconsultation.5 The results of our study differ greatly from these figures and are closer to the percentage of discharges observed in teleconsultations in a predominantly adult population, which vary between 20% and 74% according to the series.10–14
Diagnostic agreement between virtual and in-person consultations is high. In studies that assess the population in all age groups, rates vary between 60% and 80% with respect to total agreement and 70% and 90% for partial agreement.9,15 In the paediatric population these percentages are also high. In a study that included 135 patients under the age of 18 years, a rate of agreement of 82% was observed between virtual and in-person consultations. The rate was lower (69%) in cases where one dermatologist conducted the teleconsultation and another carried out the face-to-face consultation.1 The second figure can be explained by the hypothesis that one always has a tendency to agree with oneself.1 However, this did not pose a problem in our study, since the virtual and in-person consultations were randomly distributed among the participating dermatologists.
Other studies, in line with our findings, have shown lower rates of agreement between the doctor who performed the teleconsultation and the dermatologist who evaluated it (58% agreement [48% total, 10% partial]).5
One of the main limitations of our study is the assumption that the diagnosis established by the dermatologist who evaluated the teleconsultation was correct compared with that delivered by the paediatrician. We believe that this does not affect the results obtained to any great extent, given the high rate of agreement (89%, taking into account both total and partial agreement) between the diagnoses made by the two dermatologists. It may also happen that to a certain extent the diagnostic judgement established by the paediatrician influences the diagnosis made by the dermatologist in the teleconsultation. In addition, we must draw attention to the small simple size, which makes it difficult to draw comparisons between subgroups. Furthermore, the retrospective design of our study, based solely on a review of computerised data, did not allow us to evaluate other aspects of this technique, such as the degree of satisfaction of the parents or of the paediatricians who carried out the teleconsultations. Finally, our results can only be extrapolated to our National Health System and those with a similar structure.
To conclude, we have observed that the diseases involved in teledermatology consultations show a similar distribution to in-person consultations. Approximately half the teleconsultations did not require subsequent in-person evaluation, with the infectious diseases group showing the highest percentage of avoidance. The rate of agreement between the dermatologist who conducted the teleconsultation and the one who performed the face-to-face consultation was high.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Batalla A, Suh-Oh HJ, Abalde T, Salgado-Boquete L, de la Torre C. Teledermatología en edad pediátrica. Observaciones en la práctica clínica diaria. An Pediatr (Barc). 2016;84:324–330.
Previous presentation at meetings, conferences or symposia: this study has been submitted and accepted for presentation in poster format at the 24th EADV Congress.