Toxic epidermal necrolysis (TEN) is an infrequent drug-induced skin disorder, with systemic involvement and characterised by extensive mucocutaneous detachment.1 Currently, there are no guidelines or standard of care specifying the most appropriate material for wound coverage.2
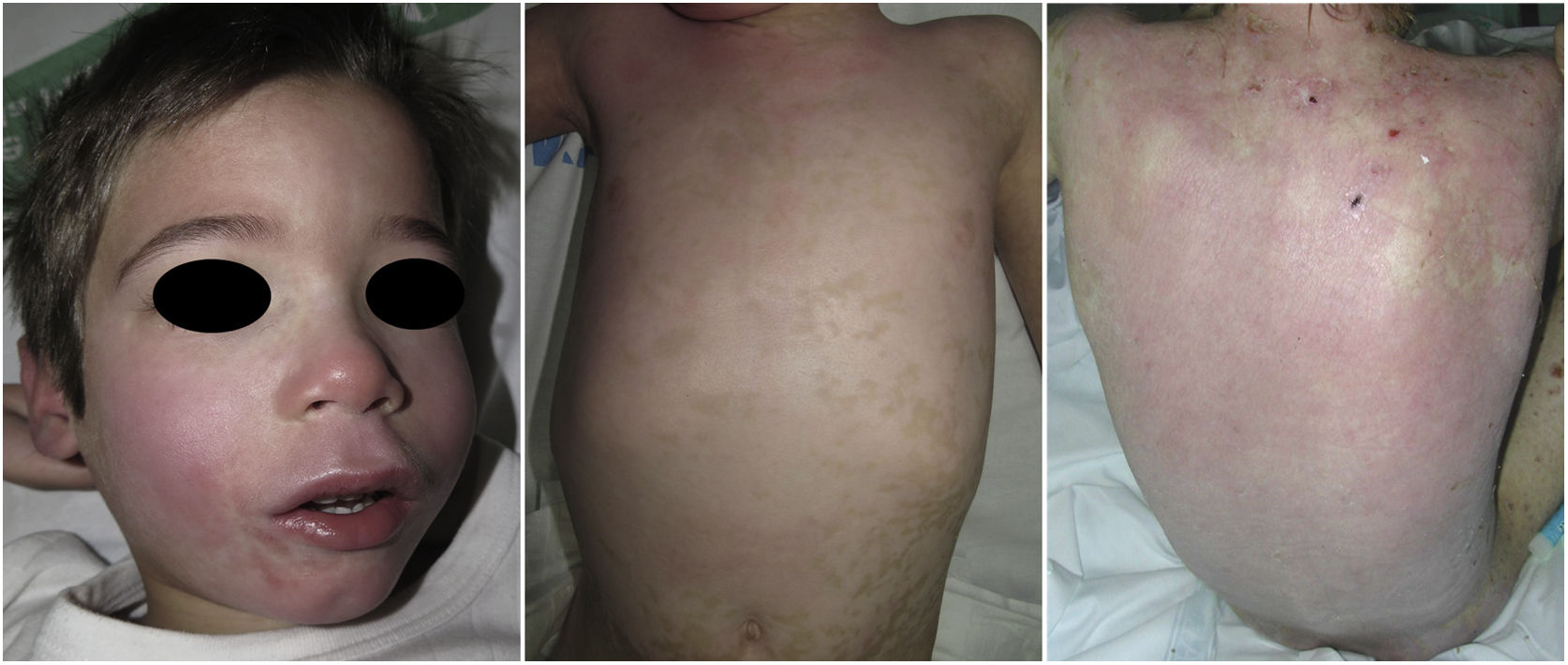
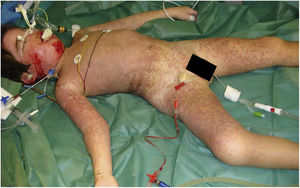
A boy aged 4 years who was receiving lamotrigine due to a history of ischaemic encephalopathy and epilepsy was admitted to the paediatric intensive care unit with a diagnosis of TEN. The patient presented with blistering over 60% of the total body surface area (Fig. 1) and extensive mucosal involvement, where the initial treatment consisted of intravenous fluid replacement and administration of cyclosporine A. The affected areas were debrided and covered with an alloplastic skin substitute (Suprathel®), a synthetic copolymer whose main component (70%) is lactic acid (Fig. 2). Suprathel-covered areas only required changing of the external dressings. After 16 days, this treatment had achieved complete re-epithelialization. The patient reported minimal or no pain during the healing process and dressing changes. At follow-up, he did not exhibit significant scarring or functional sequelae (Fig. 3).
Suprathel® is a very effective dressing for treatment of NET in children.3 It is easy to apply, requires minimum dressing changes, which improves patient comfort, prevents wound infection and promotes rapid healing, achieving satisfactory cosmetic and functional outcomes.
Ethics statementThe study was approved by the Ethics Committee of our hospital. The parents/legal guardians of the patient provided their informed consent in writing to the publication of the details of the case in this article.