Acute otitis media (AOM) is one of the most frequent causes of consultation and antibiotic prescription in pediatrics. The objective of this work is to evaluate the practice of delayed antibiotic prescription in AOM in pediatrics in primary care.
Material and methodsObservational, retrospective study, through reviewing of medical records in a Primary Care Center of Aragon Community of children with OMA in which doctors perform delayed prescription. Logistic regression analyzes possibly related to antibiotic prescription factors.
Results1390 episodes of AOM are analyzed in 696 patients. Immediate antibiotic prescription is performed in 67.6% (95% CI: 65.1–70.0%) of episodes, exclusive symptomatic in 13.7% (IC 95: 11.9–15.6%), and delayed antibiotic in 18.7% (IC 95: 16.7%–20.8%), finally being given in 53.5% (IC 95: 47.4–59.5%) of these. Factors significantly related to final antimicrobial dispensation in delayed prescription are aged between 0 and 2 years (OR 1.89, 95% CI: 1.25–2.87), bilaterality (OR 2.54, 95% CI: 1.48–4.35), ear pain (OR 0.49, CI 95: 0.29–0.82), fever (OR 2.67, IC 95: 1.95–3.65), bulging (OR 3,63; IC 95: 2,50–5,29) and otorrhea (OR 25.98; IC 95: 12.75–52.92). The same factors have influence on global prescription of antibiotics. Amoxicillin (74.6%) is the most indicated antibiotic, followed by Amoxicillin-Clavulanic (17.0%).
ConclusionsDelayed prescription in AOM seems to be useful to reduce antibiotics consumption, being necessary to advance in its implantation.
La otitis media aguda (OMA) es una de las causas más frecuentes de consulta y prescripción antibiótica en pediatría. Es objetivo de este trabajo valorar la prescripción antibiótica diferida en OMA en pediatría en atención primaria.
Material y métodosEstudio observacional, retrospectivo, mediante revisión de historias clínicas en un Centro de Salud urbano de la Comunidad Autónoma de Aragón de niños con OMA de tres cupos en los que los facultativos realizan prescripción diferida. Mediante regresión logística se analizan las variables posiblemente relacionadas con la prescripción antibiótica.
ResultadosSe analizan 1390 episodios de OMA en 696 pacientes. Se realizó prescripción inmediata de antibióticos en el 67,6% (IC 95: 65,1–70,0%) de episodios, sintomática exclusiva en el 13,7% (IC 95: 11,9–15,6%), y antibiótica diferida en el 18,7% (IC 95: 16,7%–20,8%), dispensándose finalmente el antimicrobiano en el 53,5% (IC 95: 47,4–59,5%) de estos últimos. Factores relacionados significativamente con la adquisición final antimicrobiana en prescripción diferida son la edad entre 0−2 años (OR 1,89; IC 95: 1,25–2,87), la bilateralidad (OR 2,54; IC 95: 1,48–4,35), la otalgia (OR 0,49; IC 95: 0,29–0,82), la fiebre (OR 2,67; IC 95: 1,95–3,65), el abombamiento (OR 3,63; IC 95: 2,50–5,29) y la otorrea (OR 25,98; IC 95: 12,75–52,92). Los mismos factores influyen en la prescripción global de antibióticos. Se indicó principalmente Amoxicilina (74,6%), seguido de Amoxicilina-Clavulánico (17,0%).
ConclusionesLa prescripción diferida en OMA parece útil para disminuir el consumo de antibióticos, siendo necesario avanzar en su implantación.
Acute otitis media (AOM) is one of the most frequent reasons for visits to primary care paediatric clinics and paediatric emergency departments and for antibiotic prescription.1–3 It can develop at any time in childhood, although it is most prevalent between ages 6 and 24 months.4 The incidence of AOM in children has decreased in recent years due to the introduction of conjugate vaccines against Streptococcus pneumoniae and Haemophilus influenzae type b and the application of more restrictive diagnostic criteria,5–8 but it continues to be very frequent, with an estimated proportion of children that have experienced at least one episode of AOM of 50% in our region.9
Appropriate treatment requires an accurate diagnosis of AOM and identification of the cases requiring antibiotherapy, thereby preventing its unnecessary use. This avoids excessive use of antibiotics and the adverse effects that they may have, including the increase in drug-resistant bacteria.
In this regard, one of the goals established for paediatric primary care in the National Plan on Antibiotic Resistance of 2017 in Spain was to reduce the use of antibiotics for treatment of AOM, with the rationale that management with analgesia alone for 48 h, in certain cases, and delayed prescribing with administration depending on the course of disease and/or reassessment would result in resolution in most episodes.10 Immediate antibiotherapy would be indicated in infants aged less than 6 months or in the presence of otorrhoea, bilateral AOM, severe unilateral AOM, AOM in an immunosuppressed patient or in a patient in whom adequate follow-up is not possible. A systematic review published in 2015 did not find differences between immediate prescribing and the approach consisting of analgesia and observation in the time elapsed to alleviation of pain, the number needed to treat to avoid 1 case of tympanic membrane perforation or severe complications. There were differences, although not statistically significant, in the proportion of patients that experienced recurrence, which was higher in the group that received immediate antibiotherapy.11
The available evidence on the real-world practice of delayed prescribing in the management of AOM in the paediatric population in developed countries is scarce. A Cochrane systematic review found that 30%–40% of patients of any age that receive a delayed antibiotherapy prescription end up using the drug (compared to 93% in the case of immediate prescribing), which corresponds to a substantial reduction in the use of antibiotics12 and therefore in health care costs.13,14 For this reason, we aimed to study this approach to management in more detail.
The objective of our study was to assess practices of antibiotic prescribing for the management of AOM through a review of electronic health records (EHRs) and pharmacy dispensation data. Within this analysis, we aimed to assess the effectiveness of delayed antimicrobial prescribing in reducing unnecessary use of antibiotics in the management of AOM in children at the primary care level.
Material and methodsWe conducted a retrospective observational study through the review of electronic health records in the primary care health information system (known as OMI-AP) of the Autonomous Community of Aragon, identifying children with a diagnosis of AOM from the moment that electronic prescriptions became available in the system. We collected data corresponding to 3 paediatric caseloads in a primary care centre of the city of Zaragoza, Spain, managed by clinicians that reported practicing delayed prescribing for the management of AOM.
We did not perform a sample size calculation, as this was an analysis of real-world clinical practice that included every episode of AOM that met the inclusion criteria.
Inclusion criteria: patient aged less than 15 years with a diagnosis of one or more episodes of AOM documented in the OMI-AP electronic health record database by one of the 3 paediatricians in charge of the caseloads. The diagnosis of AOM was based on the most recent consensus criteria established in Spain15 and the judgment of the physician in charge (all three paediatricians had more than 25 years of professional experience) supported by the findings of conventional otoscopy.
Exclusion criteria: presence of chronic treatment or disease that could compromise the immune response or disease of the ear, nose or throat of any severity that could affect the conventional management of AOM (for example, patients with ear tubes). Age less than 2 months, as these infants require inpatient treatment.
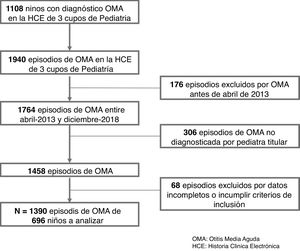
Fig. 1 presents a flow chart of how the episodes were selected.
Study variables- •
Primary variable: any form of treatment prescribed by a paediatrician for AOM (exclusive analgesia, delayed or immediate antibiotic prescription). In the case of delayed prescribing, we also studied whether it had been administered or not (we assumed that any dispensed medication was actually given to the patient, although we recognise the limitations of this assumption). The decision to administer delayed antibiotherapy was made by the carers of the patient, who were informed at diagnosis of the circumstances under which it should be given (fever, ear discharge and persistence of symptoms despite analgesia).
- •
Secondary variables: age at time of episode, sex, number of previous episodes of AOM, location of otitis, clinical characteristics (earache, fever, overall health) and features found in the examination (bulging, hyperaemia, otorrhea) at diagnosis, specific antibiotic agent (if administered) and prescribed duration of antibiotherapy.
In the descriptive analysis, we calculated measures of central tendency and dispersion for each quantitative variable. We have expressed the results of qualitative variables as percentages with the corresponding 95% confidence interval (CIs).
In the inferential analysis, to assess the potential association with variables that may have influenced the administration of antibiotherapy, we calculated odds ratios (ORs) with the corresponding 95% CIs. To assess the statistical significance of differences in quantitative variables, we used the Student t test or, if the normality assumption was not met, the Mann–Whitney U test. In the case of qualitative variables, we did the assessment by means of the χ2 test. We also performed a univariate analysis of the variables considered a priori as involved in therapeutic decision-making followed by a multivariate analysis through multinomial logistic regression. The analysis was performed with the software SPSS Statistics® version 21. In every analysis, statistical significance was defined as a P value of less than 0.05.
The study was approved by the Clinical Research Ethics Committee of Aragon under research project number 19/099, of March 13, 2019, and conducted in adherence with applicable national law (Law 14/2007 on biomedical research), and international ethics standards (Declaration of Helsinki of the World Medical Association on the ethical principles for medical research involving human subjects, Brazil, 2013). Data were anonymised and used exclusively for the purposes of the study after obtaining the authorization of the director of the primary care system of Aragon. The research team committed to safeguarding the confidentiality of patients in adherence with Organic Law 3/2018 of 5 December on the Protection of Personal Data and Guarantee of Digital Rights.
We retrieved information from 2 databases: the OMI-AP electronic health records database and the pharmacy electronic prescription stocking and dispensation database for March and April of 2019.
ResultsThe analysis included 1390 episodes of AOM in 696 patients included in 3 primary care paediatrics caseloads of a single primary care centre that were diagnosed by the paediatrician in charge between April 2013 and December 2018.
Most episodes took place in the months of autumn and spring (Fig. 2). The mean number of episodes per child was 1.997, with a slight predominance of male patients (54.9%) versus female patients (45.1%).
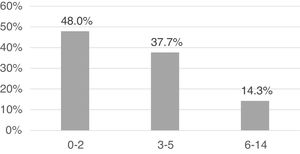
The mean decimal age at the time of the episode was 3.6 (standard deviation [SD], 2.5; range, 0.1–13.9). As can be seen in Fig. 3, the analysis by age group revealed that the distribution was skewed toward infancy, with the highest frequency of AOM episodes in the group aged 0–2 years (48.0%). Further dividing the age group by sex, we found that in the group aged 0–2 years, the risk of AOM was higher in boys (52.0%; 95% CI, 48%–56%) compared to girls (43.1%; 95% CI, 39%–47%) (OR, 1.43; 95% CI, 1.16–1.77; P = .002), with no differences based on age in any other age groups.
In 69.8% of the episodes, the patients had a previous history of AOM. The location of disease was the right ear in a majority of cases (46.2% compared to 37.2% in the left), with bilateral involvement in 13.6% of cases. In most episodes, AOM manifested with fever (52.7%), otalgia (64.1%), bulging of the tympanic membrane (66.8%) and tympanic hyperaemia (67.3%). Otorrhoea was present in 23.8% of episodes.
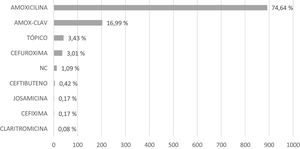
The approach to treatment was immediate prescribing of antibiotherapy in 67.6% episodes (95% CI, 65.1%–70.0%), exclusive symptomatic treatment in 13.7% (95% CI, 11.9%–15.6%), and delayed antibiotic prescribing in 18.7% (95% CI, 16.7%–20.8%). Of the overall prescriptions for antibiotherapy (either immediate or delayed), 87.3% were dispensed. Amoxicillin was the antibiotic agent prescribed most frequently (74.6%), followed by amoxicillin-clavulanic acid (17.0%), with prescription of ear drops for topical treatment in 3.4% of the cases. Fig. 4 details the rest of the prescribed antibiotics. The mean prescribed duration of antimicrobial treatment was 7.2 days (SD, 1.1), with a longer duration in the group aged 0–2 years (mean, 7.5 days, SD, 1.0).
Overall, as summarised in Table 1, in 76.7% of the episodes (95% CI, 74.4−78.9), the prescribed antibiotic agents were dispensed, including immediate and delayed prescriptions, and the percentage was higher in children aged 0–2 years (84.6%), compared to those aged 3–5 years (71.6%). However, there were no differences between the 3-to-5 and the 6-to-14 years age groups.
Univariate analysis of the association of the different variables at diagnosis with the overall percentage of dispensed antibiotherapy prescriptions (immediate and delayed). Odds ratio (OR) for dispensation of antibiotherapy for the different variables.
| % dispensation of antibiotics (95% CI; n) | OR | 95% CI | |
|---|---|---|---|
| Age group | |||
| 0−2 years | 84.6 (84.3−87.9; 548) | 2.18* | 1.63−2.90 |
| 3−5 years | 71.6 (67.7−75.5; 365) | 1.41** | 0.99−2.01 |
| 6−14 years | 64.1 (55.2−68.6; 123) | ||
| Previous episodes | |||
| Yes | 74.4 (71.6−77.2; 699) | ||
| No | 82.0 (78.3−85.7; 337) | 1.56 | 1.17−2.09 |
| Laterality | |||
| Bilateral | 84.9 (79.8−90.1; 158) | 1.83 | 1.2−2.8 |
| Unilateral | 75.5 (73.0−78.0; 848) | ||
| Fever | |||
| Yes | 85.3 (82.7−87.9; 603) | 2.97 | 2.27−3.88 |
| No | 66.1 (62.4−69.9; 404) | ||
| Otalgia | |||
| Yes | 70.5 (67.5−73.6; 608) | ||
| No | 87.7 (84.7−90.7; 399) | 2.98 | 2.17−4.08 |
| Bulging | |||
| Yes | 79.2 (76.6−81.9; 716) | 1.57 | 1.21−2.05 |
| No | 70.7 (66.4−75.2; 293) | ||
| Hyperaemia | |||
| Yes | 74.1 (71.3−77.0; 673) | ||
| No | 81.9 (78.2−85.6; 335) | 1.58 | 1.18−2.12 |
| Otorrhoea | |||
| Yes | 95.1 (92.7−97.4; 307) | 7.98 | 4.74−13.43 |
| No | 70.6 (67.8−73.5; 707) | ||
| Overall administration of antibiotics | 76.7 (74.4−78.9; 1036) | ||
The multivariate analysis of signs and symptoms, the results of which are presented in Table 1, found statistically significant differences in the percentages of antibiotic drug dispensation between children without a previous history of AOM (82% of cases with a final prescription) and with a history of AOM (74.4%); between children with bilateral AOM (84.9%) and unilateral AOM (75.5%); between children that presented with fever (85.3%) and without fever (66.1%); between children that presented with otalgia (87.7%) and without otalgia (70.5%); between children in whom the examination detected tympanic membrane bulging (79.2%) versus those in whom these feature was not identified (70.7%); in children without tympanic hyperaemia (81.9%) compared to those that did present with it (74.1%); and between children with otorrhoea (95.1%) versus children without (70.6%).
The univariate analysis, which is not included in Table 1, did not find differences in the frequency of dispensation in the overall sample between female patients (76.7%; 95% CI, 73.4%–80.1%) and male patients (76.7%; 95% CI, 73.7%–79.8%).
In the group of episodes with delayed prescribing, which corresponded to 18.7% of the total, the prescribed antibiotic agent was finally dispensed in half the cases (53.46%). Table 2 presents the overall percentage of prescriptions that were eventually dispensed in the group of delayed prescriptions and the results of the univariate analysis of the variables that could influence it. The percentage of children in whom delayed prescriptions were dispensed was significantly higher in the group aged 0–2 years (63.0%) compared to the group aged 6–14 years (36.6%), and also in the latter group compared to the group aged 3–5 years (56.4%). The percentage of prescriptions that were eventually dispensed after delayed prescribing was also significantly higher in patients with bilateral AOM compared to unilateral (91.7% vs 53.9%) and patients with fever compared to without (63.5% vs 50.3%). We did not find differences in the proportion of dispensed prescriptions between girls (59.5%) and boys (51.9%), or based on the past history of AOM or the presence or absence of otalgia, bulging, hyperaemia or otorrhoea.
Univariate analysis of the association of the different variables at diagnosis with the percentage of dispensation of delayed antibiotherapy prescriptions. Odds ratio (OR) for the dispensation of antibiotics following delayed prescribing in association with the different variables.
| % Dispensed of total prescribed (95% CI; n) | OR | 95% CI | |
|---|---|---|---|
| Age group | |||
| 0−2 years | 63.0 (53.2−72.9; 58) | 1.32* | 0.75−2.31 |
| 3−5 years | 56.4 (47.2−65.5; 66) | 2.24** | 1.08−4.67 |
| 6−14 years | 36.6 (21.8−51.3; 15) | 2.96*** | 1.38−6.35 |
| Previous episodes | |||
| Yes | 52.3 (45.3−59.2; 103) | ||
| No | 57.1 (44.9−68.6; 36) | 1.09 | 0.61−1.93 |
| Laterality | |||
| Bilateral | 91.7 (64.6−98.5; 11) | 9.42 | 1.2−74.13 |
| Unilateral | 53.9 (47.5−60.3; 125) | ||
| Fever | |||
| Yes | 63.5 (53.9−73.2; 61) | 1.72 | 1.02−2.90 |
| No | 50.3 (42.4−58.5; 77) | ||
| Otalgia | |||
| Yes | 52.7 (46.1−59.2; 116) | ||
| No | 57.9 (42.2−72.2; 22) | 1.11 | 0.55−2.24 |
| Bulging | |||
| Yes | 54.4 (47.9−60.7; 124) | 1.64 | 0.71−3.78 |
| No | 40.7 (24.5−59.3; 11) | ||
| Hyperaemia | |||
| Yes | 50.3 (43.0−57.6; 88) | ||
| No | 58.2 (47.2−68.5; 46) | 1.46 | 0.84−2.54 |
| Otorrhoea | |||
| Yes | 33.3 (9.7−70.0; 2) | ||
| No | 53.2 (47.0−59.3; 132) | 1.85 | 0.3−11.28 |
| Total | 53.46% (47.4−59.4; 139) | ||
Amoxicillin-clavulanic acid was prescribed in 20.98% of episodes in patients with a history of AOM (compared to 8.27% in the absence of previous episodes) and cefuroxime in 4.27% (compared to 0.27%).
Table 3 presents the results of the logistic regression analysis that included the factors considered a priori to influence the dispensation of antibiotherapy for management of AOM. The resulting model showed that age 0–2 years, bilateral otitis, fever, bulging, otorrhoea and absence of ear pain had a significant impact on the dispensation of antibiotherapy in patients with a diagnosis of AOM.
Analysis of the association of the study variables at the time of diagnosis with dispensation of antibiotics for treatment of acute otitis media, results expressed as odds ratios obtained through logistic regression.
| OR | 95% CI | P | |
|---|---|---|---|
| 0−2 years | 1.65 | 1.05−2.61 | .03 |
| 3−5 years | 1.02 | 0.68−1.55 | .91 |
| Previous episodes | 0.95 | 0.66−1.35 | .76 |
| Bilateral otitis | 1.69 | 1.04−2.75 | .04 |
| Fever | 2.77 | 1.98−3.88 | .00 |
| Bulging | 4.60 | 3.22−6.58 | .00 |
| Otorrhoea | 32.95 | 16.59−65.43 | .00 |
| Hyperaemia | 1.32 | 0.92−1.9 | .13 |
| Otalgia | 0.58 | 0.39−0.88 | .01 |
Similarly, the factors at diagnosis that increased the likelihood of antibiotic dispensation following delayed prescription were aged 0–2 years, bilateral otitis, fever, bulging, absence of ear pain and otorrhoea, as can be seen in Table 4.
Analysis of the association of the study variables at the time of diagnosis with dispensation of antibiotics following delayed prescription, results expressed as odds ratios obtained through logistic regression.
| OR | 95% CI | P | |
|---|---|---|---|
| 0−2 years | 1.89 | 1.25−2.87 | .00 |
| 3−5 years | 1.24 | 0.86−1.80 | .25 |
| Previous episodes | 0.89 | 0.64−1.25 | .51 |
| Bilateral otitis | 2.54 | 1.48−4.35 | .00 |
| Fever | 2.67 | 1.95−3.65 | .00 |
| Bulging | 3.63 | 2.50−5.29 | .00 |
| Otorrhoea | 25.98 | 12.75−52.92 | .00 |
| Hyperaemia | 1.13 | 0.81−1.57 | .47 |
| Otalgia | 0.49 | 0.29−0.82 | .01 |
We conducted a study that included a large number of patients and episodes managed at the primary care level. The descriptive data obtained in our study were consistent with the reviewed evidence,9 with a slight predominance of male versus female patients with AOM, a higher incidence in the autumn months and a much higher prevalence (nearly half the episodes) in children under 2 years.
Nearly 2 out of 3 children with a diagnosis of AOM in our case series received an immediate prescription for antibiotherapy, and nearly 9 out of 10 of prescriptions were dispensed. Amoxicillin was the most frequently prescribed antibiotic (74.6%) followed by amoxicillin-clavulanic acid (17%), with a mean duration of prescribed treatment of 7.2 days, as reflected in the literature.16 Antibiotic use was more frequent in children aged 0–2 years, as was also described in a review published by Ivanovska that found that antibiotics were prescribed to 52.4% of patients in this age range.17 We also found a significantly higher frequency of prescription in children with no previous history of AOM and children with bilateral AOM, fever, tympanic membrane bulging or otorrhoea. The latter, along with the presence of bilateral otitis, are clear indications for immediate antibiotherapy.18 Age less than 2 years has been considered an indication for immediate prescription in less recent guidelines and consensus recommendations,15,19,20 while in more recent guidelines, age is considered an indication for immediate antibiotherapy only in infants aged up to 6 months.21–24 It may seem surprising that the absence of ear pain or of hyperaemia is associated with more frequent dispensation of antibiotics, but it must be because otalgia is much less frequent in cases of suppurative otitis media and hyperaemia is harder to assess, both aspects that must be taken into account in the interpretation of these results.
Delayed prescribing was an infrequent practice (18.71% of episodes), although the recommended exclusive symptomatic treatment was even less frequent (13.74%). Still, it is important to consider that the outcome of delayed prescribing may be exclusive symptomatic treatment, which means that the frequency of the latter may be underestimated. The frequency of delayed prescribing was low compared to other case series,11,25,26 but in our study, in nearly half the cases (53.5%) the prescribed antibiotic agent was not ultimately dispensed. This percentage was even lower in the group of patients aged 6–14 years (antibiotic administered in 1 out of 3 episodes with delayed prescription). The factors at diagnosis that were significantly associated with the dispensation of the antibiotic agents following delayed prescription were age less than 2 years, bilateral otitis, absence of otalgia and presence of fever, bulging or otorrhoea.
In the overall multivariate analysis, we found that age 0–2 years, bilateral AOM, fever, otalgia, bulging and otorrhoea were factors significantly associated with antibiotic dispensation. This was consistent with the findings of a systematic review conducted by Rothman, which found that tympanic membrane bulging was the sign associated with the greatest probability of diagnosis of AOM and antimicrobial treatment (positive likelihood ratio, 51; 95% CI, 36–73).27
In our study, we analysed the approach to AOM, a disease that is very prevalent in the paediatric population. There are biases and limitations to our study. There was significant variation in the use of delayed prescribing between clinicians (data not shown, 2 of them used this approach in fewer than 10% of the episodes while the remaining paediatrician used it in 38.3%). The study was retrospective, and therefore the accuracy of diagnosis was not as high as it would have been in the case of a prospective study, in which abnormal findings of tympanometry/pneumatic otoscopy and discharge from the middle ear would have been the main criteria for diagnosis of AOM.28 In addition, the data on the variable “administration of treatment” was based on whether the prescribed drug was dispensed at the pharmacy with the assumption that prescribed drugs were actually administered, with the exception of those cases in which the lack of administration following dispensation was documented in the health records. It would have made a significant difference if we could have obtained more reliable information for this variable, for example, through telephone calls to the family in the context of a prospective study, but we did not consider this option for our study due to the risk of recall bias. Another aspect that would be interesting to explore in future research would be documenting and analysing the reasons why parents end up choosing to administer the antibiotic and the association of these reasons with other factors, such as socioeconomic status, educational attainment or the understanding of the mechanism of action and application of antibiotics. Some studies conducted in Europe assessed the influence of parents on clinicians when it comes to antimicrobial prescription,29 highlighting that up to 40% of parents refuse the watchful waiting option for management of paediatric AOM.30
In conclusion, in our region, delayed prescribing of antibiotherapy for management of AOM seems to be an infrequent practice, and approximately half of prescribed antibiotics are dispensed following delayed prescribing, with age less than 2 years, fever, bulging, bilateral disease and otorrhoea making administration of the prescribed antibiotic more likely. The delayed prescribing approach for management of AOM could be a useful strategy to reduce unnecessary use of antibiotics. However, more frequent delayed prescribing should be actively promoted over immediate prescribing given the likelihood of AOM to resolve spontaneously.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: García Ventura M, García Vera C, Ruiz-Canela Cáceres J, Abordaje terapéutico de la otitis media aguda en atención primaria de un área urbana. Evaluación de la prescripción diferida de antibióticos, Anales de Pediatría. 2022;96:422–430.
Presentación previa congresos: Los resultados de este artículo fueron presentados en forma de Comunicación Oral en el 17 °Congreso de la Asociación Española de Pediatría de Atención Primaria (AEPap), Madrid 13–15 febrero 2020.