Thyroglossal cysts are the most frequent neck malformation in children. They are usually located in the anterior midline near the hyoid bone, and may appear at the lingual (2.1%) or suprasternal (12.9%) level. Their presentation as a solitary thyroid nodule (STN) has been described in the literature and poses a challenge in the differential diagnosis of thyroid disorders in children.
We present two cases that illustrate the clinical presentation and diagnostic test findings of this disease.
The first patient was a boy 2 years of age presenting with a nodule in the right side of the neck, painless, well-defined, and adhered to the deep planes. Ultrasound examination showed a cystic nodule 8mm×11mm×17mm in the thyroid. Iodine-131 scintigraphy showed a cold nodule and homogeneous uptake through the rest of the gland. The thyroid function tests were normal.
Surgery was performed to reach a definitive diagnosis, revealing a cyst with mucinous contents in the upper right lobe of the gland compatible with thyroglossal duct cyst. The lesion was surgically resected and the histopathological study confirmed the diagnosis.
The second case corresponded to a boy 10 years of age with a painless nodule in the medial edge of the sternocleidomastoid muscle. Ultrasound examination showed a cystic lesion in the right thyroid lobe measuring 11mm×6mm×20mm. Scintigraphy showed a cold nodule. A fine needle aspiration puncture (FNAP) was performed, revealing a squamous epithelium and the absence of colloid material or follicular tissue, suggestive of a thyroglossal cyst.
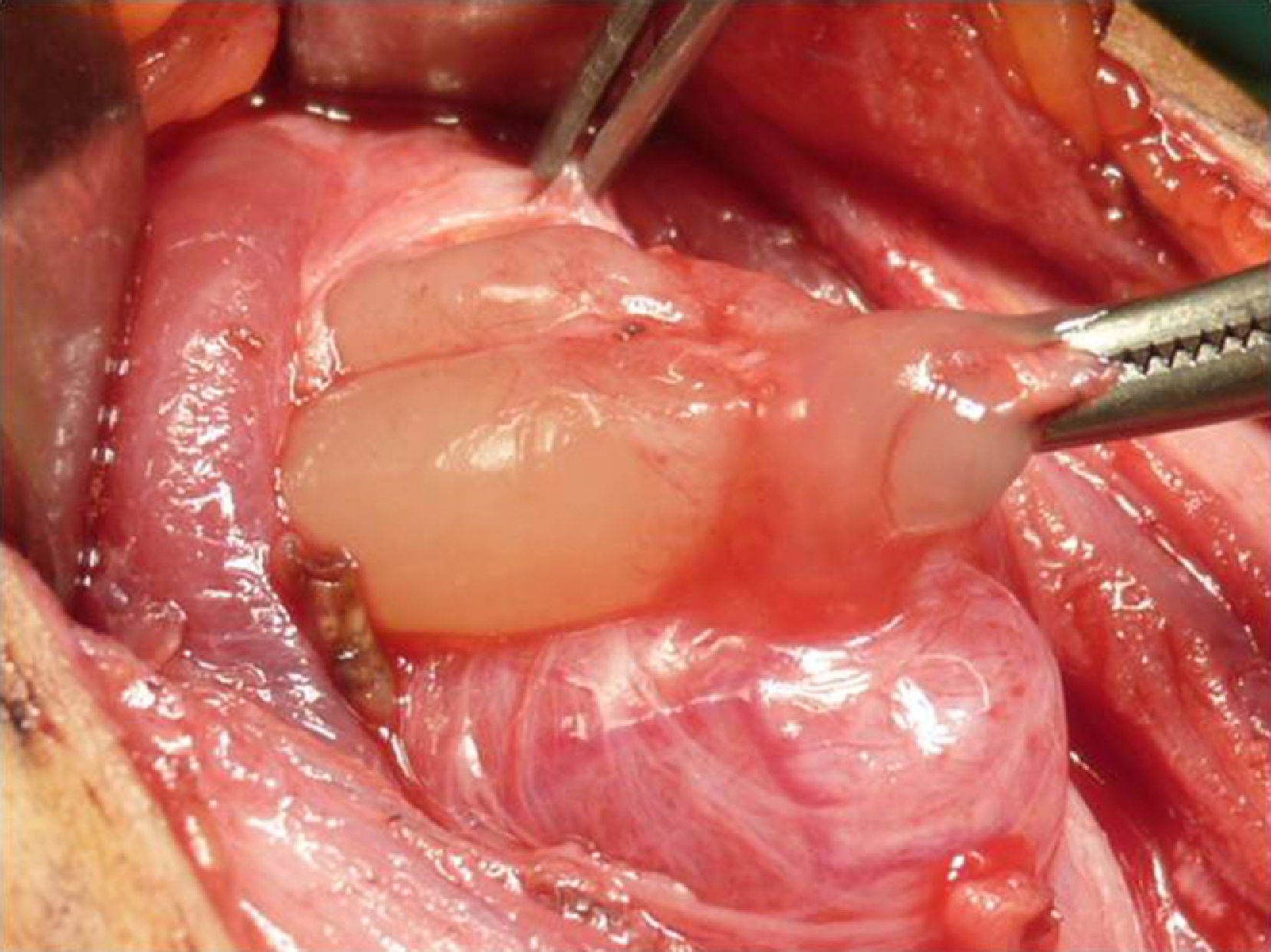
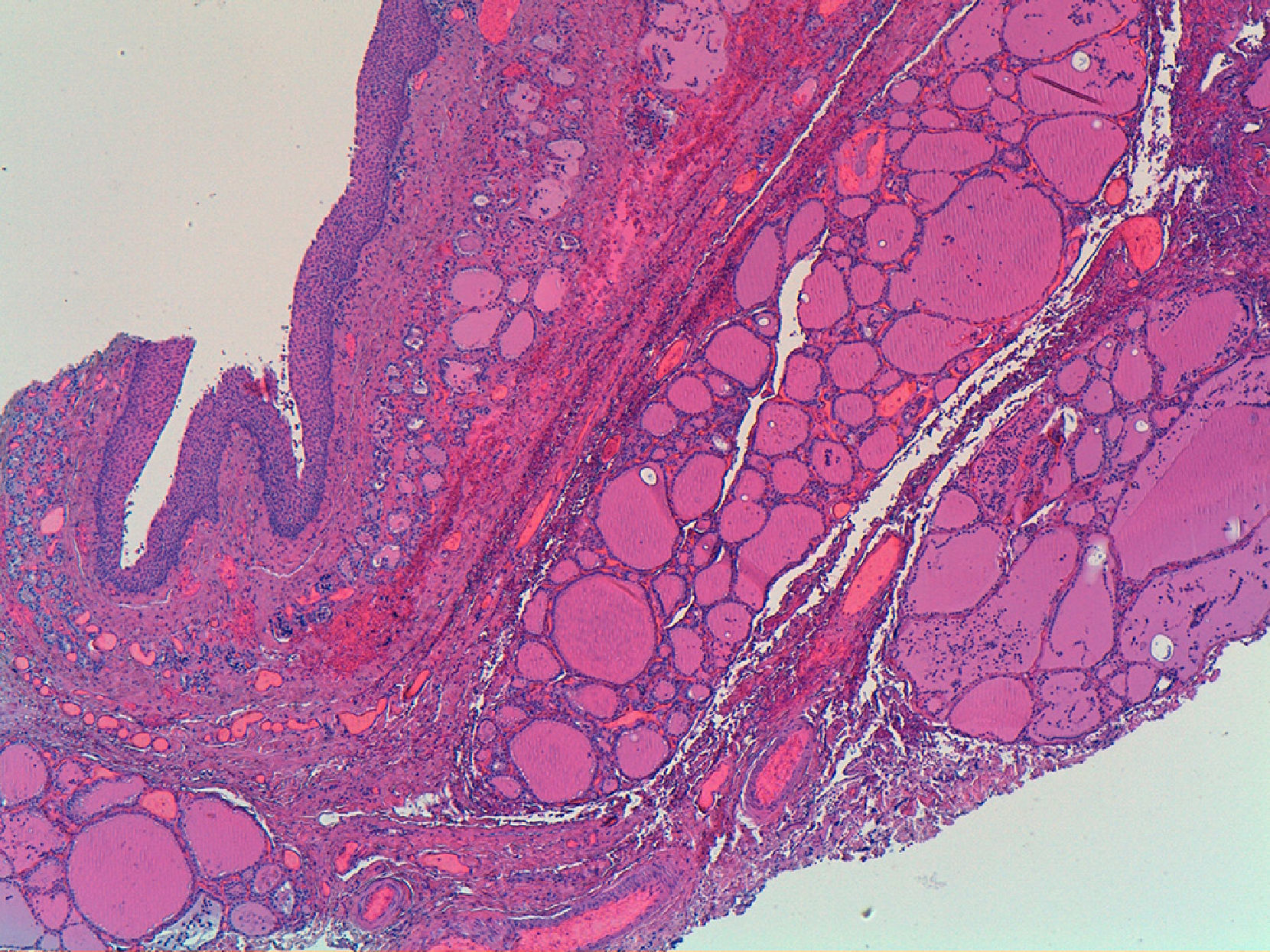
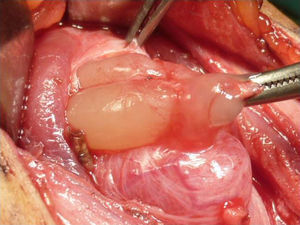
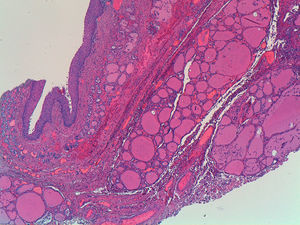
The patient underwent enucleation of the cyst (Fig. 1). The histological examination showed a nonkeratinised squamous epithelium lining with proteinaceous material inside, which confirmed the diagnosis (Fig. 2).
Solitary thyroid nodules affect 1–2% of children, but the risk of malignancy is greater in children than in adults, especially for cysts larger than 1cm. At present, this risk is estimated at 14–40% depending on the case series.1
Intrathyroid thyroglossal cysts are extremely rare; 5 cases have been described in children,2 as well as 4 asymptomatic cases in adults and 1 case in an adult that was symptomatic due to compression of adjacent structures.3,4
Traditionally, the diagnosis of STNs was based on thyroid function tests and I-131 scintigraphy. However, given the low sensitivity and specificity of scintigraphy, the current gold standard for imaging is ultrasonography, as it can detect the morphology of lesions 1mm in size, their relationship with adjacent structures, and their location within or out of the thyroid, and can guide the performance of FNAP. Benign patterns include cystic lesions, hyperechoic halos or peripheral calcifications. However, it is considered that cystic lesions can be malignant in 1% to 7% of cases.5,6
Intrathyroid thyroglossal cysts do not have specific characteristics; in published cases, thyroid function test results were normal, ultrasound examination showed unilocular cysts, and iodine-131 scintigraphy the presence of a cold nodule surrounded by the thyroid gland with homogeneous uptake of the tracer.
Cold nodules and nonfunctioning cysts are associated with a higher risk of malignancy in children despite the benign patterns found in the ultrasound examination of all the described cases, so given their characteristics the main goal is to rule out malignancy.
At present, FNAP is considered the gold standard to distinguish between benign and malignant cysts, with a sensitivity and a negative predictive value near 96%1; its main limitation is the differential diagnosis of follicular carcinoma and microfollicular adenoma. It is highly advisable that it be performed in lesions larger than 1cm or suspected to be neoplastic.1
In case number 2, cytology made diagnosis possible before surgery, which did not happen in case 1, in which surgical examination was undertaken in light of the scintigraphy findings and due to the lack of experience in the use of FNAP at the time of diagnosis. The finding of a squamous epithelium has been described by other authors2,3 as characteristic of these lesions.
Enucleation of the cyst is the first-line treament,2 prioritising the preservation of thyroid tissue. No recurrences have been described following this technique, although hemithyroidectomy may be an appropriate intervention for large cysts. If there is a transhyoid fistula, surgery should be performed by the Sistrunk procedure.4
In conclusion, the differential diagnosis of STNs must take into consideration intrathyroid thyroglossal cysts. We recommend performing a FNAP, as it can guide the diagnosis and allows exeresis of the lesion while preserving the thyroid parenchyma.
Please cite this article as: Álvarez Garcia N, Burgués Prades P, González Martínez-Pardo N, Simón Portero S, Fernández Atuán R. El quiste tirogloso intratiroideo en el diagnóstico diferencial del nódulo tiroideo solitario: a propósito de 2 casos. An Pediatr (Barc). 2015;82:360–361.
Previous presentation: Congreso de la Sociedad Española de Cirugía Pediátrica, May 22–23, 2014, Cádiz, Spain.