Patient safety has become a central component of quality of care. One of the best known and most widely used security tools in all work settings is the checklists.
The checklist is a tool that helps to not forget any step during the performance of a procedure, to do tasks with an established order, to control the fulfillment of a series of requirements or to collect data in a systematic way for its subsequent analysis. It is an aid to improve the efficiency of teamwork, promote communication, decrease variability, standardize care and improve patient safety.
Main barriers to implementation are reviewed: staff attitudes, hierarchies, poor design, inadequate training, duplication with other work lists, work overload, cultural barriers, lack of replication or checklist closing time.
Finally, its applications in Pediatrics are reviewed starting from the most widespread, the safety checklist of pediatric surgery, checklists in neonatal critical units, for safe delivery, for risk procedures, in pediatric intensive care and for pathology time-dependent emergent, e.g. pediatric trauma.
It is necessary to highlight the role of leadership in the implantation of a checklist in any area of Pediatrics. There must be one or more people from the team with the support of the Heads of Service and Managers who lead the training of the personnel, direct the implementation of the LV, evaluate the results, inform the rest of the team and can modify the processes depending on the problems found.
La seguridad de los pacientes se ha convertido en un componente central de la calidad asistencial. Una de las herramientas de seguridad más conocidas y extendidas en todos los ámbitos laborales son las listas de verificación (LV).
Una LV es una herramienta que ayuda a no olvidar ningún paso durante la realización de un procedimiento, hacer tareas con un orden establecido, controlar el cumplimiento de una serie de requisitos o recoger datos de forma sistemática para su posterior análisis. Es una ayuda para mejorar la eficacia del trabajo en equipo, fomentar la comunicación, disminuir la variabilidad, estandarizar la atención y mejorar la seguridad de los pacientes.
Se repasan las principales barreras para la implantación como las actitudes del personal, jerarquías, diseño deficiente, capacitación inadecuada, duplicación con otras listas de trabajo, sobrecarga de trabajo, barreras culturales, falta de replicación o tiempo de cierre de la LV.
Finalmente se revisan sus aplicaciones en la edad pediátrica partiendo desde la más extendida, la LV de seguridad de la cirugía pediátrica, el parto y periodo neonatal (LV de unidades de críticos neonatales, LV para el parto seguro), para procedimientos de riesgo, para cuidados intensivos pediátricos y para la patología emergente tiempo-dependiente, por ejemplo, el trauma pediátrico.
Es importante remarcar el papel del liderazgo en la implantación de una LV en cualquier área de trabajo de la Pediatría. Debe haber una o más personas del equipo con el apoyo de los Jefes de Servicio y Directivos que lideren la formación del personal, dirijan la implantación de la LV, evalúen los resultados, informen al resto del equipo y puedan modificar los procesos en función de los problemas encontrados.
The considerable development of diagnostic techniques, technologies and treatments that we have witnessed in recent years has contributed to a significant decrease in mortality due to illness or accidents.
On the other hand, the increasing complexity of medicine has also resulted in an increase in health care-related safety incidents and adverse events (AEs). Health care errors are now among the leading causes of morbidity and mortality in hospitalised patients.1
Patient safety has become one of the main priorities of health care policy in the United States and is an essential component of care quality. Thus, in October 2004 the World Alliance for Patient Safety was launched with the purpose of coordinating and disseminating improvements in patient safety worldwide (www.who.int/patientsafety).
In the past few years, numerous tools have been developed with the common goal of improving health care safety: patient identification, health information plans, hand hygiene, zero patient harm programmes, dose calculators, electronic prescription, daily rounds, checklists, clinical guidelines, adverse event reporting systems etc.
It is difficult to establish whether any of these tools performs better than all others in absolute terms. What is widely accepted since the development of the Swiss cheese model of safety incidents2 is that the more filters or barriers in place, the lower the probability of errors or AEs in care delivery.
One of the best known and most widespread safety measures in the workplace is the checklist. The creation of checklists dates from 1935. The United States Air Force established a list of steps that had to be verified before takeoff of the B-17 aircraft, known as “the Flying Fortress”.
Definition and characteristicsA checklist is a tool that prevents the omission of any of the steps involved in the performance of a procedure, helps carry out tasks in a pre-established order or helps collect data systematically for subsequent analysis. It is as simple and effective measure to reduce the risk of error due to distraction or excessive confidence in standard operating procedures. However, it does not help prevent errors stemming from lack of experience, lack of skill or lack of supervision.
Checklists are not a regulatory tool. A checklist is an aid meant to promote effective teamwork and communication and to reduce variability. It is used in every work setting and routinely in everyday life, from the checklist used by technicians that perform official vehicle inspections to the checklists that detail all the parts and mechanisms required to assemble a piece of furniture. In air traffic safety, checklists are used prior to takeoff to ensure that no critical step has been omitted. Checklists are also employed in industrial processes and audits to ensure compliance with established procedures and prevent errors.
In the health care community, checklists have been established as a simple and inexpensive means to deal with the increasing complexity of care delivery. Checklists differ from algorithms, clinical guidelines and management protocols, and therefore cannot be used for every situation.
Under the right circumstances, checklists are tools that can help standardise care and improve communication and patient safety. When it comes to patient safety, a systematic review of a few randomised controlled trials assessed the impact of checklists on the safety and outcomes of hospitalised patients. The review concluded that studies of high methodological quality are required to assess the effectiveness of checklists in promoting safety in hospitals to confirm the perceived benefits.3
Some of the main characteristics of checklists are:
- •
Simplicity. Simpler measures are easier to establish. Professionals must be aware of the risk of turning a checklist into a complex, protracted and difficult to use tool.
- •
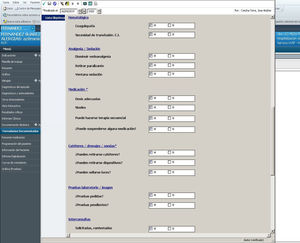
Applicability to different settings. Checklists must be adapted to the circumstances of each clinical setting. Each facility must review any given checklist to adapt it to local practices and create a sense of appropriateness, and therefore specific items may need to be modified according to differences between facilities as long as the essential safety measures are preserved. For instance, a daily goal checklist for a paediatric intensive care unit (PICU) is not valid for the paediatrics ward of the same hospital, or even for the PICU in a different hospital (Fig. 1). The generalization of checklists and a lack of applicability to the given unit or hospital inspire rejection. Each medical setting, with its particular structure, workflow and clinical needs, requires a different design and development.4
- •
A potential for measurement. Once completed, checklists serve as a record and can be reviewed at a later time to conduct comparative or quantitative studies. In the Bacteriemia Zero (zero bacteraemia) project, hospitals were given periodic feedback on the rates of primary and catheter-related bacteraemia, which also served as a motivation to improve.5
Regular auditing helps assess the progress of the intervention programme. On one hand, audits must assess the outcomes of the use of checklists and periodically monitor adherence to their use. Monitoring the use of checklists may reveal that staff members frequently do not use them as they should. Improved adherence to the use of checklists is associated with better outcomes.
Even more important is to analyse any problems associated with the use of checklists, even if they appear to be trivial. Hospital administrators need to know how checklists are being used. Solutions must be sought for any identified problems and health care professionals need to be informed. Such feedback can contribute to the success of the programme.
Structure and developmentThere is no guideline outlining the effective way to develop and design effective checklists. Some authors have proposed organising the process in 5 stages: a) conception; b) determining content and design; c) testing and validation; d) introduction, training and implementation, and e) ongoing evaluation, revision and possible retirement.4
Checklists are usually designed in the form of questions with a binary answer (YES/NO), although there may be more than 2 answer options, as long as they are close-ended (Fig. 2). The close-ended format of answers is meant to foster objectivity, although it also results in eliminating information that might be useful, as it does not allow for documentation of subtleties or singularities. The items in checklists include the critical steps in a process or issues related to patient safety (Fig. 2).
Each item in a checklist usually consists of a sentence or paragraph of text with an adjacent box for answering. Once the task is completed, the box is filled with a mark verifying completion.
It is essential that a specific individual is in charge of the verification process. Usually, boxes are checked by the nursing staff, although this can be done by any member of the care team participating in the process. This does not mean that checklists are only filled out by a single staff member. Checklists must be a participatory and involve every staff member involved in the procedure at hand. Each team must find a way to incorporate the use of the checklist as efficiently as possible, attempting to complete every step. Checklists must include a section devoted to observations to enable recording of additional information should an incident occur.
It may be useful to involve local leaders to promote this intervention in the hospital and encourage colleagues to participate. Before a checklist is introduced, some form of training workshop should be held, led by the leaders of the intervention, which helps promote team spirit. It is crucial that leaders take the time to explain how to use the checklist and its purpose. In-person workshops also allow staff from different hospitals to share experiences and perceive the project as a shared mission. In short, factors that are key to successful implementation include a committed leadership, adaptation of the checklist to local circumstances and acceptance by checklist users.
Barriers to the establishment of the use of checklistsIntroducing a new tool in clinical practice can be challenging. Some hospitals have not been able to replicate the outcomes of the use of checklists in other facilities. Several factors may affect the success or failure of a checklist, ranging from the attitudes of the staff, a poor design, deficient training, overlap with other checklists, cultural barriers or the way in which the management present the tool to staff.6 The lack of replication may also be due to the methodology employed in the initial trials and follow-up studies.
Checklists do work as long as they are implemented correctly, although this is far more complicated than having a checklist at hand. Implementation does not only involve a change in practice, but also a change in culture or organization. Checklists can be seen as yet another initiative imposed by management as opposed to an appealing novelty from which to benefit.
Some staff members will quickly adopt their use, while others will prove more reluctant. There may be resistance from health professionals, who may perceive that such tools reduce the art of medicine to an administrative chore list. In this sense, the perception of personal responsibility by each team member in regard to the checklist is crucial. Many health professionals do not regard checklists as an important tool in guaranteeing patient safety through communication and teamwork, and instead perceive them as a mere exercise in checking boxes.7 Oftentimes, they do not pay attention to the different items, read only some of them, or a member of the team is absent during verification.6
The hierarchy structure of the staff can also be an important barrier to the use of checklists. Some of the medical staff may not be comfortable with the leadership assume by the nursing staff, who are usually in charge of completing checklists. Promoting collaborative teamwork through previous training may also help overcome this barrier.
The staff may perceive checklists as an interruption to their routine workflow that results in delays, adds to the workload or is redundant with other safety measures. They may also question whether there is sufficient evidence supporting their use. On the other hand, checklists that are cluttered or poorly written promote this perception and hinder their completion. There is evidence that the use of checklists does not have a significant impact in the time of initiation of surgical procedures,8 so it is important to emphasise the importance of this “delay” in the prevention of preventable errors.
Among other reasons, health care staff that are resistant to the use of checklists have expressed that it can increase the anxiety and worry of awake patients as they hear the checklist items, especially if going through the checklist uncovers deficiencies or errors. These drawbacks can be avoided by explaining to the patient the importance of completing the checklist before the procedure as a means to prevent errors.
Completion of the “sign out” portion is the biggest barrier to correct implementation of checklists. The reason for this is the difference in wait times between different professionals. At times, the surgeon or clinician complete the procedure while the nursing staff is busy or at a time that is critical in the performance of the anaesthesiologist.8 As a result, items on the patient recovery and management after the procedure are often not discussed as a team.
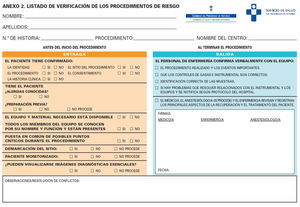
Practical applications in paediatricsSurgeryThe Safe Surgery Checklist is the most widely known checklist worldwide. The Safe Surgery Saves Lives initiative was launched by the World Alliance for Patient Safety of the World Health Organization (WHO) in 2007 to reduce mortality due to unsafe surgical care.9 The collective of surgeons, anaesthesiologists, nursing staff and patient safety experts identified 10 key safety objectives in surgical procedures: patient identification, safe anaesthesia, correct surgery at the correct site, communication with patient (informed consent) and between health care staff, antibiotic prophylaxis, antithrombotic prophylaxis, identification of specimens, prevention of retention of foreign bodies in surgical wound. This gave rise to the safe surgery checklist. The inclusion of each control measure in the checklist is based on clinical evidence or expert opinion. The aim of the checklist is to consolidate widely accepted safety practices and promote teamwork between professionals in different health care fields.
This checklist divides the operation into 3 phases: the period before induction of anaesthesia (sign in), the period after induction and before surgical incision (time out), and the period during or immediately after wound closure (sign out). In each phase, the checklist coordinator must be permitted to confirm that the team has completed its tasks before it proceeds onward.
Several studies have demonstrated that the implementation of surgical safety checklists has achieved a decrease in surgery-related mortality and complications.10,11 Studies conducted by Haynes and colleagues have demonstrated that mortality and surgical complications decreased significantly after the introduction of the checklist in a heterogeneous group of hospitals12 and that it was possible to decrease mortality even further through the voluntary and collaborative implementation of a checklist program.13
In addition to reducing morbidity and mortality in patients and documenting correct practice, the use of checklists can also increase safety for health care professionals. It is fair to assume that it will result in fewer AEs and therefore fewer filed complaints, while providing additional sources for the defence of professionals when complaints are filed.
NewbornsDue to the particular characteristic of their patients, neonatal intensive care units are settings with a high risk of AEs. The incidence of AEs in neonatal units is estimated at 20–75 events per 100 patients, and medication errors are the leading cause of AEs.14 Checklist can help detect these errors, although there is still little evidence on their use in neonatal clinical practice.
A pioneering study on the use of checklists in the neonatal intensive care setting conducted in Spain15 highlighted staff satisfaction with the introduction of checklists, particularly staff members with fewer years of experience, which may reflect the sense of security that it elicits, as well as a change in organizational culture among younger professionals. The study also found that the checklist was least effective in detecting AEs and was perceived less positively by the staff in association with its use in less complex patients (intermediate care unit), which once more highlights the need to tailor checklists to the specific needs of units and patients.
ChildbirthDue to the continued high mortality of mothers and newborns associated with childbirth worldwide, the WHO developed and promoted a Safe Childbirth Checklist as a tool to improve the quality of care given to women and newborns during labour and delivery in low-resource settings. This checklist focuses on basic care practices in institutional childbirth and addresses the main causes of maternal death, stillbirth and early neonatal death. Its usefulness has been evaluated in different countries in Africa and Asia.16
Since 2014, the WHO has sponsored a multicentre randomised controlled trial (BetterBirth) in more than 100 hospitals in India to assess whether the use of checklists improved care outcomes in women and newborns.17 The results did not meet expectations. The intervention achieved significant improvement in the quality of care of facility-based childbirth, but the improvements did not suffice to reduce neonatal and maternal mortality in comparison to the control group. Among the explanations considered for the lack of impact on mortality were gaps in the skills or resources needed for the management of complications.17
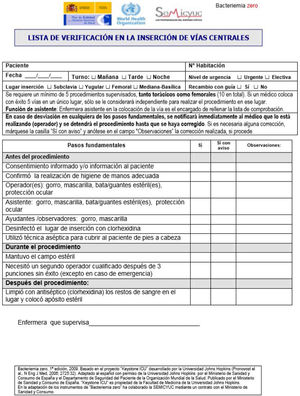
High-risk proceduresThere are several examples of procedure-specific checklists. One of the pioneers in demonstrating the potential of checklists in medical care was Peter Pronovost. In 2009, Spain, following the United States, was among the first countries to implement the Bacteriemia Zero (BZ) project through the collaboration of the Quality Agency of the Ministry of Health and Consumption of Spain and the Sociedad Española de Medicina Intensiva y Unidades Coronarias (Spanish Society of Intensive Care Medicine and Coronary Care Units), with the support of the Johns Hopkins University.5 Checklists were not new in medicine, but the work of Pronovost suggested that they could save lives.
The BZ project was important in that its aim, in addition to preventing infections associated with the use of central catheters, was to establish a safety culture in the intensive care setting. This multifactorial intervention programme included use of a daily goals sheet, appointment of leaders/coordinators among the medical and nursing staff, implementation of procedures with a known impact in reducing the incidence of bloodstream infections, use of a “central line cart”, a checklist to ensure adherence to infection control measures during catheter insertion (Fig. 3) and monthly calculation of the incidence of bacteraemia. As Gawande said, “If something so simple can transform intensive care, what else can it do?”6
In the Public Health System of the Principality of Asturias, a multidisciplinary working group designed a checklist for high-risk diagnostic and therapeutic procedures that has been used in our paediatric intensive care unit since April 2011 for all procedures requiring sedation or analgesia (Fig. 2).
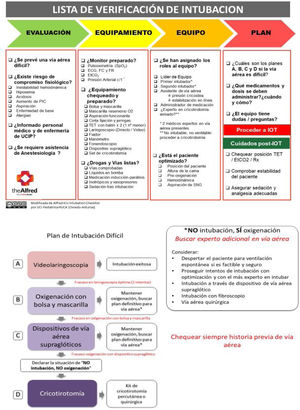
Paediatric intensive careIn the paediatric intensive care setting, checklists are used for the most common procedures, including some already mentioned in this article, such as central venous or arterial catheterization, invasive procedures requiring sedation/analgesia and endotracheal intubation.
Several intubation checklists have been published to date,18,19 but one of the best known is the Alfred ICU intubation checklist (Fig. 4). It is based to a great extent on the guidelines for intubation of adult patients published by Higgs et al.,18 to be adapted to local circumstances. This checklist is available online free of charge in the website of this Australian hospital with an express invitation to adapt and modify it as needed by the given setting. The checklist incorporates aspects of teamwork and encourages thinking that helps anticipate problems and potential solutions. The checklist ends by asking care team members whether anyone has any questions or concerns.
When it comes to clinical practice, other checklists that have been around for a long time are daily goals sheets used in the context of rounds20–22 with the aim of simplifying and standardising the management of complex patients (who are often also critically ill) in the intensive care unit.
There is evidence supporting performance of multidisciplinary rounds in the ICU setting. Such rounds should be led by an intensive care specialist,22 have explicitly defined roles for each participating provider, an established location and time and be structured by means of a checklist (daily goals sheet). The essential steps in this process are the daily goals sheet and the standardisation of the rounds.23
The daily goals sheet is perceived as improving the management of critical patients by ensuring a systematic approach and through the establishment of individualised daily goals.20–22,24 The goals of such checklists are to improve communication between ICU staff, the family and the specialists21 and to improve patient safety.
The use of checklists in daily rounds can help reduce the incidence of AEs,21–24 mortality,20 the length of stay in the ICU and in hospital20,21 and the incidence of infections related to medical devices.21 In addition, the use of checklists with a family-centred approach in hospital rounds is associated with a more favourable perception of the patient safety climate.25
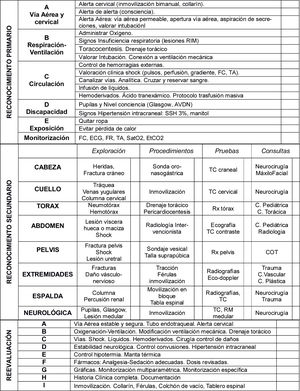
Emergency care and trauma careLastly, checklists may be of use in urgent or emergent (time-sensitive) care, such as cardiopulmonary resuscitation or paediatric trauma care (Fig. 5). There is a widespread assumption that under these circumstances the use of checklists may not be feasible, as there is hardly any time to complete them. However, it may be precisely in these situations that checklists are most necessary, as it is important to think clearly and quickly, and more errors occur due to rushing. There is evidence that use of the safe surgery checklist in urgent as well as elective surgical procedures achieves a reduction in the incidence of complications as well as mortality.10,11
Checklist for the initial management of paediatric trauma patients.25
The initial management of paediatric patients with polytrauma requires a structured and well-organised approach.26 Checklists in this context must guide initial management to prevent omissions (Fig. 4). Training on checklists and memorization of their contents may facilitate their use with the aim of taking a standardised approach to emergency situations.
To conclude, we ought to highlight the importance of leadership at the time of introducing a checklist in any paediatrics practice setting. One or more care team members, with the support of the head of the department and the administration, must lead and oversee training of the staff and the implementation of the checklist, assess outcomes, provide feedback to the rest of the care team and be able to modify processes based on the identified problems (errors).
The checklist is a seemingly trivial tool whose potential to contribute to improving processes and minimising errors belies its essential simplicity.20
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Concha-Torre A, Alonso YD, Blanco SÁ, Allende AV, Mayordomo-Colunga J, Barrio BF. Las listas de verificación: ¿una ayuda o una molestia? An Pediatr (Barc). 2020;93:135–135.