Diagnostic safety failures cause up to 15% of adverse health care-related events, many of which have serious consequences. The nature of diagnostic errors is complex and involves individual factors, such as cognitive and availability biases, as well as factors related to organizations and work dynamics. Through this document, the Health Care Quality and Patient Safety Committee of the Asociación Española de Pediatría (Spanish Association of Pediatrics) offers an updated review of the bases of diagnostic error and its characteristics in different health care settings, and proposes strategies for improving diagnostic safety and clinical reasoning, including educational and care delivery aspects and the application of novel technological resources, such as those based on artificial intelligence.
Los problemas relacionados con la seguridad diagnóstica originan hasta el 15 % de los eventos adversos ligados con la asistencia sanitaria, muchos de ellos con graves consecuencias. La naturaleza del error diagnóstico es compleja,combina factores individuales, como los sesgos cognitivos y heurísticos, así como factores vinculados a las organizaciones y a las dinámicas de trabajo. Mediante este documento, el Comité de Calidad Asistencial y Seguridad del Paciente de la Asociación Española de Pediatría ofrece una revisión actualizada de las bases del error diagnóstico, sus características en los distintos ámbitos asistenciales, y plantea estrategias de mejora en la seguridad diagnóstica y del razonamiento clínico, que incluyen aspectos educativos, asistenciales y la aplicación de recursos tecnológicos novedosos, como los basados en la inteligencia artificial.
Problems related to diagnostic safety cause up to 15% of health care-related adverse events.1,2 These events can have serious consequences for patients, families and health care professionals.
The nature of diagnostic safety problems is complex, but there are basically two types of contributing factors3: individual-level cognitive factors and systemic factors. While the practice of pediatrics is essentially an intellectual process, we, as providers, may be unaware of the mental processes that shape decision-making in our practice. This has spurred considerable interest in the analysis of both the cognitive strategies employed in clinical decision-making and the main causes of cognitive errors in care delivery. Other factors at the level of health care systems or organizations can also compromise diagnostic safety. Some examples are a workplace culture that hinders effective communication among professionals or between professionals and patients, excessive workloads or flaws in diagnostic pathways.
The aim of the Care Quality and Patient Safety Committee of the Asociación Española de Pediatría (Spanish Association of Pediatrics) in publishing this document is to offer an up-to-date review on the issue in different pediatric care settings and propose possible measures to improve diagnostic safety.
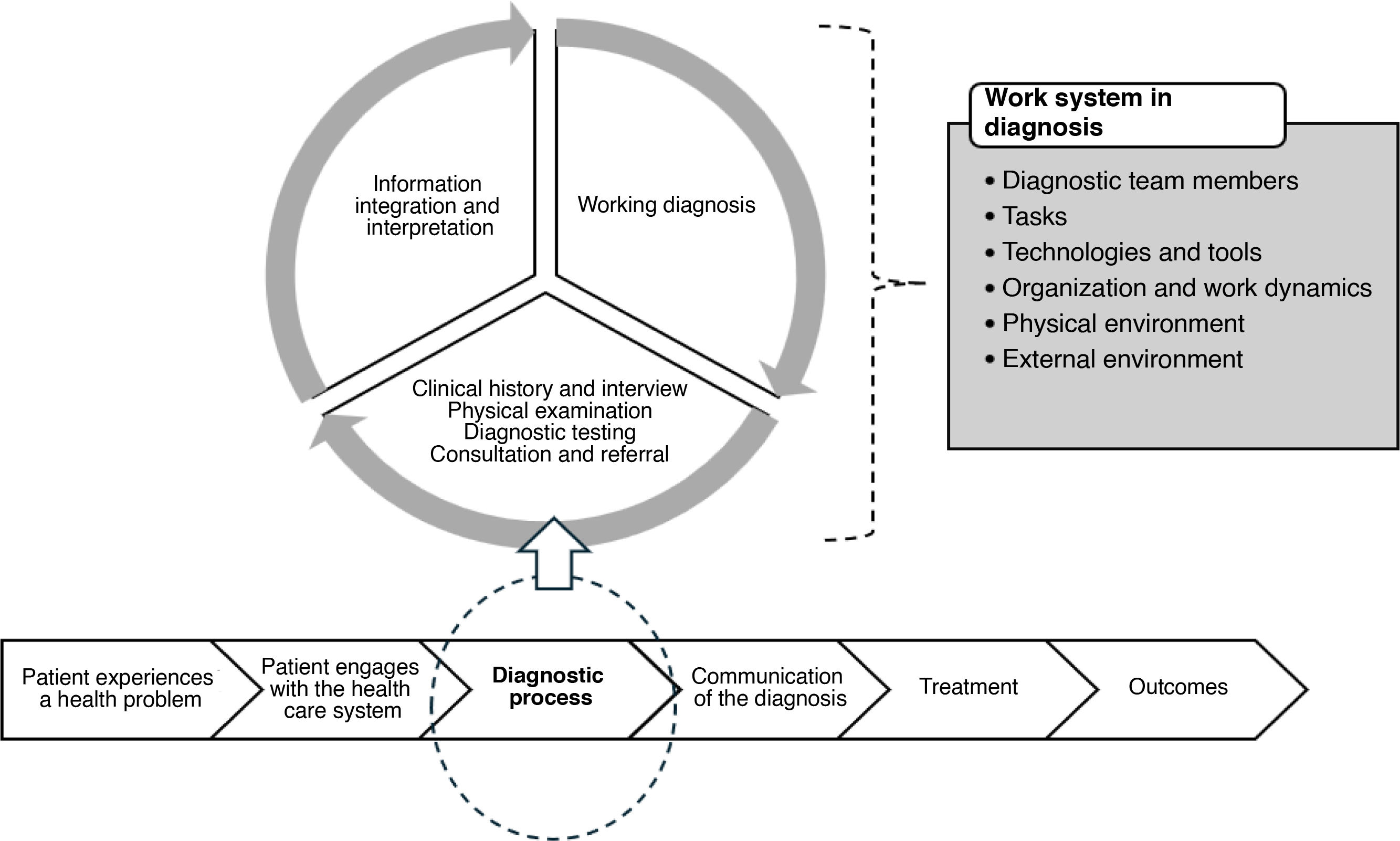
Conceptual framework of diagnostic errorsThere are two main objectives in diagnosis: to identify the disease and to rule out other possible diagnoses. This is an essential stage in care delivery, as it determines subsequent intervention and patient outcomes. Diagnosis can be a complex process depending on the context, is potentially reproducible, and the time to diagnosis can range from a few minutes to several weeks (Fig. 1).
Conceptualization of the diagnostic process. Source: Adapted from Institute of Medicine.4
Diagnostic errors encompass a diverse spectrum of medical errors that, in some cases, may be difficult to distinguish from the natural history of disease. However, there are several useful definitions and models that help identify diagnostic errors in clinical practice. The authors of the report of the National Academies of Sciences, Engineering, and Medicine of the United States defined it as the failure to establish an accurate and timely explanation of the patient’s health problem(s) or communicate that explanation to the patient.4
The scope of this definition covers wrong, delayed and missed diagnosis. The overarching concept is that of a “missed opportunity,” the fact that something could have been done differently to achieve an early and accurate diagnosis, and instead the process has resulted in unnecessary harm. In recent years, the concept of overdiagnosis has also been included in the definition, a phenomenon attributed to increased detection or widening boundaries/lowered thresholds for defining what is abnormal, so that healthy children are turned into patients.
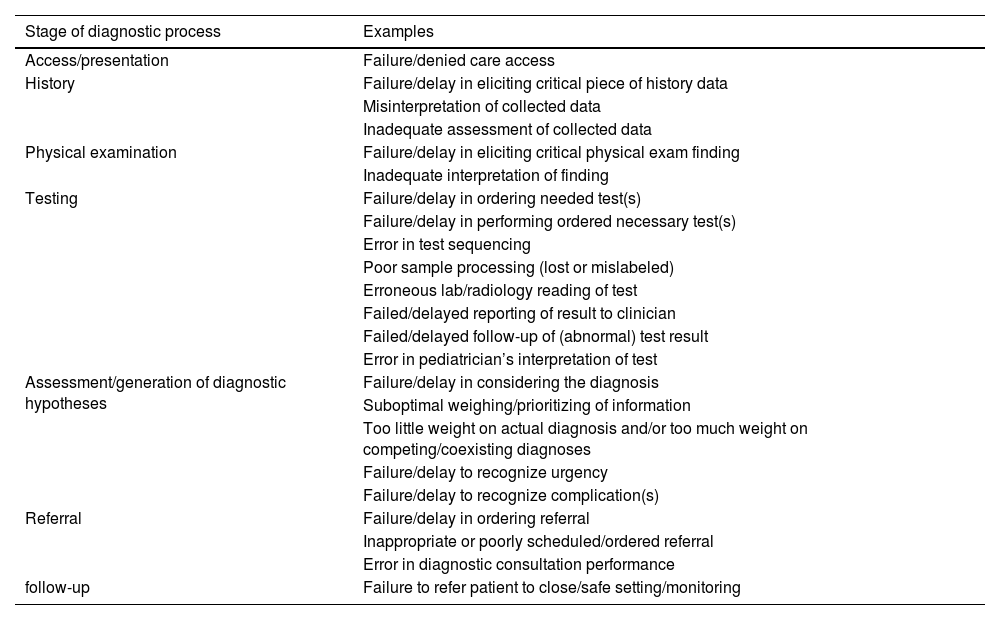
Errors can arise at any stage of the diagnostic process5 (Table 1). In every instance, the consequences can range from a harmless (near-miss incident or event), to very serious.
Examples of diagnostic errors occurring at different stages of the diagnostic process.
| Stage of diagnostic process | Examples |
|---|---|
| Access/presentation | Failure/denied care access |
| History | Failure/delay in eliciting critical piece of history data |
| Misinterpretation of collected data | |
| Inadequate assessment of collected data | |
| Physical examination | Failure/delay in eliciting critical physical exam finding |
| Inadequate interpretation of finding | |
| Testing | Failure/delay in ordering needed test(s) |
| Failure/delay in performing ordered necessary test(s) | |
| Error in test sequencing | |
| Poor sample processing (lost or mislabeled) | |
| Erroneous lab/radiology reading of test | |
| Failed/delayed reporting of result to clinician | |
| Failed/delayed follow-up of (abnormal) test result | |
| Error in pediatrician’s interpretation of test | |
| Assessment/generation of diagnostic hypotheses | Failure/delay in considering the diagnosis |
| Suboptimal weighing/prioritizing of information | |
| Too little weight on actual diagnosis and/or too much weight on competing/coexisting diagnoses | |
| Failure/delay to recognize urgency | |
| Failure/delay to recognize complication(s) | |
| Referral | Failure/delay in ordering referral |
| Inappropriate or poorly scheduled/ordered referral | |
| Error in diagnostic consultation performance | |
| follow-up | Failure to refer patient to close/safe setting/monitoring |
Diagnostic errors are a serious public health problem on account of their frequency, severity and socioeconomic impact. Although the actual incidence may vary based on the methodological approach to its calculation, it is estimated that most people will experience at least one diagnostic error in their lifetime.6 In the pediatric care setting, surveyed providers have reported making at least one error that caused harm at least once a year,7 and errors have been identified across emergency, critical, inpatient and outpatient care settings.
Multiple studies have assessed the grave consequences of diagnostic errors. In the United States, they are estimated to cause more than 80 000 deaths and serious sequelae in 200 000 patients.8 On the other hand, studies conducted in large samples of autopsies have found substantial discrepancies between clinical and postmortem diagnoses in 10% to 20% of cases, in which patient outcomes may have been better had they been managed differently.9
The Organisation for Economic Co-operation and Development10 estimates that the direct cost of unsafe care (including diagnostic errors) on to health budgets approaches 13% of healthcare spending. This includes the additional service use, legal costs and long-term costs related to affected individuals as a result of unsafe care. The actual burden of the harm resulting from diagnostic errors may be underestimated and harms and costs may be up to 20 times greater than reported.11
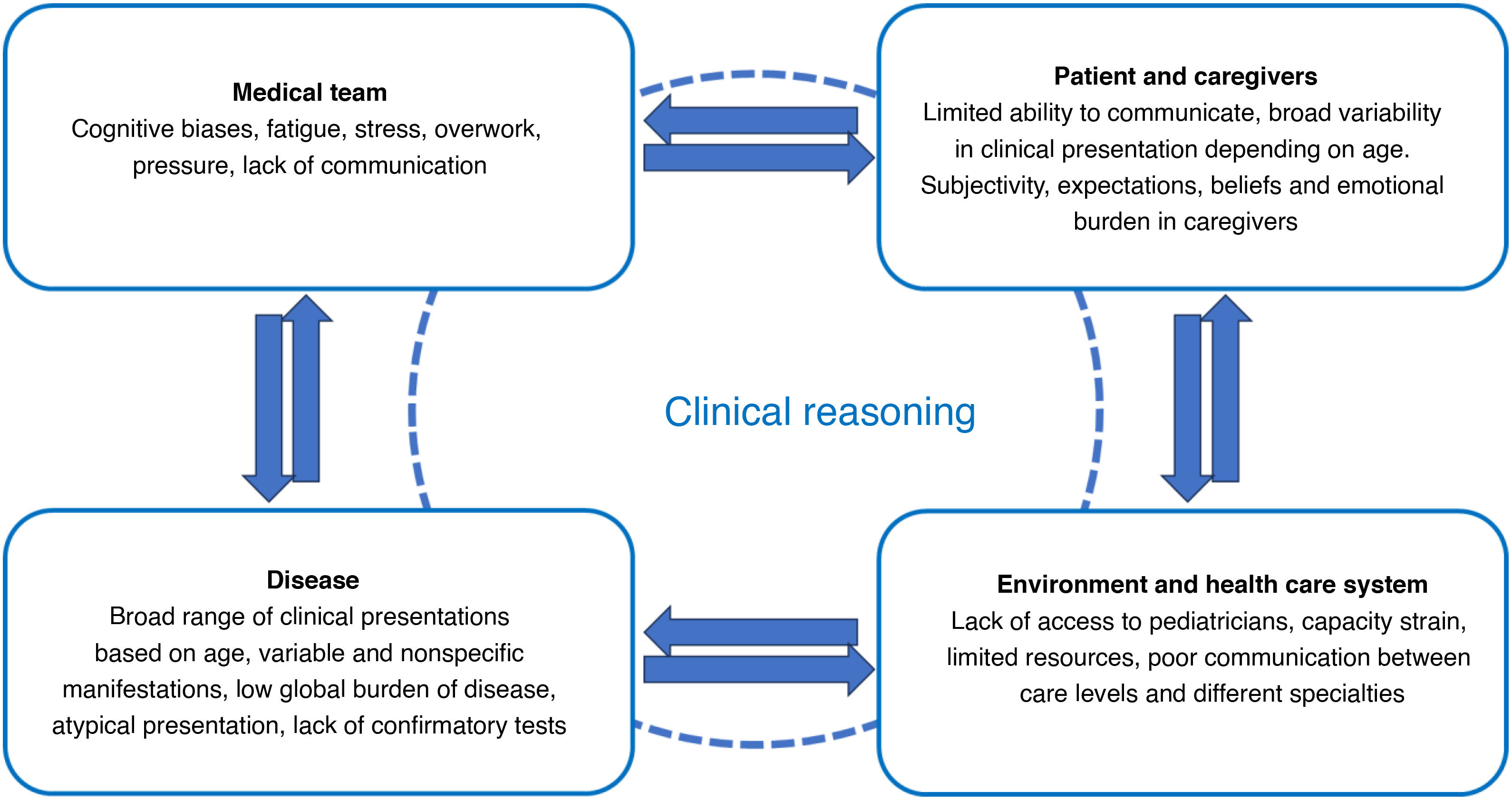
Predisposing and contributing factorsDiagnostic errors emerge from the complex interaction of pediatric patient, caregiver, disease and care team characteristics and the overall clinical context. Understanding these factors and how they interact is key in order to improve diagnostic accuracy and patient safety (Fig. 2)12:
- 1
Patient- and caregiver-related factors. Clinical manifestations vary throughout childhood and adolescence, as does the capacity of the child to communicate. The information provided by caregivers, the main proxy representatives of pediatric patients, may be affected by their mental models, expectations and beliefs, sometimes resulting in the ordering of tests and treatments that, in turn, may change the approach to management.
- 2
Disease-related factors. The epidemiology of health conditions and diseases in the pediatric population varies based on age, and even common diseases may present differently throughout the lifespan. Diseases that are rare, for which there is no confirmatory tests or with atypical presentations also pose a diagnostic challenge.
- 3
Provider-related factors. Individual physicians contribute to diagnostic errors through cognitive biases, fatigue, stress, overwork and the pressure to make quick decisions in certain circumstances. Lack of experience or training, burnout and difficulty integrating complex information can also compromise diagnostic safety.
- 4
Systemic/environmental factors. Lack of access to other specialists, capacity strain, limited resources and poor communication between levels of care play an important role in diagnostic errors.
Relationship diagram of the factors contributing to diagnostic safety problems. Source: Adapted from Merkebu et al.12
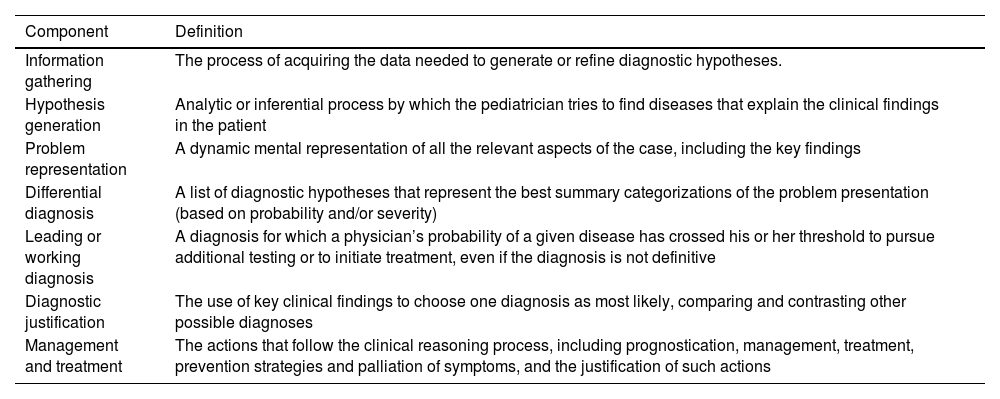
Clinical reasoning is the process wherein pediatricians analyze and interpret gathered data to explain the presenting complaint in the patient and to make decisions about appropriate confirmatory diagnosis and therapeutic interventions (Table 2).13 Despite scientific and technological advances, clinical decision-making is a process essentially based on critical thinking with a series of specific factors at play14:
- 1
The level of knowledge of the provider.
- 2
Cultural capital, nonmedical knowledge and lifetime cumulative experience.
- 3
Cognitive skills, with performance affected by emotion, physiological states or the work environment.
- 4
Metacognition: awareness and understanding of one’s own decision-making processes, motivation and cognitive skills, limitations or aptitudes for applying these components.
Components of clinical reasoning.
| Component | Definition |
|---|---|
| Information gathering | The process of acquiring the data needed to generate or refine diagnostic hypotheses. |
| Hypothesis generation | Analytic or inferential process by which the pediatrician tries to find diseases that explain the clinical findings in the patient |
| Problem representation | A dynamic mental representation of all the relevant aspects of the case, including the key findings |
| Differential diagnosis | A list of diagnostic hypotheses that represent the best summary categorizations of the problem presentation (based on probability and/or severity) |
| Leading or working diagnosis | A diagnosis for which a physician’s probability of a given disease has crossed his or her threshold to pursue additional testing or to initiate treatment, even if the diagnosis is not definitive |
| Diagnostic justification | The use of key clinical findings to choose one diagnosis as most likely, comparing and contrasting other possible diagnoses |
| Management and treatment | The actions that follow the clinical reasoning process, including prognostication, management, treatment, prevention strategies and palliation of symptoms, and the justification of such actions |
The mental processes involved in decision-making both in daily life and clinical practice15 have been classified into two broad but distinct systems or types:
- •
System 1 thinking, which is fast, automatic, and intuitive, operating with little to no effort and no sense of voluntary control. It applies inductive and associative logic to make generalizations on the basis of particular observations. It is emotion-driven and more prone to cognitive error.
- •
System 2 thinking, which is systematic, analytical and requires attention. It is less error-prone but requires effort and interruption of other activities to focus on the task at hand. It is reason-driven and applies the hypothetico-deductive approach. It is more reliable in handling complex issues and less susceptible to cognitive or emotional biases.
A combination of both systems is usually most effective in everyday clinical practice. This requires diligence and a solution-focused approach to clinical work, but also a thoughtful and analytical approach in certain situations.
Biases and heuristics as causes of diagnostic errorThe diagnostic process requires the integration of problem-solving strategies with a high level of mental flexibility, all of which is affected by the degree of uncertainty, severity and urgency of the presenting problem. Although this is a crucial stage in care delivery, in some cases the necessary critical reasoning is not carried out and decision-making is affected by biases, leading to diagnostic error.16 Among these biases are heuristics, mental rules applied all but automatically whose function is to simplify the problem through system 1 processing. They are seemingly efficient mental shortcuts that appear to effectively address complex or ambiguous situations. In some clinical scenarios, the use of heuristics is inevitable to a certain extent, as clinicians cannot possibly reflect thoroughly on every single aspect or choice in care delivery.
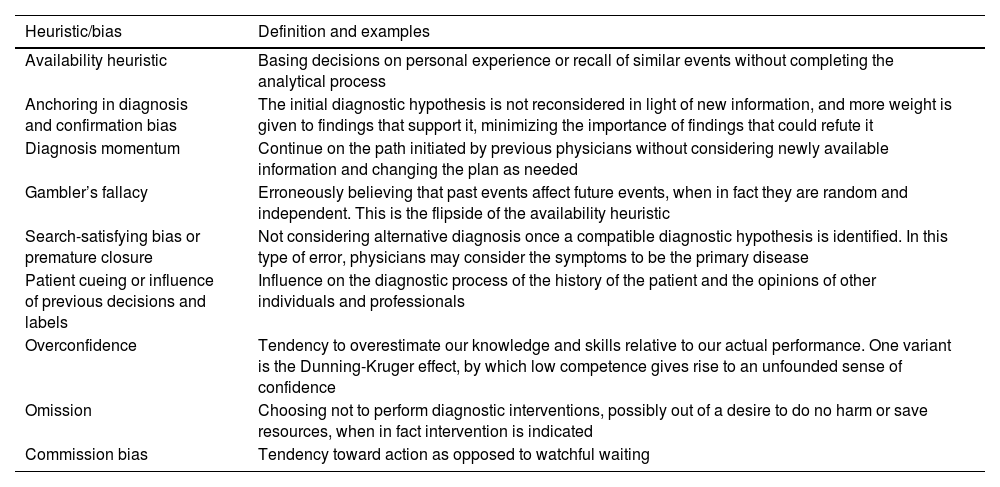
The problem is that heuristics or biases may be based on premises that are inaccurate or not rigorous (approximations, clinical rules), leading to diagnostic error through mistaken conclusions. More than 170 cognitive biases have been identified, and at least 30 have been reported in the literature as causing errors in medical decision-making.17Table 3 presents some of the most common biases.
Lists of biases and heuristics that are common causes of diagnostic errors.
| Heuristic/bias | Definition and examples |
|---|---|
| Availability heuristic | Basing decisions on personal experience or recall of similar events without completing the analytical process |
| Anchoring in diagnosis and confirmation bias | The initial diagnostic hypothesis is not reconsidered in light of new information, and more weight is given to findings that support it, minimizing the importance of findings that could refute it |
| Diagnosis momentum | Continue on the path initiated by previous physicians without considering newly available information and changing the plan as needed |
| Gambler’s fallacy | Erroneously believing that past events affect future events, when in fact they are random and independent. This is the flipside of the availability heuristic |
| Search-satisfying bias or premature closure | Not considering alternative diagnosis once a compatible diagnostic hypothesis is identified. In this type of error, physicians may consider the symptoms to be the primary disease |
| Patient cueing or influence of previous decisions and labels | Influence on the diagnostic process of the history of the patient and the opinions of other individuals and professionals |
| Overconfidence | Tendency to overestimate our knowledge and skills relative to our actual performance. One variant is the Dunning-Kruger effect, by which low competence gives rise to an unfounded sense of confidence |
| Omission | Choosing not to perform diagnostic interventions, possibly out of a desire to do no harm or save resources, when in fact intervention is indicated |
| Commission bias | Tendency toward action as opposed to watchful waiting |
In everyday practice, in addition to cognitive biases, there may also be errors that are driven by emotion, such as those resulting from conflict in the relationship between the physician and the patient or caregivers, environmental conditions, fatigue, emotional stress and changes in mood in providers.18,19
Diagnostic safety problems related to the health care system and specific care settingsAlthough different care settings share common challenges in diagnostic safety, each of them has intrinsic factors that play a role in diagnostic error.
At the primary care level, diagnostic errors are frequent and usually not immediately harmful, but may eventually have a relevant impact.20 The lack of robust patient safety infrastructures and the limited access to specialists exacerbate this problem. Furthermore, communication gaps between primary care and hospital settings are a significant source of error.21
In pediatric emergency departments, decision-making is compromised by heavy workloads, frequent interruptions and adverse environmental conditions. Pediatricians often have to work with incomplete information due to lack of access to health care records, which increases the probability of errors.
In inpatient care settings, the lack of effective communication during patient transfers and the limited integration of health care records have been identified as relevant sources of error.22 The poor implementation of early warning systems increases the risk of late or ineffective recognition of patient deterioration, resulting in unplanned transfer to the intensive care unit and poorer subsequent outcomes.23
In critical care, medical complexity and urgency frequently increase the probability of diagnostic errors. Diagnostic uncertainty at admission and atypical presentation at admission have also been found to be associated with diagnostic errors.24
In addition to posing a threat to diagnostic safety in themselves, many of these system-related factors facilitate the occurrence of errors stemming from provider-related factors or hinder their detection.
Clinical uncertainty and overdiagnosisMost pediatricians face situations of diagnostic uncertainty in the various settings where they practice. To manage this uncertainty, they need to come to terms with the limitations of medical knowledge and their personal limitations and be aware of the potential iatrogenic effects of diagnostic procedures. Clinical reasoning and medical judgment must be used to weigh the risks of any intervention against the expected benefits for the patient. Quaternary prevention25 is a recent concept encompassing the measures that can be taken to prevent, reduce or palliate the harm caused by unnecessary health care interventions.
The concept of overdiagnosis as an undesirable effect of medical practice has emerged in recent years. Overdetection of borderline values or indeterminate findings that rarely affect the course of the disease but result in further testing is increasingly common. Variants of normal, which are common in children or adolescents, or life circumstances, such as grief secondary to a loss or insomnia resulting from poor sleep habits, are medicalized. In other instances, the thresholds applied to classify an individual as having a disorder are lowered (eg, age threshold for attention-deficit hyperactivity disorder)26 or results of screening in healthy individuals that require diagnostic confirmation are taken as a definitive diagnosis.
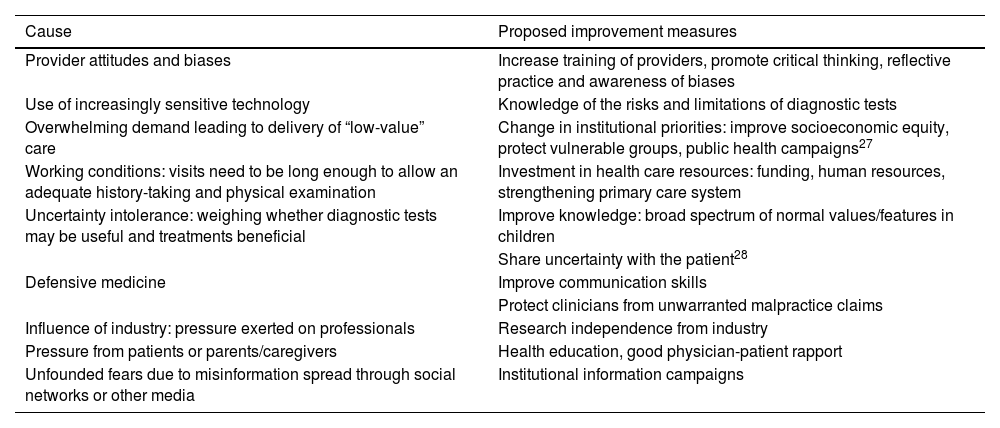
Overdiagnosis has several deleterious consequences for patients, families and health care systems. Diagnostic tests themselves can have negative consequences, such as exposure to radiation, the risks associated with sedation, procedural pain or the need to fast before the test is performed. In addition, children and adolescents may end up receiving unnecessary treatments and being labelled as “diseased until proven otherwise” has a negative impact on their emotional development and in their family and social lives. Lastly, overdiagnosis results in substantial consumption of health care resources, with an opportunity cost to the detriment of other health care interventions that are needed in the population. Table 4 presents some causes of overdiagnosis and proposed measures for improvement.
Causes of overdiagnosis in clinical practice and possible improvement measures.
| Cause | Proposed improvement measures |
|---|---|
| Provider attitudes and biases | Increase training of providers, promote critical thinking, reflective practice and awareness of biases |
| Use of increasingly sensitive technology | Knowledge of the risks and limitations of diagnostic tests |
| Overwhelming demand leading to delivery of “low-value” care | Change in institutional priorities: improve socioeconomic equity, protect vulnerable groups, public health campaigns27 |
| Working conditions: visits need to be long enough to allow an adequate history-taking and physical examination | Investment in health care resources: funding, human resources, strengthening primary care system |
| Uncertainty intolerance: weighing whether diagnostic tests may be useful and treatments beneficial | Improve knowledge: broad spectrum of normal values/features in children |
| Share uncertainty with the patient28 | |
| Defensive medicine | Improve communication skills |
| Protect clinicians from unwarranted malpractice claims | |
| Influence of industry: pressure exerted on professionals | Research independence from industry |
| Pressure from patients or parents/caregivers | Health education, good physician-patient rapport |
| Unfounded fears due to misinformation spread through social networks or other media | Institutional information campaigns |
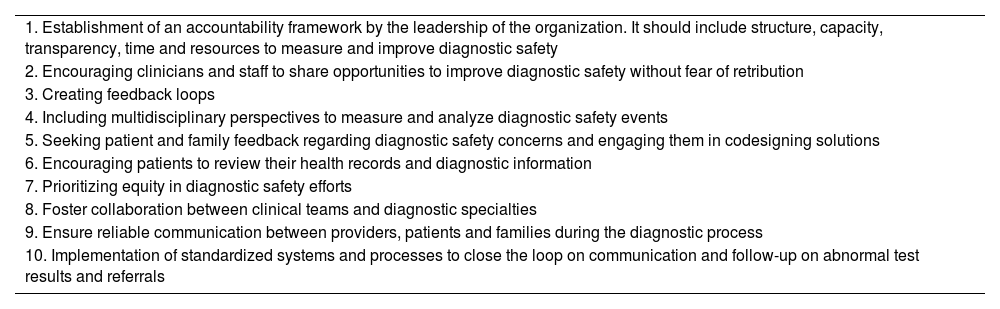
The complex nature of diagnostic errors can make their correct identification, quantification and analysis difficult. Strategies to address diagnostic errors must include interventions targeting both providers and organizations. Comprehensive quality improvement initiatives have been developed to this end, combining systems to optimize detection and retrospective measurement with interventions to promote transparency regarding disclosure and discussion of errors, provision of feedback to clinicians and education on the diagnostic process.29
One possible improvement consists in the implementation of checklists, which are intended to encourage additional reflection on the initial diagnostic impression.30 There are clinical prediction rules and decision support tools to aid the differential diagnosis of specific diseases, general checklists to guarantee the basic steps in clinical reasoning31 as well as safer diagnostic checklists developed by institutions32 (Table 5).
Ten priorities for diagnostic excellence in health care organizations.
| 1. Establishment of an accountability framework by the leadership of the organization. It should include structure, capacity, transparency, time and resources to measure and improve diagnostic safety |
| 2. Encouraging clinicians and staff to share opportunities to improve diagnostic safety without fear of retribution |
| 3. Creating feedback loops |
| 4. Including multidisciplinary perspectives to measure and analyze diagnostic safety events |
| 5. Seeking patient and family feedback regarding diagnostic safety concerns and engaging them in codesigning solutions |
| 6. Encouraging patients to review their health records and diagnostic information |
| 7. Prioritizing equity in diagnostic safety efforts |
| 8. Foster collaboration between clinical teams and diagnostic specialties |
| 9. Ensure reliable communication between providers, patients and families during the diagnostic process |
| 10. Implementation of standardized systems and processes to close the loop on communication and follow-up on abnormal test results and referrals |
Improving metacognition, that is, the ability to reflect on one’s own thought processes, is a key strategy to reduce cognitive bias. Improving metacognition, that is, the capacity to reflect on one’s own thought processes, is a key strategy in reducing cognitive bias. Relational reasoning strategies have been developed (analogy, anomaly, antinomy and antithesis) to help identify significant patterns within any stream of information to supplement the clinical reasoning process of providers.33 One widely accepted recommendation is the reflective practice of taking what is known as a “diagnostic timeout”.34 This process, which basically consists in seeking alternatives to one’s conscious opinion (“what else could the patient have?”) reduces many of the biases associated with heuristics.
Training of new pediatricians in diagnostic excellence and development of clinical reasoningClinical reasoning is considered a core competency for the practice of medicine. It is essential for all aspects of clinical practice, including diagnostic accuracy and how to handle complexity and uncertainty.35 In spite of its importance, there are significant inconsistencies and gaps in the approach to teaching clinical reasoning in the curricula of both medical schools and specialty or residency training programs, especially if it is based solely in experience, without a reflective approach.
As is also the case in clinical practice, learning clinical reasoning requires a balance between inductive and deductive strategies,36 on which systems 1 and 2 of thinking are based. Future pediatricians need to learn reliable clinical patterns to be able to categorize the manifestations of common diseases and warning signs. They also need to be trained in the hypothetico-deductive method, critical thinking and the recognition of the most common cognitive biases in clinical practice.
For training to be successful, the following characteristics must converge: the establishment of activities with defined objectives, constant and immediate feedback and the opportunity to repeat activities until they are perfected, with a key element shared by all that is individual motivation.37
Some of the educational strategies that can be used to promote the acquisition of clinical reasoning skills are38: exposure to a wide variety of clinical cases, activation of prior knowledge, recognition of disease patterns, formulation of expert strategies to reach a diagnosis, making residents formulate differential diagnoses, and encouraging reflection, metacognition and deliberate practice and providing instructive feedback. Clinical reasoning skills should be assessed throughout the medical training process in a variety of settings, including the deliberative method. These skills can be trained in real-world work settings and through simulation.
Inclusion of novel complementary tools. Artificial intelligenceCurrently, the integration of new technologies, such as artificial intelligence (AI), is significantly improving the accuracy and efficiency of all processes, in general and in health care in particular. Artificial intelligence-based tools,39 such as machine learning and image processing algorithms, have an enormous potential to improve accuracy and efficiency in clinical practice.
Artificial intelligence can serve as a complementary tool in medical diagnosis, helping health care professionals identify complex patterns in large volumes of clinical data and images. In addition, AI can speed up diagnosis times, which is crucial in emergencies and for patients with rare diseases, particularly pediatric ones.40
While it has its advantages, the inclusion of AI in diagnostic processes also poses challenges and risks that must be carefully evaluated. Artificial intelligence-based systems depend on quality data, and any errors in the data can lead to incorrect diagnoses. In addition, the interpretation of AI results still requires supervision by trained professionals. There is also concern about excessive reliance on machines and the potential dehumanization of health care delivery, especially in the treatment of complex diseases that require a comprehensive evaluation and a personalized approach to management.
Although AI promises great advances in diagnostic safety, it must be integrated with caution, ensuring that technology complements human knowledge to produce the best results for the patient. It is essential that more research be conducted (studies on different AI models, their performance, usefulness, ethics, etc) before AI models are implemented in clinical practice.
ConclusionThe complex nature of diagnostic errors calls for a combination of individual and collective improvement measures. Clinical reasoning must remain a cornerstone of pediatrics training and care delivery, but threats and barriers to diagnostic safety must also be reduced across care settings. Last of all, tools such as checklists and novel resources, like those based on artificial intelligence, should be integrated in clinical practice to improve diagnostic accuracy.