The aim of this project was to evaluate the psychopathological impact of home confinement and school closing between March and September 2020 on the mental health of Catalonian children.
MethodsPEDSAME study: first cross-sectional section (beginning of the school year) and retrospective data (lockdown), carried out through the network of Primary Care pediatricians in the Catalan population between 5 and 14 years (included) from 09/14/2020 to 10/30/2020 in a random sample. Data were collected with an online survey through the RedCap platform at the beginning of the school year. The main variable was the result of the Strengths and Difficulties Questionnaire answered by parents to assess the risk of psychopathology, in addition to other related variable.
ResultsThe results obtained at the beginning of the school year show that 9.8% of the patients were probable cases of psychopathology. The most affected group were those between 5 and 8 years. The perception of the children's level of concern for their health and that of their family was a risk factor for presenting psychopathology, while the good family environment was a protective factor. Emotional and behavioral symptoms, sleep disorders and problematic use of screens were detected more frequently during confinement than at the beginning of the school year.
ConclusionsConfinement and the absence of schooling for 6 months had a negative impact on the mental health of the child–adolescent population who showed worse indicators than the previous year.
El objetivo de este proyecto fue evaluar el impacto psicopatológico del confinamiento domiciliario y cierre escolar entre marzo y septiembre 2020 en la población pediátrica catalana.
MétodosEstudio PEDSAME: primer corte transversal (inicio de curso escolar) y datos retrospectivos (periodo de confinamiento), realizado a través de la red de pediatras de atención primaria en población catalana entre 5 y 14 años (incluidos) del 14/09/2020 al 30/10/2020 en una muestra aleatoria. Los datos fueron recogidos con una encuesta on line a través de la plataforma RedCap al inicio del curso. La variable principal fue el resultado del cuestionario Strengths and Difficulties Questionnaire contestado por los progenitores para evaluar el riesgo de psicopatología, además de otras variables relacionadas.
ResultadosLos resultados obtenidos al inicio del curso escolar mostraron que el 9,8% de los pacientes eran casos probables de psicopatología. La franja más afectada fue la de los 5 a 8 años. La percepción del nivel de preocupación de los niños por su salud y la de su familia fue un factor de riesgo de presentar psicopatología, mientras que el buen ambiente familiar resultó protector. Durante el confinamiento se detectaron con mayor frecuencia síntomas emocionales, de conducta, trastornos del sueño y uso problemático de pantallas respecto al inicio del curso escolar.
ConclusionesEl confinamiento y la ausencia de escolarización durante 6 meses supusieron un impacto negativo en la salud mental de la población infantojuvenil, con peores indicadores que el curso anterior.
Coronavirus disease 2019 (COVID-19) has given rise to an unprecedented pandemic, as no infectious disease had ever affected these many countries or this large a population. In Spain, as in many other countries, it has motivated the imposition of significant social isolation measures, such as lockdowns and school closures.1
In previous epidemics considered public health emergencies, evidence emerged of their deleterious effect on mental health.2–5 The scientific literature has described anxiety, depression, sleep disorders, post-traumatic stress disorder, addictive behaviours and eating disorders,6 as well as hallucinations and psychotic episodes.7
Several studies have confirmed the negative psychological impact of the COVID-19 pandemic, the lockdown and other measures used to contain it on the mental health of the population.7 The earliest evidence was published by Wang et al.,8 who reported a moderate to severe impact on mental health in 54% of individuals. In the paediatric population, early evidence from China described high levels of anxiety in children and adolescents of both sexes (which we will refer to from hereon as “children”) and depression symptoms in more than 22.9,10 In Germany, Ravens-Siebere et al11 found a higher incidence of mental health disorders in comparison with past records: 17.8% versus 9.9%, as well as higher levels of anxiety. The impact was hardest on children in low-income households, immigrants and individuals living in cramped spaces.
In Spain, several studies in adults reported a moderate to severe psychological impact on 24.7% of individuals, with deterioration of mental health in nearly 50%12,13 and a higher incidence of stress, anxiety and depression in the young.13 Lavigne-Cerván et al14 found a higher incidence of anxiety at ages 9–12 years and more sleep disturbances at ages 13–18 years. Orgiles et al15 described a substantial impact on the lives of Italian and Spanish youth, and many parents reported changes in mood and behaviour in their children. In Catalonia, the authors of the EmCoVID-19 found a significant increase in emotional symptoms and behavioural problems in children and adolescents.16 In vulnerable families, the incidence of mental health symptoms has been even higher; according to Save the Children,17 stress levels and household conflict had increased in 4 out of 10 disadvantaged households in association with cramped and poor living conditions.
Few studies have analysed the impact on mental health in children. The aim of our study was to assess the psychological impact of home confinement and school closures between March and September 2020 in the paediatric population of Catalonia.
Material and methodsStudy design and settingWe conducted a longitudinal, observational study (PEDSAME study) in a single cohort of children aged 5–14 years (both included) in Catalonia from 14/09/2020 to 30/10/2020, obtaining a random sample through the regional primary care paediatrician network. This article presents the analysis of the data for the first 2 time points of the study: the first time point, with retrospective collection of data corresponding to the lockdown, and the second time point, with collection of current data at the beginning of the school year.
The PEDSAME study is an ongoing project conducted through the network of primary care paediatricians (XaRePAP) of the Section on Primary Care of the Societat Catalana de Pediatría (Catalonian Society of Paediatrics), whose members are primary care paediatricians and paediatric nurses with representation of the 4 provinces of Catalonia and rural, suburban and urban settings.
Study periodFrom September 14 to October 30, 2020.
Population under studyWe analysed a random sample of children recruited from the caseloads of the primary care paediatricians, members of the XaRePAP network. The inclusion criteria were: age 5–14 years (both included) that resided in Catalonia during the study period. The exclusion criteria were lack of signed informed consent, presence of a language barrier impeding communication or inability to contact the participant through the phone.
SampleWe estimated the sample size required to detect mental health disorders, with an expected prevalence in the population of 7.5% (833 000, source: IDESCAT),18 a precision of 3% and a 95% level of confidence, and found that we needed a minimum of 297 participants.
Data collectionWe sent a broad sample of random numbers to the 35 participating paediatricians, which they used to select 15 patients from a numbered list of patients in their caseloads.
We reached out to the legal guardians of selected patients by telephone to inform them about the study and asking them to participate. If they accepted, we sent a link through the RedCap platform (Research Electronic Data Capture, Vanderbilt University)19,20 to download the study information sheet, fill out the consent form and complete the online questionnaire, from which we obtained the self-reported data provided by the primary caregivers. We used the same questionnaire to collect data for the lockdown period and for the beginning of the school year.
We provided paper copies of the questionnaire to families that did not have internet access.
This article presents the results corresponding to the data obtained in the initial time point, at the start of the school year. They are cross-sectional data collected in October 2020 on the mental health condition of children at the start of the school year, along with retrospective data collected to assess mental health during the lockdown (March-May 2020).
Study variablesThe primary outcome was the score obtained in the Strengths and Difficulties Questionnaire (SDQ).21,22
We analysed individual, family, clinical and mental health variables in relation to COVID-19 during the lockdown. We also collected data regarding online schooling, pre-existing medical and psychiatric conditions or learning disorders diagnosed before the pandemic, treatments, chronic diseases, and emotional and behavioural manifestations, worry, screen use and physical activity during the lockdown and at the beginning of the school year.
The SDQ21 is a brief instrument to screen for mental disorders in children and adolescents. It assesses emotional symptoms and conduct problems in individuals aged 5–17 years. It consists of 25 items structured in 5 dimensions: emotional symptoms, conduct problems, peer problems, hyperactivity and prosocial behaviour. There are 3 answer choices for each item, not true, somewhat true and certainly true, which are assigned 0, 1 and 2 points, respectively. The questionnaire is completed by primary caregivers. We stratified the scores to define the risk of the presence of a mental health disorder as follows: normal range (0–13 points), possible disorder (14–16 points) and probable disorder (17–40 points). The Spanish version of the SDQ has proven to have discriminatory power, with an optimal cut-off score for diagnosis of 20 points in the total difficulties score that offers the highest sensitivity (0.96) and specificity (0.95) according to Fajardo et al23; reference values for the parent version of the SDQ have been calculated and are available for use in Spain.24 The PEDSAME study uses the Spanish version of the SDQ, available for download at no cost at www.sdqinfo.com. We used the same reference ranges used by the Department of Health of Catalonia to allow comparison of results, so we maintained the cut-off score of 17 to define probable disorder, as specified in the aforementioned website. Español-Martín et al21 analysed whether the Spanish version is a valid tool to screen for emotional and behavioural problems applying these ranges. They found that the Spanish version is valid to screen for emotional and behavioural problems applying the cut-off score of 17 points.21
Ethical considerationsThe study adhered to best practice protocols for biomedical research. The PEDSAME was approved by the Ethics Committee of the Institut Universitari d’Investigació en Atenció Primària Jordi Gol, file no. 20/142-PVC, on July 17, 2020.
Statistical analysisWe performed a descriptive analysis of the sample. We summarised quantitative data as mean values and used the t test to make comparisons. In the case of categorical variables, we calculated percentages for each category and made comparisons by means of the chi square test. Statistical significance was defined as a p-value of less than 0.05.
We compared the data obtained in October to the data obtained during the lockdown. We assessed differences between both periods in the main emotional symptoms and did the analysis by age group.
We calculated the total scores of the SDQ in October 2020 and performed a multivariate analysis by means of binary logistic regression to identify the factors associated with SDQ scores indicative of mental health disorders.
The statistical analysis was performed with the software SPSS version 25 (SPSS Inc, Chicago, IL, USA).
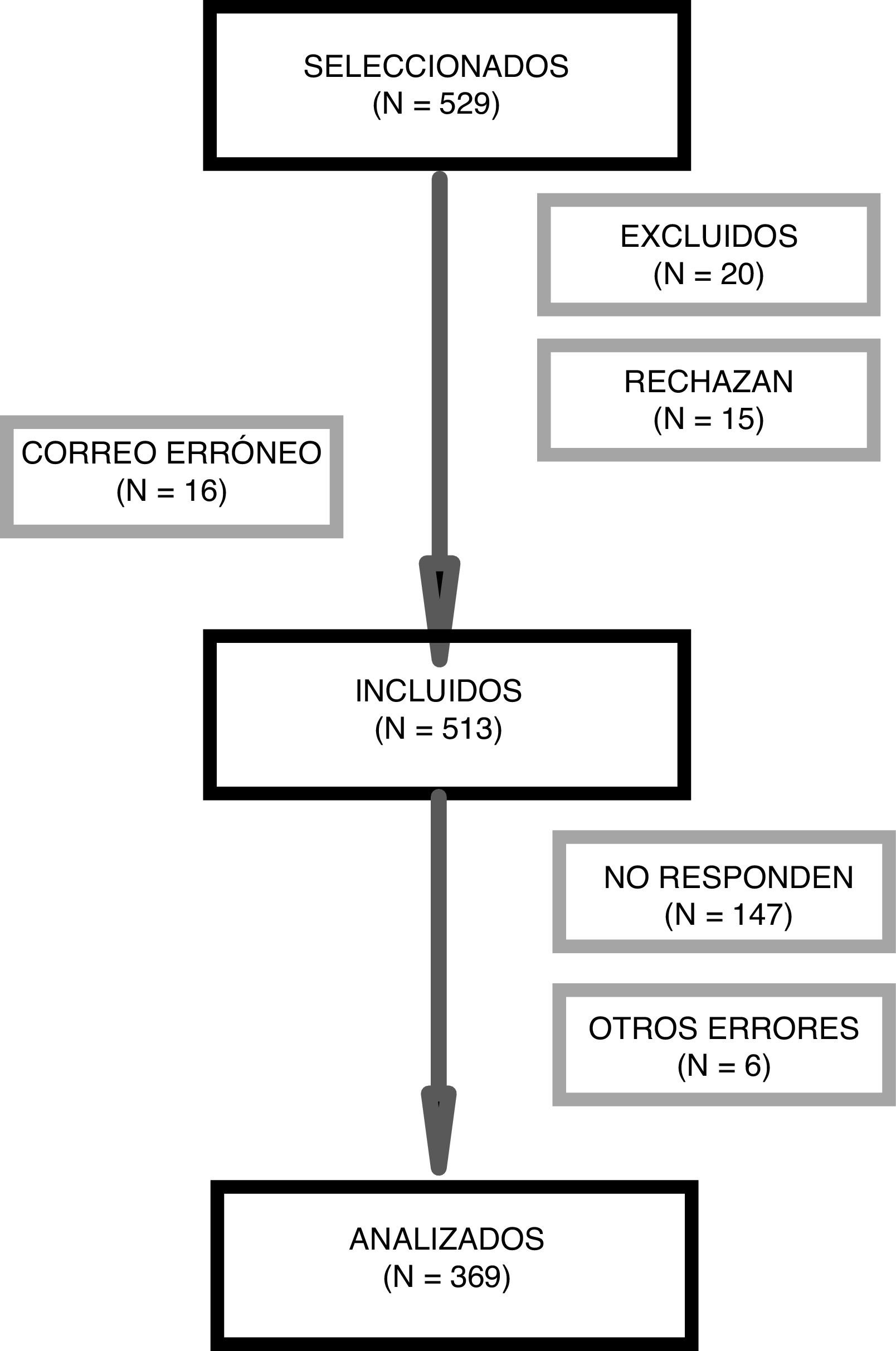
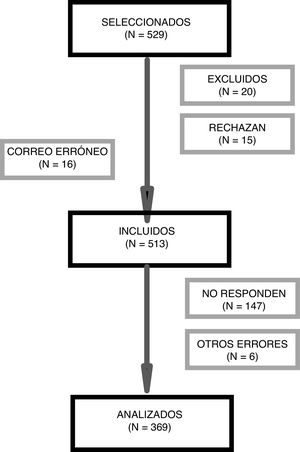
ResultsWe invited 529 children to participate, and the final analysis included 369 of them (Fig. 1).
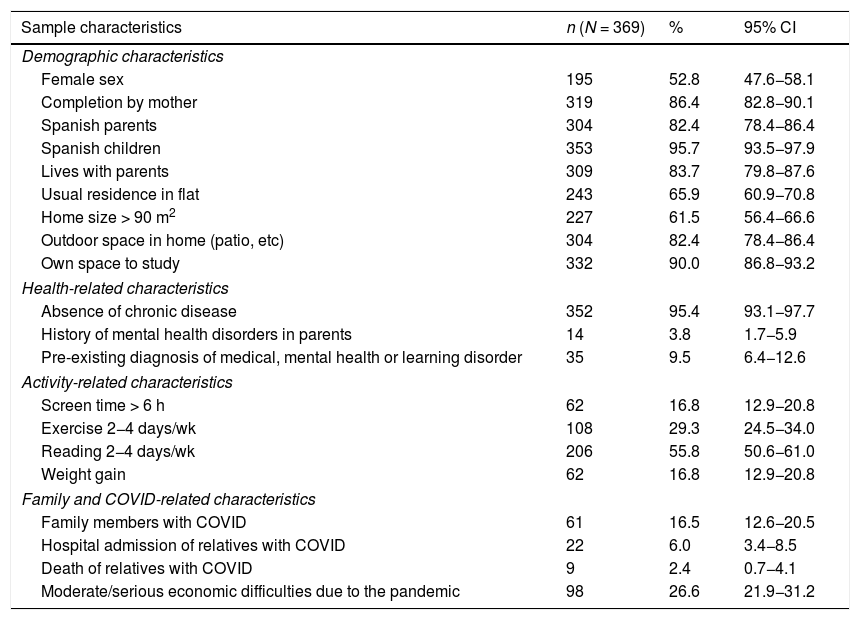
Descriptive analysis of the sampleTable 1 presents the general characteristics of the sample and the frequency of COVID-19 in the household. We ought to highlight that 9.4% had a previous diagnosis of mental health or learning disorders.
General characteristics of the sample.
| Sample characteristics | n (N = 369) | % | 95% CI |
|---|---|---|---|
| Demographic characteristics | |||
| Female sex | 195 | 52.8 | 47.6−58.1 |
| Completion by mother | 319 | 86.4 | 82.8−90.1 |
| Spanish parents | 304 | 82.4 | 78.4−86.4 |
| Spanish children | 353 | 95.7 | 93.5−97.9 |
| Lives with parents | 309 | 83.7 | 79.8−87.6 |
| Usual residence in flat | 243 | 65.9 | 60.9−70.8 |
| Home size > 90 m2 | 227 | 61.5 | 56.4−66.6 |
| Outdoor space in home (patio, etc) | 304 | 82.4 | 78.4−86.4 |
| Own space to study | 332 | 90.0 | 86.8−93.2 |
| Health-related characteristics | |||
| Absence of chronic disease | 352 | 95.4 | 93.1−97.7 |
| History of mental health disorders in parents | 14 | 3.8 | 1.7−5.9 |
| Pre-existing diagnosis of medical, mental health or learning disorder | 35 | 9.5 | 6.4−12.6 |
| Activity-related characteristics | |||
| Screen time > 6 h | 62 | 16.8 | 12.9−20.8 |
| Exercise 2−4 days/wk | 108 | 29.3 | 24.5−34.0 |
| Reading 2−4 days/wk | 206 | 55.8 | 50.6−61.0 |
| Weight gain | 62 | 16.8 | 12.9−20.8 |
| Family and COVID-related characteristics | |||
| Family members with COVID | 61 | 16.5 | 12.6−20.5 |
| Hospital admission of relatives with COVID | 22 | 6.0 | 3.4−8.5 |
| Death of relatives with COVID | 9 | 2.4 | 0.7−4.1 |
| Moderate/serious economic difficulties due to the pandemic | 98 | 26.6 | 21.9−31.2 |
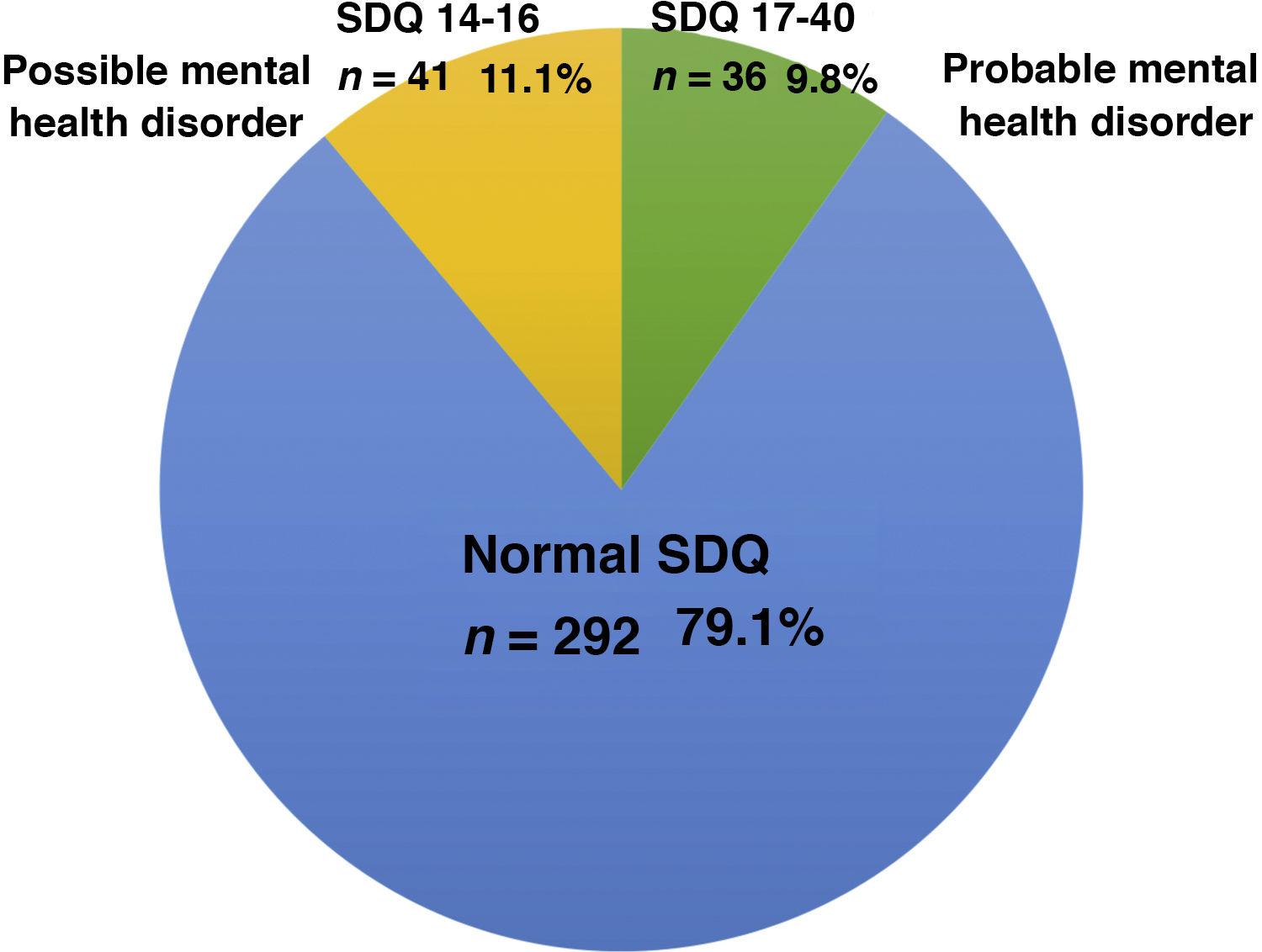
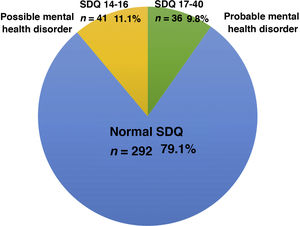
Fig. 2 presents the results of the SDQ in the first phase of an ongoing study, which corresponded to the beginning of the school year: the questionnaire found that mental health disorders were probable in 9.8% of participants (score ≥ 17), and possible in 11.1% (score, 14–16).
The proportion of participants with SDQ scores in the abnormal range was significantly higher in the group with a previous diagnosis of mental health or learning disorder (30.6%) compared to participants without this history (7.2%).
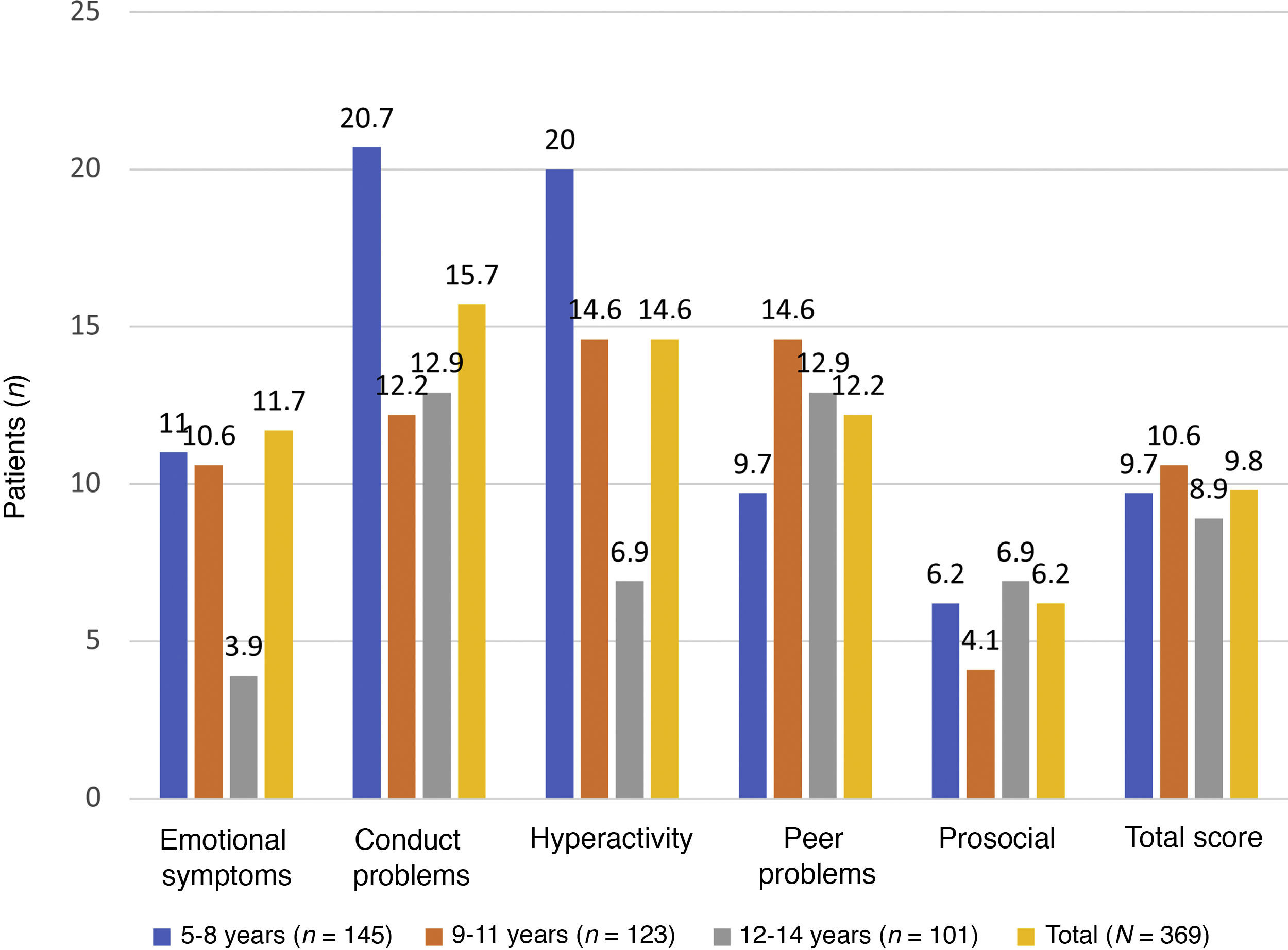
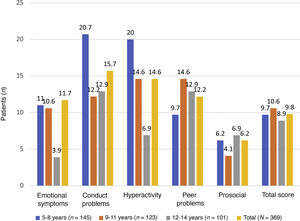
Fig. 3 illustrates that the scores in the conduct problems and hyperactivity symptoms subscales were higher in children aged 5–8 years.
Compared to the rest of the sample, participants with SDQ scores in the abnormal range had significantly less room of their own to study, were more worried about their health (as were their parents) and perceived their home life more negatively, both during the lockdown and at the beginning of the school year. Also, in both periods, participants with abnormal scores exhibited significantly more emotional symptoms and conduct problems (irritability, sadness, nervousness and aggressiveness) and greater difficulty sleeping. During the lockdown, participants in this group were also more likely to use screens excessively.
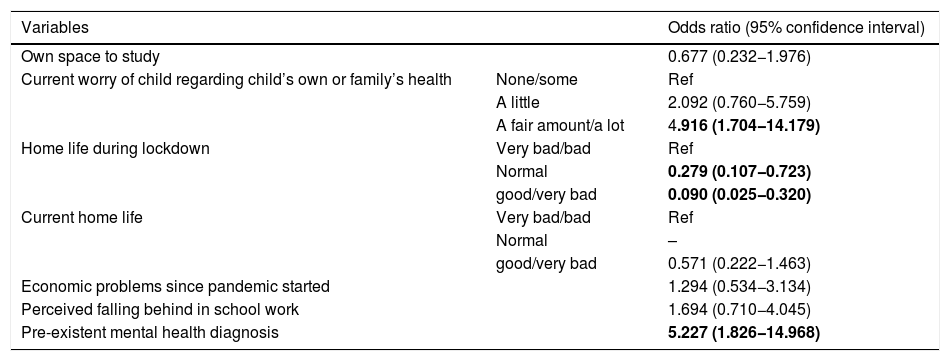
Table 2 presents the multivariate analysis of patients with a SDQ score in the abnormal range (≥17 points) compared to the rest of the sample. We fit the model by adding only those variables that could have contributed to the impairment of mental health and with significant differences between 2 groups. The variables that remained significant in the multivariate analysis were current worry of the child regarding their own or their parents’ health, and a positive perception of the home life during the lockdown and at the beginning of the school year.
Odds ratio for patients with SDQ scores in the probable mental health problem range (≥ 17) compared to the rest of the sample.
| Variables | Odds ratio (95% confidence interval) | |
|---|---|---|
| Own space to study | 0.677 (0.232−1.976) | |
| Current worry of child regarding child’s own or family’s health | None/some | Ref |
| A little | 2.092 (0.760−5.759) | |
| A fair amount/a lot | 4.916 (1.704−14.179) | |
| Home life during lockdown | Very bad/bad | Ref |
| Normal | 0.279 (0.107−0.723) | |
| good/very bad | 0.090 (0.025−0.320) | |
| Current home life | Very bad/bad | Ref |
| Normal | – | |
| good/very bad | 0.571 (0.222−1.463) | |
| Economic problems since pandemic started | 1.294 (0.534−3.134) | |
| Perceived falling behind in school work | 1.694 (0.710−4.045) | |
| Pre-existent mental health diagnosis | 5.227 (1.826−14.968) | |
Odds ratio obtained by logistic regression analysis for each individual variable adjusted for all other variables featured in the table.
Statistically significant results are presented in boldface.
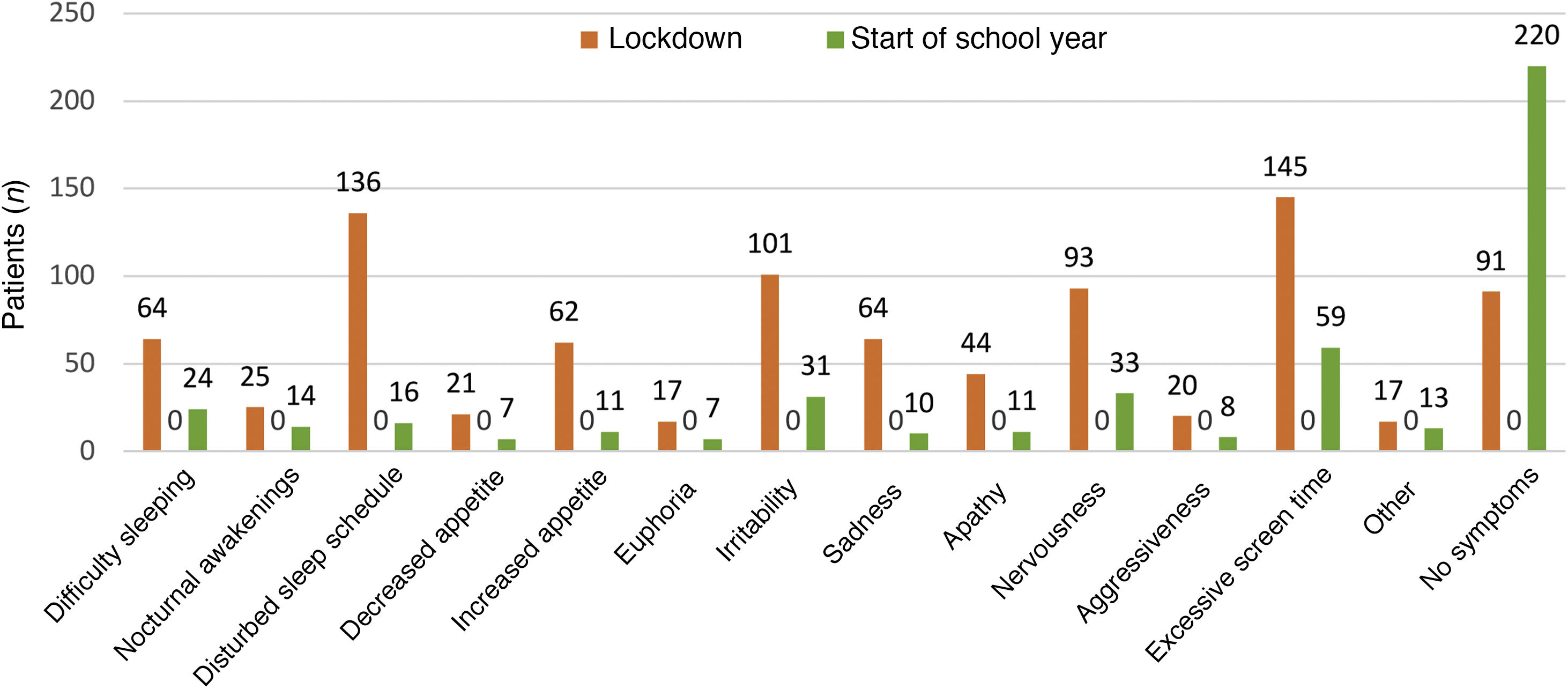
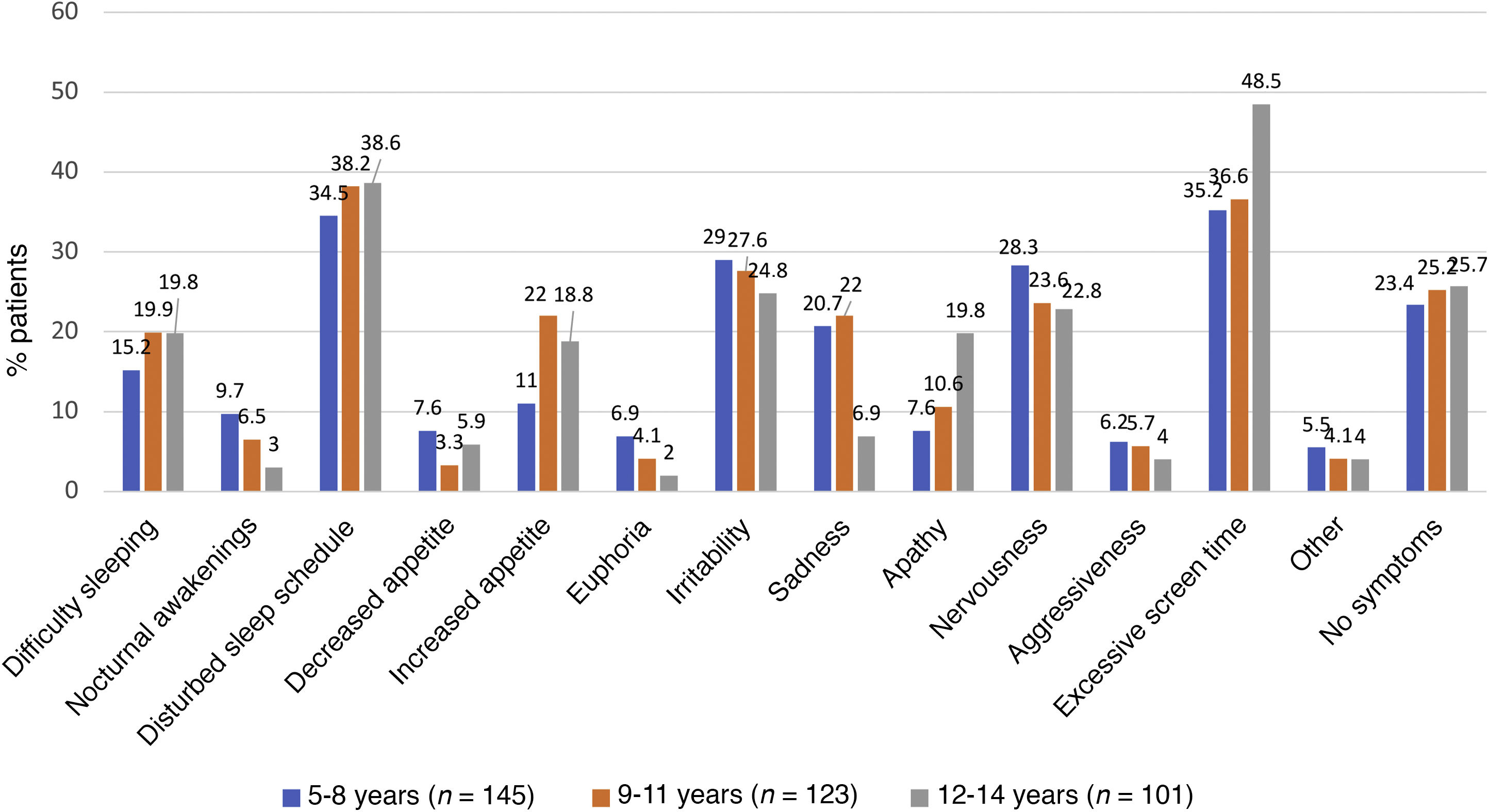
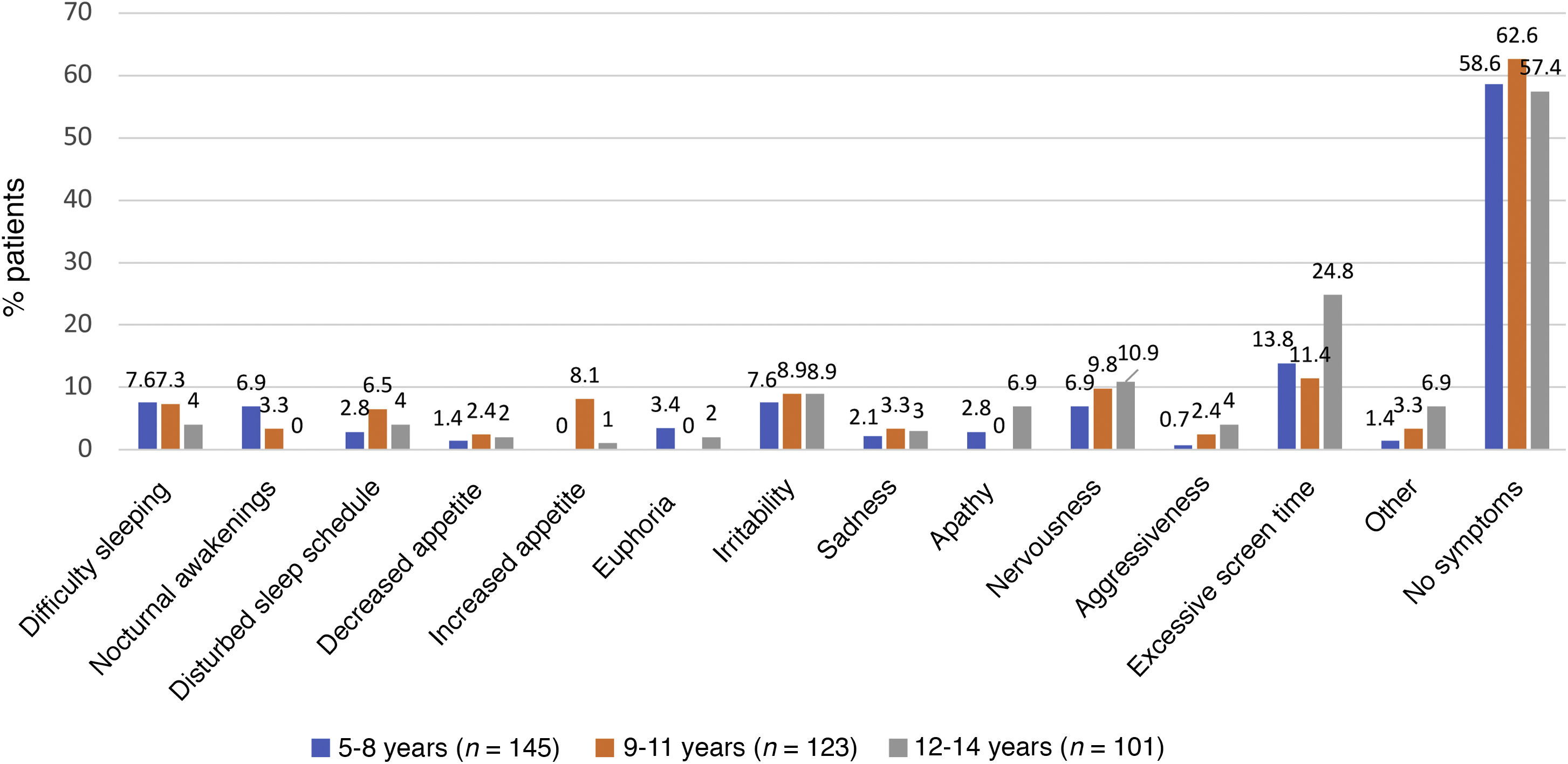
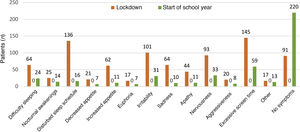
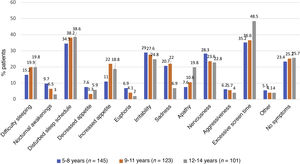
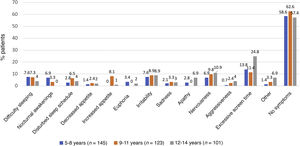
As can be seen in Fig. 4, the overall incidence of emotional symptoms and conduct problems in the sample was significantly higher during the lockdown than at the beginning of the school year, in particular when it came to sadness, nervousness and irritability. We found differences in sleep patterns and screen time, with 62% of participants reporting more than 6 h of screen time during the lockdown compared to 2% at the beginning of the school year. When we compared emotional symptoms and conduct problems by age group (Fig. 5), we found that children aged 5–8 years exhibited irritability, nervousness, euphoria and aggressiveness more frequently during the lockdown. Apathy, sleep disturbances and excessive screen use were more frequent in adolescents aged 12–14 years. During the lockdown, children in all age groups were less physically active and engaged in virtual conferences with family, and 17% gained weight. The difference in the manifestations observed during the lockdown compared to the beginning of the school year were more marked in the group aged 5–8 years (Figs. 5 and 6). The level of worry of children during the lockdown and the beginning of the school year ranged from low to moderate and remained stable, whereas parents were clearly more anxious during the lockdown. The perception of the home life remained stable, ranging from good to very good, in most cases.
The scores obtained at the beginning of the school year (following 6 months of school closure) revealed that mental health problems were probable in 9.8% of patients. Children aged 5–8 years seemed to be most affected. The reported level of worry of children regarding their own health and the health of their families was a risk factor for mental health problems, while a positive perception of the home life had a protective effect. During the lockdown, there was a higher frequency of emotional symptoms and behaviour problems (sadness, irritability and nervousness), sleep disturbances and excessive screen use compared to the beginning of the school year.
When it came to the patients in whom mental health problems were probable, we found a proportion of 9.8% at the start of the school year, which would correspond to an increase of 2 percent points compared to the 7.5% prevalence reported for the 2018–2019 period in Catalonia.18 If we were to add the percentage of patients in whom mental health problems were possible (11.1%) the estimated prevalence would increase to 20.9%, substantially greater compared to the 13.2% reported by the Ministry of Health, also based on SDQ scores, in 2017.25 A higher proportion of patients with a previous diagnosis of mental health or learning had SDQ scores in the abnormal range (30.6%) compared to children without a pre-existing diagnosis (7.2%) (P = 0.000). When we compared our findings to the previous literature, we found that studies that used the SDQ as an assessment tool found similar results in this population (Liu and Ezpeleta).26,27 On the other hand, the data published by Via et al16 show an increase ranging from 13% and 34.7% in the risk of mental health problems, chiefly symptoms of anxiety and depression. The higher frequency of mental health problems found by the latter authors could be due to the use of different instruments for detection and to motivational bias related to recruitment through social media, as opposed to random selection in our study.
Some authors have hypothesised that the magnitude of the impact of home confinement and the pandemic will depend, among other factors, on the age of the child.28 To date, the results in the PEDSAME cohort show a higher frequency of symptoms of irritability, sadness and nervousness during the lockdown in children aged 5–8 years, consistent with the findings of Via et al.16 Other studies, however, have found a higher impact on adolescents.29,30 The higher impact on younger children observed in our study could be explained at least in part by the difficulty at these ages to replace face-to-face interactions with peers with virtual relationships, as restrictions on outdoor activities affect this age group more strongly.
The general belief in the scientific community is that home confinement has a deleterious impact on mental health.31 There is evidence that confinement measures and changes in daily routines has a negative impact on psychological dimensions in the parents, exposing children to significant risks to their wellbeing.32 The results of the PEDSAME study evinced an association between the level of worry children experienced about their own and their families’ health and SDQ scores in the abnormal range. Similarly, Li Duan9 reported an association between psychological symptoms and the strategies used to cope with the situation.
When we analysed the symptoms associated with the lockdown, the PEDSAME study found an increase in sadness, irritability, nervousness, sleep disturbances and excessive screen time compared to the beginning of the school year. Jiao et al33 found similar emotional and behavioural symptoms, with nearly one third of children in their sample reporting irritability, nervousness and sleep disturbances. When it came to the use of electronic devices, the age group that made excessive use at all times (screen time > 6 h/day) was adolescents, and we also found excessive screen time in children with SDQ scores in the abnormal range. This trend had been described previously in the literature.9,34
As for physical activity, the percentage of children that did not engage in any form of physical activity during the lockdown was 9%. This contrasts with the data on vulnerable families published by Save the Children, with percentages above 80%.35 Other authors26 consider that physical activity could be an effective measure for alleviating behavioural problems in confined school-age children. A previous study found an association between engaging in physical activity for less than 1 h a day and mental health problems.34 Orgiles et al15 found that physical activity had a protective effect and that the wellbeing of parents was directly correlated to the wellbeing of children, a finding corroborated by the PEDSAME study, as a positive perception of home life was a protective factor for mental health disorders.
The retrospective collection of data for the lockdown period may be a limitation in our study, as it carries a risk of recall bias. But the time elapsed from the end of the lockdown to data collection was not excessively long and its influence was probably small. Another limitation is that there was little representation of the adolescent population, as paediatric services in the public health system only cover the population aged 14 years and younger and therefore our study did not include any adolescent past that age. In addition, the SDQ was completed by the main caregivers or teachers of participants and not by the children themselves (although participants could complete the questionnaire themselves from age 11–12 years).
The random selection of patients through a network of paediatricians representative of the territory of Catalonia is one of the strengths of the PEDSAME study, as most studies on this subject have used convenience or nonprobability sampling methods.
We must also underscore the usefulness of the SDQ for screening of mental health problems in children and adolescents. The translation to Spanish of this instrument has been validated and exhibited a high internal consistency. Recently, several studies have been published that used this same questionnaire to assess the impact of the COVID-19 pandemic in child and adolescent mental health, reporting outcomes consistent with those obtained in the PEDSAME study.11,26,27,32,36
The PEDSAME cohort study is still ongoing, and the mental health of participants will be assessed through the end of the 2020/2021 academic years at 3 additional time points: December 2020, March 2021 and June 2021. Its longitudinal and prospective design will allow detection of changes in mental health based on the evolution of the pandemic.
ConclusionHome confinement and the closure of schools for 6 months have had a negative impact on the mental health of the child and adolescent population. The most frequent manifestations involved increases in emotional symptoms and conduct problems, sleep disturbances and unhealthy use of screens during the lockdown, and the incidence of psychiatric disorders increased compared to the pre-pandemic period. A positive perception of the home life had a protective effect on mental health, while excessive worry in children was a risk factor for mental health problems.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank the families that spent the time required to complete the questionnaires for the study and the participating primary care paediatrics teams.
Olga Salvadó, Patricia Álvarez, Mercè Bernad, Mireia Biosca, Silvia Burgaya, Montse Delgado, Ramón Capdevila, Jessica Esquivel, Carlos Gatius, María Josep Gellioda, Mireia Giménez, Daniel Gros, Loli Jaramillo, Pyrene Martínez, Ana M. Moreno, Aurora S. Morillo, Alejandro Novoa, Miriam Poblet, Silvia Prado, Celia Pujol, Teresa Pujol, Ángeles Reyes, Anna María Ristol, Pilar Ruiz-Cuevas, Cinta Valldepérez, Elías Vallina, Marta Vera and Mónica Vila.
Previous presentation: This study was presented at the I Annual Virtual Gathering of the Societat Catalana de Pediatria; May 27, 2021; Barcelona, Spain.
Appendix A lists the members of the primary care paediatrics research networks of the Section on Primary Care of the Societat Catalana de Pediatria (Catalonian Society of Paediatrics) (XaRePAP).
Please cite this article as: Gatell-Carbó A, Alcover-Bloch E, Balaguer-Martínez JV, Pérez-Porcuna T, Esteller-Carceller M, Álvarez-Garcia P, et al. Estado de la salud mental infantojuvenil durante la primera ola de la pandemia de la COVID-19 y en el inicio del curso escolar 2020−2021. An Pediatr (Barc). 2021;95:354–363.