Edited by: Azucena Díez-Suárez
University Clinic of Navarra. Pamplona. Spain
Pedro Javier Rodríguez-Hernández
University Hospital Complex Ntra Sra de Candelaria. Tenerife. Spain
Last update: August 2025
More infoSomatic symptoms affect approximately 25% of children and adolescents, with a significant impact in 10%, and somatization disorders affect 1%–3% of the population. In addition to somatic symptom disorder, illness anxiety disorder (or hypochondria), conversion disorder and factitious disorder may be common reasons for seeking care. Somatization is associated with anxiety and depressive symptoms throughout the lifespan. There are widespread myths regarding somatization, and it is essential that all professionals who treat children are familiar with them. The basis of the treatment of somatization is the development of an individualized rehabilitation program with the main goal of gradually returning to normal function. A paediatrician, psychiatrist or psychologist can direct the treatment, but the approach must always be interdisciplinary, including nursing staff, physical and occupational therapists, teachers or school counsellors. There is limited evidence on the treatment of somatic symptoms, but cognitive behavioural therapy and antidepressants have been found to be effective in cases of greater severity or with psychiatric comorbidity. Analgesics should be used rationally, favouring non-pharmacological pain management measures.
Las somatizaciones afectan a aproximadamente 25% de los niños y adolescentes, en el 10% ocasionan un impacto importante, y los trastornos de somatización al 1%–3% de la población. Además de los trastornos somatomorfos, el trastorno de ansiedad por enfermedad (o hipocondría), los conversivos y los trastornos facticios pueden ser motivos de consulta habituales. Las somatizaciones se asocian a síntomas de ansiedad y depresivos a lo largo de la vida. Los falsos mitos relativos a las somatizaciones son frecuentes y es imprescindible que todos los profesionales que tratan a niños estén familiarizados con ellos. La base del tratamiento de las somatizaciones es la elaboración de un programa de rehabilitación individualizado, cuyo objetivo principal es volver de forma progresiva a la normalidad. Lo puede dirigir un pediatra, psiquiatra o psicólogo, pero el abordaje siempre debe ser interdisciplinar, incluyendo a enfermería, profesores, fisioterapeutas, terapeutas ocupacionales, profesores u orientadores escolares. La evidencia de los tratamientos es limitada, pero la terapia cognitivo conductual y los antidepresivos en los casos más graves o de comorbilidad psiquiátrica son efectivos. Se debe indicar un uso racional de analgésicos, favoreciendo medidas no farmacológicas para el dolor.
Somatization is defined as the experience of physical symptoms in the absence of abnormal results in the medical evaluation. The cause is mental, but the patients experience physical symptoms instead of psychological symptoms. When children experience somatization, particularly in the case of somatic symptom disorders, they and their families tend to attribute the symptoms to a different kind of disease, despite evidence to the contrary from physical examinations and diagnostic tests. Somatic symptom disorders can be severe and have an irreversible impact in the current and future adult life of the child and of the family. Somatic symptoms can be precursors to other psychiatric disorders, especially anxiety and depressive disorders. The current consensus suggests that the term “somatization” or “somatoform” is more appropriate than alternative terms, given their connotations:
- •
Functional: this refers to the function affected by the symptom, but there is not always such a function, or it may not be consistent.
- •
Psychogenic (psyche, “soul”; geno, “birth” or “origin”): may lead to confusing somatization with factitious disorders
- •
Non-organic: incorrect, as all psychiatric symptoms and disorders originate in one organ—the brain.
Somatic symptoms, especially if they are moderate or severe, are difficult to understand and can be a source of frustration for health care providers. Since they do not fit the classic model of medicine (symptom/finding of examination or assessment), these symptoms are usually met with skepticism. Providers that manage patients with somatization are overwhelmed by the frequency of the visits, the increased use of health care resources and the tension that arises in the interactions with the family and the patient. False beliefs about somatic symptoms are widespread in our society and also abound among health care providers. Some of the most frequent myths are1:
- •
Patients who somatize are weaker
- •
Children make up the symptoms to get attention or for evasion purposes
- •
The family is to blame
- •
If many tests are performed, the problem will be identified
- •
If the child is ignored, the symptoms will disappear
- •
With tough love, you can have the child go to school
Pediatricians and other health care professionals must help debunk these prejudices, and this requires adequate knowledge and demanding that sufficient time be allocated for visits in order to properly explain the nature of the ailment to the child and the family. Although support from mental health professionals may be necessary in the most severe cases, the approach adopted from the initial contact with the health care system is key to manage the situation appropriately, avoiding performance of unnecessary tests and teaching parents how to respond to symptoms so that they do not worsen and can be extinguished over time.
Types of symptoms and disordersPractically any physical complaint could be a somatic symptom, although nonspecific symptoms are most common, such as asthenia or pain (chiefly headache, abdominal pain or back pain). We ought to specifically mention neurologic symptoms, encompassed in the particular diagnostic label of conversion disorder, which manifests with symptoms such as paralysis or paresthesia, among others. In some cases, somatization may manifest in uncommon or even bizarre forms, such as sneezing, hearing loss, pregnancy…
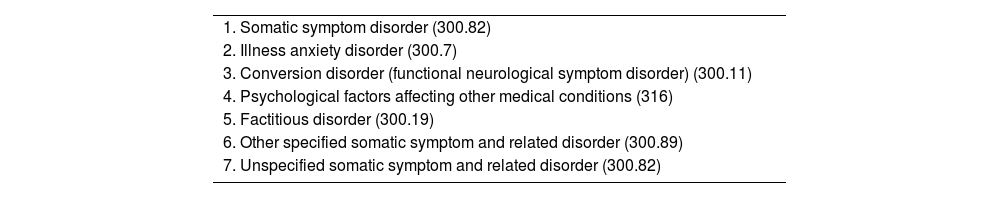
Somatic symptom disorder refers to the presence of somatic symptoms that are very frequent, intense or have a significant impact on the life of the child. Somatic symptom and related disorders are recognized and featured in the classifications of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) and the International Classification of Diseases, 11th Revision (ICD-11) (Table 1). Their diagnosis requires that the criteria be met for a minimum of 6 months. The criteria are not different for children versus adults.2–4 We now proceed to summarize the characteristics of the main disorders in this category:
Somatic symptom and related disorders, DSM-5 classification.
| 1. Somatic symptom disorder (300.82) |
| 2. Illness anxiety disorder (300.7) |
| 3. Conversion disorder (functional neurological symptom disorder) (300.11) |
| 4. Psychological factors affecting other medical conditions (316) |
| 5. Factitious disorder (300.19) |
| 6. Other specified somatic symptom and related disorder (300.89) |
| 7. Unspecified somatic symptom and related disorder (300.82) |
DSM-5, Diagnostic and Statistical Manual of Mental Disorders, fifth edition.
The symptoms cause significant disruption of daily life, for instance, school absenteeism, decreased engagement in activities or social isolation. The thoughts and feelings associated with the symptoms are disproportionate, persistent and anxiety-producing. The child (and family) devote (this is the verb used in the DSM-5, which is illustrative of the situation) excessive time and energy to these health concerns.
Illness anxiety disorderPreviously known as hypochondriasis, it consists in an excessive worry about having or contracting a disease, but, unlike the previous disorder, somatic symptoms are either absent or mild. The associated anxiety is intense, as are the behaviors related to the perceived or feared illness, which may be disproportionate, leading to excessive consultations or requests for testing or, on the contrary, avoidance of seeking care due to the anxiety it produces.
In pediatric care, it is not unusual to encounter a “lethal” combination in which a child exhibits somatization while a parent exhibits hypochondria. This should not be confused with factitious disorder imposed on another, which is much less frequent.
Conversion disorderThe main features are the presence of symptoms of altered motor or sensory function and findings of the examinations or tests performed that are incompatible with the reported symptom. The most frequent manifestations are syncope and non-epileptic seizures. To differentiate epileptic from non-epileptic seizures, it is useful to take an exhaustive history exploring different aspects of the child’s life (school, friends, family) and examine home video recordings. In addition to the presence of stressors that could act like triggers, some signs and symptoms have been proposed to help differentiate them. Asynchronous activity, pelvic thrusting, opisthotonus, post-ictal somnolence that can be lifted with other stimuli or the occurrence of seizures only in certain places or situations suggest that the seizures are non-epileptic in nature.5
Factitious disorderAlthough factitious disorder is classified within this group of disorders, they actually differ from somatization in that the child intentionally falsifies the symptoms, injuries or diseases.6 In this case, the child is not “truly suffering” from these manifestations. A classic example would be to bring a thermometer close to a heat source to pretend having a fever. In the case of factitious disorder imposed on another, it is the parent or main caregiver who falsify the symptoms. In factitious disorders, the benefit for the patient may vary: it may be avoiding a dreaded situation (like going to school), a material gain (money, some form of assistance or social recognition) or a psychological reward (remaining hospitalized, for the parents not to divorce). In some cases, the same child or adolescent can exhibit both somatic and factitious symptoms through the lifespan, concurrently or at different times.
Epidemiology: what is the prevalence in the pediatric population?It is estimated that 25% of the population aged less than 18 years complains of one or more of these symptoms weekly. Of all children who visit the pediatrician for any reason, approximately 10% have physical symptoms that cannot be attributed to any recognizable disease but have a significant impact on their daily life.7 The estimated prevalence of somatic symptom disorders is approximately one to three percent.8–10 These complaints usually affect the patient’s quality of life, family and social adaptation, cognitive development, academic performance and mood. The most frequent type is somatic symptom disorder, followed by conversion disorder. The most frequent presenting complaints are headache, abdominal pain, generalized pain and globus. Non-epileptic seizures and syncope are the most frequent manifestations in conversion disorder.8 Overall, there is a higher prevalence of these disorders in the female population, and the age at onset is greater in conversion disorder compared to somatic symptom disorder.9,10
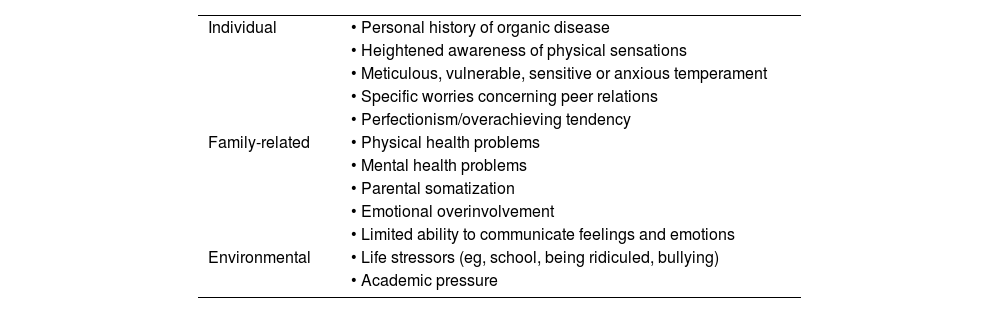
Risk factorsThere is no specific single risk factor for the development of somatic symptoms. Some risk factors are individual, some are family-related and some are environmental. Children who experience illness personally or in their immediate environment, among their loved ones, are more likely to develop somatic symptoms. That is, it is not only possible but also probable that somatic symptoms and other types of illness co-occur. Table 2 summarizes the main risk factor for somatic symptoms. Some children are more prone to somatization, and the individual factors associated with increased vulnerability to these symptoms are11–13:
- •
Difficulties in verbal expression and especially in verbalizing emotions (tendency toward alexithymia)
- •
Perfectionist, anxious, obsessive, insecure or fearful temperament, as these traits are associated with less effective coping strategies
- •
Lower pain threshold (Fig. 1).
Risk factors for somatization in children and adolescents.
| Individual | • Personal history of organic disease |
| • Heightened awareness of physical sensations | |
| • Meticulous, vulnerable, sensitive or anxious temperament | |
| • Specific worries concerning peer relations | |
| • Perfectionism/overachieving tendency | |
| Family-related | • Physical health problems |
| • Mental health problems | |
| • Parental somatization | |
| • Emotional overinvolvement | |
| • Limited ability to communicate feelings and emotions | |
| Environmental | • Life stressors (eg, school, being ridiculed, bullying) |
| • Academic pressure |
Source: adapted from Garralda, 2005.14
Difficulties or changes in the family, such as marital problems, moving, diseases or deaths, not to mention any form of neglect or abuse and the presence of recurrent somatization in parents, can have an impact on the development of somatic symptoms in children.13 Extreme parenting styles, such as authoritarian or invalidating parenting or, on the other extreme, overprotective parenting, are risk factors for the development and especially the chronification of somatization.1 One of the most common complications is school absenteeism or refusal, so it is important to explore whether the child is experiencing suffering in relation to the school. It could be due to academic difficulties, social rejection or bullying from peers or any form of abuse on the part of the teaching staff or other adults in contact with the child.13,14
Psychiatric comorbiditiesThe presence of other psychiatric disorders is very common in children who have somatic symptom and related disorders is very common, as it is estimated that 50%–90% have such comorbidities.10,11,15,16 For instance, the risk of anxiety disorder is five times greater in children with recurrent abdominal pain.11 In adolescents with chronic pain, the overall risk of having a psychiatric comorbidity of any kind increases by two- to three-fold.16 They are not only more likely to experience anxiety, depression or post-traumatic stress, but also of oppositional defiant or conduct disorder, eating disorders and substance use.16 It has been hypothesized that there is a dose-response mechanism in this relationship: the more severe the somatization and its impact on the child's life, the greater the risk and severity of psychiatric comorbidities15
Treatment of somatic symptomsThe appropriate treatment for somatization depends on its severity and the degree of suffering and impairment that it causes. However, in essence, the approach is always the same: to try to avoid disruptions in the patient’s everyday life, to which end an interdisciplinary and coordinated care plan is required. The better the training of the providers managing the child on the foundations of somatic symptoms, the better the patient outcomes will be. Due to the skepticism and misconceptions that we discussed above, the feelings of dissatisfaction and being misunderstood of children and their families may be a good starting point.
The first step is to explain the characteristics of somatic symptoms and convey a clear and unified message to the family and the child, in a developmentally appropriate manner, avoiding performance of unnecessary tests or visits to additional specialists. The evidence on the management of disorders involving somatization is limited due to the heterogeneity of the symptoms, their classification, the skepticism, the lack of training on the subject and the current conditions of care delivery in the primary care setting. Overall, cognitive-behavioral interventions and the use of antidepressants in cases of psychiatric comorbidity (the majority) have been found to be effective.17,18,25
The care plan should be individualized to each particular child, situation and family, guided by a multidisciplinary team that may include psychologists, psychiatrists, pediatricians, pediatric neurologists, nurses, technicians and physical, occupational or speech therapists, among others. Active involvement of the family, the school and any other important setting in the child’s life is necessary for the treatment to succeed.8,25 Medication may be needed to reduce anxiety or depression, and the use of other drugs, such as analgesics, should be restricted. The use of placebos is rarely helpful. In severe cases, the patient may require inpatient pediatric or psychiatric care.
Cognitive-behavioral interventionsCognitive-behavioral interventions are aimed at identifying and changing maladaptive thoughts and behaviors that deviate from normal functioning and promote the persistence of the symptom in order to develop more adaptive and appropriate ones. It is the first-line treatment, and the use of psychotherapy does not exclude other approaches, such as physical therapy or medication. Cognitive-behavioral therapy has been studied in the context of chronic fatigue and found effective in several pediatric populations.22,24 Its primary objective is to improve the functioning and coping skills of the child in different situations.23 In many cases, it focuses on helping the patient “live with the symptom”. For this to succeed, it is important to train patients and their families in specific techniques to make symptoms more manageable: distraction, coping strategies, extinction, relaxation training and behavioral activation.23 Education in the rational and moderate use of analgesics or an individualized exercise plan to address muscular problems are also frequently included in the management of psychosomatic pain or fatigue. Treatment should start with simple goals, progressively working toward more complex goals (gradual return to school, doing homework) until daily activity has normalized.
Training in mindfulness and relaxation techniquesOne of the most widely used and effective technique in children aged 4–12 years, approximately, is the Koeppen relaxation technique adapted for children. It involves a series of sessions guided by a professional and thereafter by trained family members, where the child is told step by step what to do. The technique should be taught and practiced a at a quite time in a comfortable setting, and, once learned, applied daily. Usually, daily practice at midday and at night is recommended, as physical tension and worry tend to accumulate in the course of the day. Relaxation sessions could offer a pleasant and comfortable break and reduce this physical tension and worry.
Mindfulness-based techniques involve training the patient to focus on the current activity and stay in the moment, trying to avoid dwelling on the past or the future. There are mindfulness programs adapted for children and adolescents and there is a growing body of evidence on their usefulness in the management of multiple diseases.19
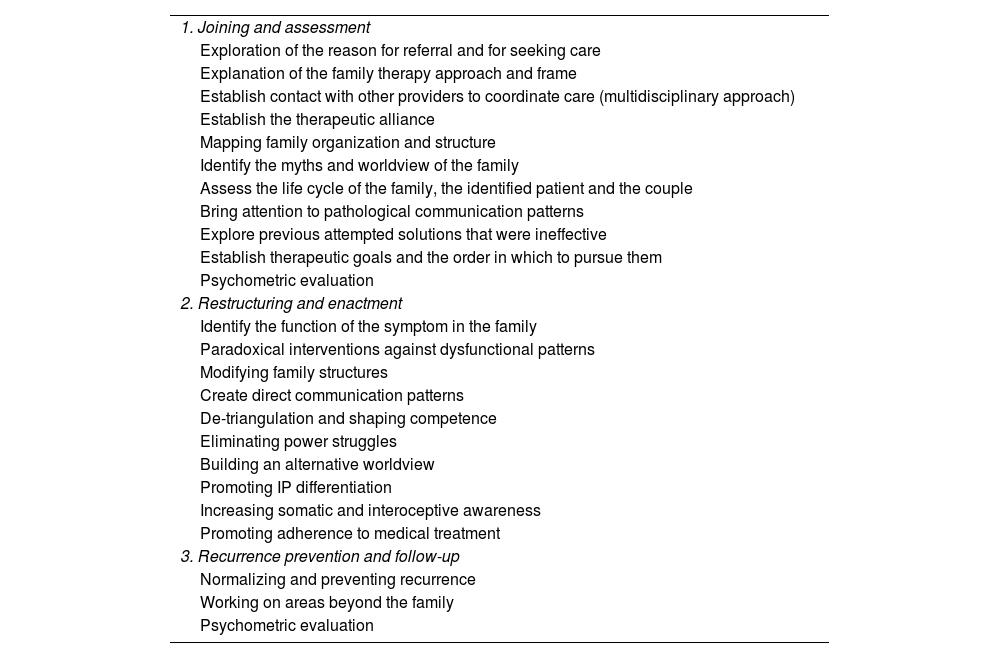
Specific family-based interventionsThe family is unquestionably one of the most important and influential pillars in our life, especially for children and adolescents. Family-centered interventions, as opposed to interventions focusing solely on the patient and the symptoms, offer the opportunity to assess the relationships and interactions between family members. Family therapy is not indicated in every case of somatization, but in most cases an understanding of its basic principles is useful in their management. In many cases of somatization, the symptom is a factor that promotes cohesiveness in the family: “if I heal, my parents will separate” is a common line of thought in children with severe somatization.20,21Table 3 presents the different stages and goals of family systems therapy.
Phases of family therapy.
| 1. Joining and assessment |
| Exploration of the reason for referral and for seeking care |
| Explanation of the family therapy approach and frame |
| Establish contact with other providers to coordinate care (multidisciplinary approach) |
| Establish the therapeutic alliance |
| Mapping family organization and structure |
| Identify the myths and worldview of the family |
| Assess the life cycle of the family, the identified patient and the couple |
| Bring attention to pathological communication patterns |
| Explore previous attempted solutions that were ineffective |
| Establish therapeutic goals and the order in which to pursue them |
| Psychometric evaluation |
| 2. Restructuring and enactment |
| Identify the function of the symptom in the family |
| Paradoxical interventions against dysfunctional patterns |
| Modifying family structures |
| Create direct communication patterns |
| De-triangulation and shaping competence |
| Eliminating power struggles |
| Building an alternative worldview |
| Promoting IP differentiation |
| Increasing somatic and interoceptive awareness |
| Promoting adherence to medical treatment |
| 3. Recurrence prevention and follow-up |
| Normalizing and preventing recurrence |
| Working on areas beyond the family |
| Psychometric evaluation |
IP, identified patient.
Source: adapted from Gómez Holgado.21
In children, the placebo effect tends to be even larger than in adults. While it is true that it can help symptoms improve in some individuals, especially those who are highly suggestible, it is never the sole or best solution. Therefore, generally speaking, the use of placebo, for instance, empty gelcaps or fluids without medication, or pharmacy products of unproven effectiveness, is not usually recommended for management of somatization. In some cases, placebo may be used in a time-limited fashion for diagnostic confirmation.
Rational use of analgesicsWhen somatization manifests as pain, children usually take analgesics, anti-inflammatories or, in the most severe cases, even opiates. Usually, somatic symptoms do not respond or only transiently respond to analgesics, which in many cases results in excessive use of these drugs. By definition, analgesics are not indicated for somatic symptoms, so the goal is to completely withdraw them. It is the duty of every care team to help patients with somatic symptoms and their families use these drugs appropriately. Nonpharmacological pain management strategies, such as rehabilitation, relaxation or even hypnosis, should be proposed as an alternative.17
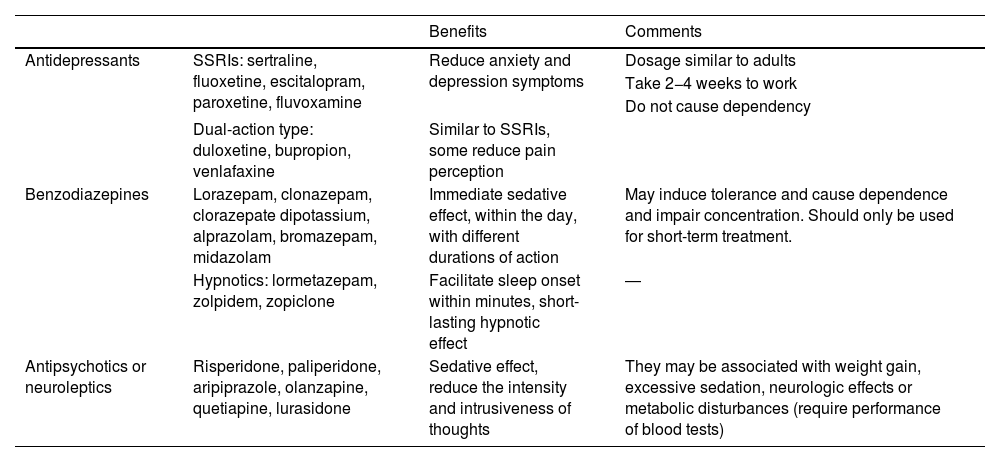
Psychiatric drugsThe main types of drugs that can be used to improve somatization are the same prescribed to treat depression or anxiety, chiefly antidepressants, but also benzodiazepines or antipsychotics.10,11 Antidepressants are indicated in cases in which somatization is associated with anxiety or depression.1,16,17 Some drugs, like duloxetine, although not indicated for use in children or adolescents, can lower the pain threshold.16Table 4 presents the most commonly used psychiatric drugs, summarizing its potential benefits and aspects that need to be taken into account.
Psychotropic drugs used most widely in the management of somatization.
| Benefits | Comments | ||
|---|---|---|---|
| Antidepressants | SSRIs: sertraline, fluoxetine, escitalopram, paroxetine, fluvoxamine | Reduce anxiety and depression symptoms | Dosage similar to adults |
| Take 2−4 weeks to work | |||
| Do not cause dependency | |||
| Dual-action type: duloxetine, bupropion, venlafaxine | Similar to SSRIs, some reduce pain perception | ||
| Benzodiazepines | Lorazepam, clonazepam, clorazepate dipotassium, alprazolam, bromazepam, midazolam | Immediate sedative effect, within the day, with different durations of action | May induce tolerance and cause dependence and impair concentration. Should only be used for short-term treatment. |
| Hypnotics: lormetazepam, zolpidem, zopiclone | Facilitate sleep onset within minutes, short-lasting hypnotic effect | ― | |
| Antipsychotics or neuroleptics | Risperidone, paliperidone, aripiprazole, olanzapine, quetiapine, lurasidone | Sedative effect, reduce the intensity and intrusiveness of thoughts | They may be associated with weight gain, excessive sedation, neurologic effects or metabolic disturbances (require performance of blood tests) |
SSRI, selective serotonin reuptake inhibitor.
Somatic symptoms that do not fulfil the criteria for a disorder occur in most of the population at some point, and they usually resolve, as long as they are correctly identified and their nature understood. In individuals prone to somatization, they can become chronic, and in this adults it is common for somatic symptoms to be associated with symptoms of depression and anxiety.26 Somatoform disorders are associated with a level of impairment similar to the level observed in depression, with an enormous impact on quality of life, as well as sizable costs due to medical expenses and disability interfering with work in adulthood.7 Adequate treatment in childhood offers a great opportunity to prevent this outcome. Studies in adults suggest that in approximately two thirds of the cases, somatic symptoms resolve, in half, they persist at 1 year from onset, and in 10%, somatization persists for the entire life of the patient. The factors associated with poorer prognosis are female sex, neurologic symptoms, comorbid depression and parental psychiatric disease.7,9 Outcomes depend on the presence or absence of perpetuating factors and access to adequate treatment. In most cases, particularly in conversion disorder, the prognosis is far better compared to other illnesses, such as tumors, epilepsy or degenerative diseases. This is usually a key point to highlight in working with the families of children with conversion disorder.
ConclusionSomatic symptoms are very frequent in children and adolescents, and somatoform disorders occur in 1%–2% of the pediatric population. In more than half the cases, they are associated with psychiatric disorders, chiefly anxiety and depression, although there may be other psychiatric comorbidities. The factors associated with their development are certain personality traits (introversion, insecurity), difficulties with verbal expression, family dysfunction and the presence of disease or abuse. The impact of somatoform disorders is comparable to that of depression, as they affect cognitive and social functioning and work performance in adulthood. The treatment is based in the implementation of an individualized rehabilitation plan with the objective of normalizing daily activity. There is evidence that cognitive-behavioral therapy and antidepressants can improve somatization. The prognosis is favorable in most cases, and is poorer in female patients or in patients whose parents have psychiatric disorders.