Paediatric rheumatology has well-defined characteristics, including the diseases included in its scope of practice,1 the training objectives for professionals that practice it2 and the requirements that must be met by health care units in the field.3 In the United States, this subspecialty has been recognised since 1992 and requires a training programme lasting 3 years. In Europe, a specialist training curriculum of 2 years’ duration has been developed that is endorsed by the Paediatric Rheumatology European Society and the European Board of Rheumatology.
In spite of this, and as is the case of other paediatric subspecialties, specialisation in paediatric rheumatology is still not recognised in Spain.4 In addition, since this field deals with diseases that often have a low prevalence, there are few units with a high level of clinical experience, which results in considerable heterogeneity in management and inadequate specialised training for residents in many hospitals. All of the above can have a negative impact on the care of children with rheumatic disease.4,5
To assess how the care of paediatric patients with rheumatic disease is organised in Spain and the perception of paediatricians and residents in paediatrics of the need for specific training in paediatric rheumatology, we conducted a cross-sectional, multicentre and descriptive nationwide study by means of an anonymous questionnaire (GoogleDocs®). We disseminated the questionnaire among paediatricians and residents of paediatrics in August and September of 2017 through electronic mail and social networks.
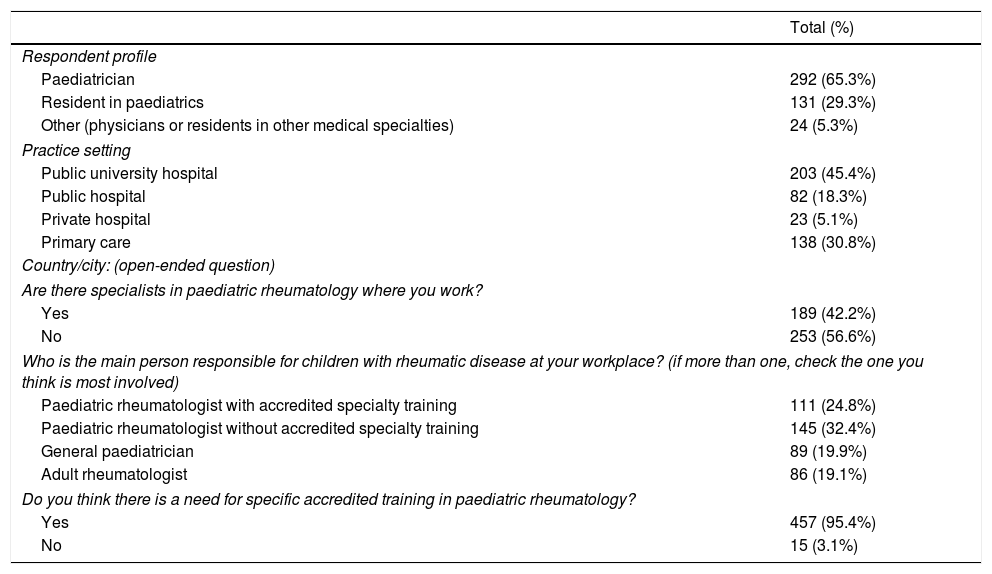
We obtained 447 responses (Table 1). The sample included 292 physicians specialised in paediatrics (65.1%) and 131 medical residents in paediatrics (29.2%). The remaining 24 respondents (5.3%) were physicians and residents in other specialties (rheumatology, family medicine and immunology). The geographical distribution of responses was: Madrid, 180; Basque Country, 39; Castilla y Leon, 33; Andalusia, 25; Asturias, 23; Catalonia, 22; Balearic Islands, 14; Galicia, 11; Navarre, 8; Castilla-La Mancha, 6; Extremadura, 6; Murcia, 6; and Canary Islands, 3. The distribution by work setting was: primary care (45%), hospital (49%) and private medical practices (6%).
Answers to the questionnaire on training in paediatric rheumatology.
| Total (%) | |
|---|---|
| Respondent profile | |
| Paediatrician | 292 (65.3%) |
| Resident in paediatrics | 131 (29.3%) |
| Other (physicians or residents in other medical specialties) | 24 (5.3%) |
| Practice setting | |
| Public university hospital | 203 (45.4%) |
| Public hospital | 82 (18.3%) |
| Private hospital | 23 (5.1%) |
| Primary care | 138 (30.8%) |
| Country/city: (open-ended question) | |
| Are there specialists in paediatric rheumatology where you work? | |
| Yes | 189 (42.2%) |
| No | 253 (56.6%) |
| Who is the main person responsible for children with rheumatic disease at your workplace? (if more than one, check the one you think is most involved) | |
| Paediatric rheumatologist with accredited specialty training | 111 (24.8%) |
| Paediatric rheumatologist without accredited specialty training | 145 (32.4%) |
| General paediatrician | 89 (19.9%) |
| Adult rheumatologist | 86 (19.1%) |
| Do you think there is a need for specific accredited training in paediatric rheumatology? | |
| Yes | 457 (95.4%) |
| No | 15 (3.1%) |
Of all respondents, 56.6% reported that there were no specialists in paediatric rheumatology in their hospitals. A similar percentage (57.2%) believed that the clinician that was mainly responsible for the management of children with rheumatic diseases was a paediatric rheumatologist, with 32.4% reporting that this clinician did not have accredited training in this subspecialty and 24.8% that the clinician did have this training. Another 19.9% reported that the physician usually in charge of these patients was a general paediatrician, while 19.1% reported it was an adult rheumatologist. In addition, 95.3% of respondents advocated for the establishment of accredited training in paediatric rheumatology, and 52.5% considered that this specialised training should last 2 years.
Paediatric rheumatology is one of the most recent paediatrics subspecialties to emerge; at present it is not officially recognised, and there are no established minimum qualifications to practice it or a formal training curriculum on this subspecialty.4 Specific education in this field is truly needed,5 as asserted by most respondents (95.3%). In Spain, any professional in the field of paediatrics or of rheumatology can manage children with rheumatic disease. The results of our survey reflect that in 39% of cases, the main professional in charge of the management of children with rheumatoid disease is not a paediatric rheumatologist (general paediatrician in 19.9% and rheumatologist in 19.1%).
We ought to highlight that 24.8% of respondents believed that children with rheumatic disease were managed by paediatric rheumatologists with officially accredited training in the field, even though the subspecialty is not recognised as such in Spain. This discrepancy is due to the confusion of formal “specialization” in a particular field of paediatrics and the completion of a longer rotation, of variable duration, in the last year of the residency programme, the latter being the usual pathway to achieving more specialised knowledge in the absence of a formal accredited curriculum. As an alternative, the establishment of “specific qualification areas” in paediatrics (Royal Decree 639/2014) opened the doors to the regularization of these professional fields, but the decree was repealed on 12/12/2016.6 In the field of paediatric rheumatology, despite the development of a specific training programme by the Education and Training Committee of the Paediatric Rheumatology European Society, there is currently no official consensus or recognition allowing accreditation in this field.
There are some limitations to our survey. To facilitate and simplify participation, we did not ask respondents about their age or sex, so we cannot determine the degree to which the sample was representative of Spanish paediatricians and residents in paediatrics. Furthermore, its dissemination through working groups and social networks and the short period for submitting responses may have been a source of selection bias.
This survey reinforces the perception that training in paediatric rheumatology needs to be improved in Spain. Its findings evince the heterogeneity in the management of paediatric patients with rheumatic disease, while most respondents acknowledge that there was a lack of specific training in this field.
We thank doctors Lacassagne, Erika Sifuentes and Parichat Khaosut.
Please cite this article as: Udaondo Gascón C, Murias Loza S, Alcobendas Rueda R, Remesal Camba A, de Inocencio Arocena J. ¿Debe mejorar la formación en reumatología pediátrica? Resultados de una encuesta nacional. An Pediatr (Barc). 2020;92:165–166.