Acute kidney injury (AKI) is a severe complication in critically ill children. The aim of the study was to describe the characteristics of AKI, as well as to analyse the prognostic factors for mortality and renal replacement therapy (RRT) in children admitted to Paediatric Intensive Care Units (PICUs) in Spain.
Patients and methodsProspective observational multicentre study in children from 7 days to 16 years old who were admitted to a PICU. A univariate and multivariate logistic regression analysis of the risk factors for mortality and renal replacement therapy at PICU discharge were performed.
ResultsA total of 139 cases of AKI were analysed. RRT was necessary in 60.1% of cases. Mortality rate was 32.6%. At PICU discharge, RRT was necessary in 15% of survivors. Thrombopenia and low creatinine clearance values were prognostic markers of RRT at PICU discharge. High values of platelets, serum creatinine and weight were associated with higher survival.
ConclusionsCritically ill children with AKI had a high mortality and morbidity rate. Platelet values and creatinine clearance are markers of RRT at PICU discharge, whereas number of platelets, serum creatinine and weight were associated with mortality.
El daño renal agudo (DRA) es una complicación grave en niños críticos. El objetivo de este estudio fue describir las características de esta patología en las Unidades de Cuidados Intensivos Pediátricos (UCIP) españolas e identificar factores de riesgo asociados con la mortalidad y la necesidad de depuración extrarrenal al alta.
Pacientes y métodosEstudio prospectivo observacional multicéntrico que incluyó niños de 7 días a 16 años de edad con DRA ingresados en UCIP. Se realizó un estudio univariante y multivariante de los factores de riesgo asociados con la mortalidad y necesidad de depuración extrarrenal al alta.
ResultadosSe analizaron 139 casos de DRA. En el 60,1% de los casos fue necesaria la utilización de alguna técnica de depuración. La mortalidad durante el ingreso fue del 32,4% y el 15,1% de los supervivientes necesitaban diálisis al alta de la UCIP. En el estudio de regresión logística multivariante la trombocitopenia y los valores bajos de aclaramiento de creatinina fueron factores pronósticos que predijeron la necesidad de diálisis al alta. Ajustando por peso, las cifras elevadas de plaquetas y creatinina se relacionaron con una mayor supervivencia.
ConclusionesLos niños críticamente enfermos con DRA presentan una morbimortalidad elevada. La cifra de plaquetas y el aclaramiento de creatinina son marcadores de necesidad de diálisis al alta de la UCIP y la cifra de plaquetas, la creatinina sérica y el peso, marcadores de supervivencia.
Acute kidney injury (AKI) is a severe complication in Paediatric Intensive Care Units (PICU), with a mortality rate of between 30 and 44%.1–5
Over the past few years, studies have been performed using one of 2 standardised definitions of AKI: the modified paediatric RIFLE criteria (pRIFLE)6 or the classification system Acute Kidney Injury Network (AKIN).7 These studies have shown the different impact of AKI on critically ill children, due to variations in severity and in the inclusion criteria of study populations. However, all have found that AKI is associated with a longer hospital stay and higher mortality.8,9
Since AKI in critically ill children has high morbidity and mortality, it is necessary to investigate prognostic markers, which will detect patients who may benefit from prompt treatment.10 The objective of this study is to describe the epidemiological characteristics of AKI in Spanish PICUs and to identify risk factors that will predict mortality and the need for renal replacement therapy after discharge from the PICU.
Patients and methodsA multi-centre prospective observational study was conducted in 19 Spanish PICUs for one year (15 October, 2002–15 October, 2003), taking as reference a previous pilot study conducted in 4 units.4
The study included children aged between 7 days and 16 years, presenting acute alteration of kidney function, excluding premature new-born babies. Among children with chronic kidney failure and acute worsening of kidney function, AKI is defined as a 25% serum creatinine increase above baseline level in a maximum period of 72h. Re-admissions of patients with a new episode of AKI are considered independent cases. AKI was defined as serum creatinine higher than 2 standard deviations (SD) above the normal value for the patient's age.11 Patients were classified retrospectively according to the changes in creatinine values based on pRIFLE criteria6: 23.3% were classified with “Injury” status, and 73.5% as “Failure”, with 3.2% at “Risk”. On PICU discharge, 10% had “Loss” status and 6.7% were at “End stage”.
For all patients, the age, weight, sex, Paediatric Risk of Mortality Score (PRISM II),12 cause of AKI, type of AKI (oliguric or preserved diuresis), clearance techniques, medical complications, organ dysfunction,13 serial analytical data (on PICU admission, on AKI diagnosis, at 24h of diagnosis, at the beginning of dialysis, at the end of the latter, and at PICU discharge), were recorded, as well as the maximum change in urea, creatinine, creatinine clearance (calculated by means of the Schwartz equation), glucose, acid-base balance, ions, proteins, uric acid, lactate and haemogram, need for dialysis on PICU discharge, mortality, and causes of the latter. The maximum change in creatinine and urea, and the minimum platelet value refer to the maximum and minimum values reached during admission, respectively.
Continuous variables were described by means of mean±standard deviations or by medians and ranges. Categorical variables were described by means of absolute and relative frequencies. The comparisons of continuous and categorical variables were made by means of the Mann–Whitney and the chi-square tests, respectively. Multivariate logistic regression analyses were used to develop prognostic criteria. Variables were introduced into these models, based on the likelihood ratio criterion. To minimise data loss, variables that did not fit the model were excluded. The area under the curve (AUC) “Receiver Operating Characteristic” (ROC) was used to measure the prognostic capability of the models. To minimise the effect of missing values, the “general bootstrap algorithm” was used for the comparison with the AUC.14 Significant differences were defined as those with a “p” lower than 0.05. The data was processed by means of the free software R.3.1 (www.r-project.org).
ResultsThere were 7119 admissions, with 143 cases (2%) of AKI, during the study period. Four cases were excluded due to absence of data. The mean age±SD was 51.8±57.4 months. In 49.6% of cases, patients were under two years (34,8% under 12 months). Oligoanuria accounted for 66.7% of all cases. The main causes were postoperative complications (25.2%): congenital heart disease (33 cases), pulmonary transplant (2 cases), and liver transplant (one case), infectious processes (24.5%), 97% of which involved sepsis, and renal pathology (20.3%), most of which (7.7%) involved haemolytic uraemic syndrome. Other triggering pathologies included problems with the heart (9.1%), digestion (4.9%), breathing (2.8%) and haematological disorders (1.4%).
All cases involved medical complications, with thrombocytopenia in 84.5%, organ failure during treatment in 86%, in addition to kidney failure (mean organ failure±SD: 2.8±1.8). The most frequent were respiratory (72.5%) and cardiovascular (67.1%) failures, with 55% of patients presenting 3 or more organ failures, 37% 4 or more, and 20% 5 or more, with a mortality of 55%, 60% and 65%, respectively.
Mortality during admission to the PICU was 32.4%, with the mortality estimated by PRISM II at 20.9%.
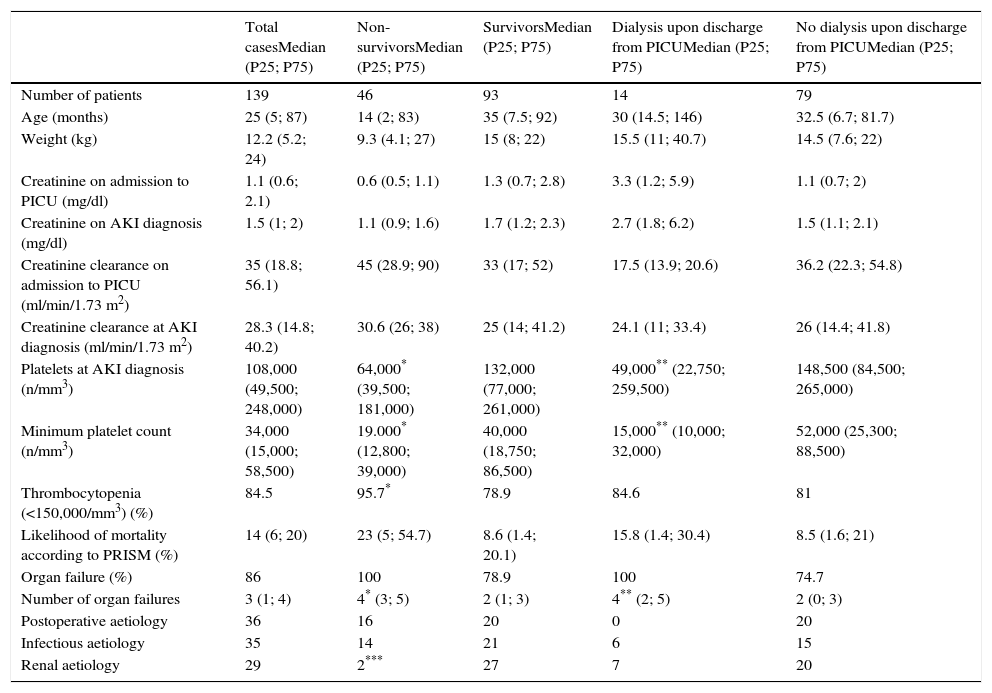
Table 1 shows the clinical and analytical characteristics of the total population, including survivors and non-survivors, and patients with or without need for dialysis on discharge from PICU, as well as mortality and need for dialysis on discharge for the 3 largest aetiological subgroups. All non-survivors and all patients needing dialysis on discharge presented some organ dysfunction, as well as a higher number of organ failures. The platelet count at AKI diagnosis and peak platelet levels were significantly lower in both non-surviivors and patients needing dialysis after discharge. The presence of thrombocytopenia (platelets<150,000/mm3) was associated with higher mortality.
Clinical and analytical characteristics of all patients: non-survivors, survivors, those requiring dialysis after PICU discharge and those that did not.
| Total casesMedian (P25; P75) | Non-survivorsMedian (P25; P75) | SurvivorsMedian (P25; P75) | Dialysis upon discharge from PICUMedian (P25; P75) | No dialysis upon discharge from PICUMedian (P25; P75) | |
|---|---|---|---|---|---|
| Number of patients | 139 | 46 | 93 | 14 | 79 |
| Age (months) | 25 (5; 87) | 14 (2; 83) | 35 (7.5; 92) | 30 (14.5; 146) | 32.5 (6.7; 81.7) |
| Weight (kg) | 12.2 (5.2; 24) | 9.3 (4.1; 27) | 15 (8; 22) | 15.5 (11; 40.7) | 14.5 (7.6; 22) |
| Creatinine on admission to PICU (mg/dl) | 1.1 (0.6; 2.1) | 0.6 (0.5; 1.1) | 1.3 (0.7; 2.8) | 3.3 (1.2; 5.9) | 1.1 (0.7; 2) |
| Creatinine on AKI diagnosis (mg/dl) | 1.5 (1; 2) | 1.1 (0.9; 1.6) | 1.7 (1.2; 2.3) | 2.7 (1.8; 6.2) | 1.5 (1.1; 2.1) |
| Creatinine clearance on admission to PICU (ml/min/1.73 m2) | 35 (18.8; 56.1) | 45 (28.9; 90) | 33 (17; 52) | 17.5 (13.9; 20.6) | 36.2 (22.3; 54.8) |
| Creatinine clearance at AKI diagnosis (ml/min/1.73 m2) | 28.3 (14.8; 40.2) | 30.6 (26; 38) | 25 (14; 41.2) | 24.1 (11; 33.4) | 26 (14.4; 41.8) |
| Platelets at AKI diagnosis (n/mm3) | 108,000 (49,500; 248,000) | 64,000* (39,500; 181,000) | 132,000 (77,000; 261,000) | 49,000** (22,750; 259,500) | 148,500 (84,500; 265,000) |
| Minimum platelet count (n/mm3) | 34,000 (15,000; 58,500) | 19.000* (12,800; 39,000) | 40,000 (18,750; 86,500) | 15,000** (10,000; 32,000) | 52,000 (25,300; 88,500) |
| Thrombocytopenia (<150,000/mm3) (%) | 84.5 | 95.7* | 78.9 | 84.6 | 81 |
| Likelihood of mortality according to PRISM (%) | 14 (6; 20) | 23 (5; 54.7) | 8.6 (1.4; 20.1) | 15.8 (1.4; 30.4) | 8.5 (1.6; 21) |
| Organ failure (%) | 86 | 100 | 78.9 | 100 | 74.7 |
| Number of organ failures | 3 (1; 4) | 4* (3; 5) | 2 (1; 3) | 4** (2; 5) | 2 (0; 3) |
| Postoperative aetiology | 36 | 16 | 20 | 0 | 20 |
| Infectious aetiology | 35 | 14 | 21 | 6 | 15 |
| Renal aetiology | 29 | 2*** | 27 | 7 | 20 |
AKI: acute kidney injury; (P25; P75): 25 percentile; 75 percentile; PICU: Paediatric Intensive Care Unit.
In 86 patients (60.1%) renal replacement therapy was needed, with peritoneal dialysis (45%) and continuous venovenous extrarenal clearance techniques (44%) being the most widely used. Among non-survivors, 60% were receiving dialysis at the time of death, while 15.1% of survivors required dialysis on discharge from the PICU.
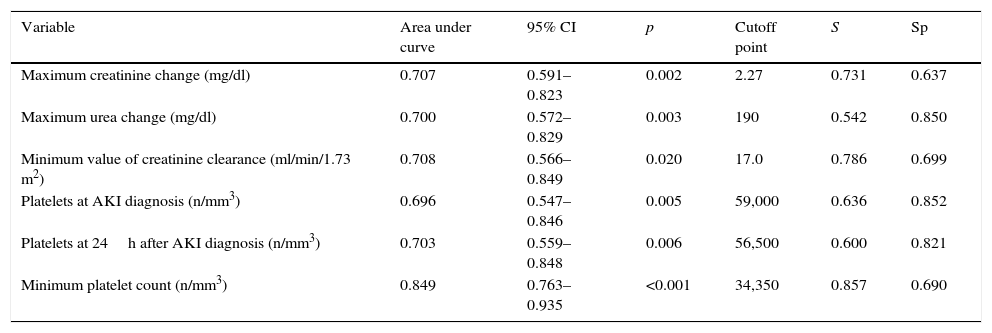
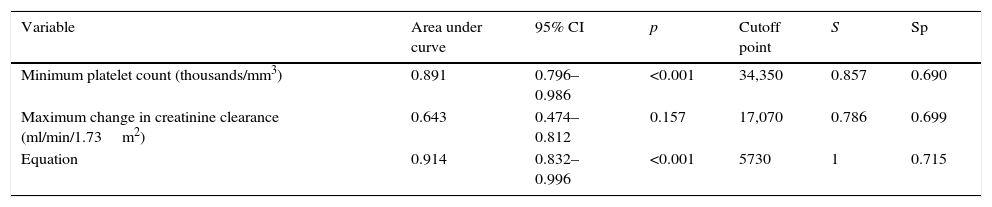
The capacity of analytical parameters to predict the need of dialysis on discharge from the PICU expressed as area under ROC curve with its respective cutoff points is shown in Table 2. The minimum platelet count was the variable with the best predictive capability.
Capacity of analytical parameters to predict need for dialysis at discharge, according to the univariate model.
| Variable | Area under curve | 95% CI | p | Cutoff point | S | Sp |
|---|---|---|---|---|---|---|
| Maximum creatinine change (mg/dl) | 0.707 | 0.591–0.823 | 0.002 | 2.27 | 0.731 | 0.637 |
| Maximum urea change (mg/dl) | 0.700 | 0.572–0.829 | 0.003 | 190 | 0.542 | 0.850 |
| Minimum value of creatinine clearance (ml/min/1.73 m2) | 0.708 | 0.566–0.849 | 0.020 | 17.0 | 0.786 | 0.699 |
| Platelets at AKI diagnosis (n/mm3) | 0.696 | 0.547–0.846 | 0.005 | 59,000 | 0.636 | 0.852 |
| Platelets at 24h after AKI diagnosis (n/mm3) | 0.703 | 0.559–0.848 | 0.006 | 56,500 | 0.600 | 0.821 |
| Minimum platelet count (n/mm3) | 0.849 | 0.763–0.935 | <0.001 | 34,350 | 0.857 | 0.690 |
Sp: specificity; AKI: acute kidney injury; CI: confidence interval; S: sensitivity.
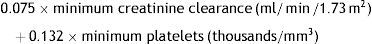
In the study of multivariate logistic regression, only the minimum platelet and creatinine clearance values remained in the final model. For every additional 1000 platelets/mm3, the risk of dialysis on discharge decreased (risk per 0.876) or, put differently, each 1000platelet/mm3 decrease multiplied the risk by 1.141 (Table 3). An equation was obtained which can predict the need for dialysis on discharge:
Table 4 shows the AUCs with their respective cutoff points.
Capacity of maximum change in platelets and creatinine clearance and the study equation to predict need for dialysis at discharge, according to the multivariate model.
| Variable | Area under curve | 95% CI | p | Cutoff point | S | Sp |
|---|---|---|---|---|---|---|
| Minimum platelet count (thousands/mm3) | 0.891 | 0.796–0.986 | <0.001 | 34,350 | 0.857 | 0.690 |
| Maximum change in creatinine clearance (ml/min/1.73m2) | 0.643 | 0.474–0.812 | 0.157 | 17,070 | 0.786 | 0.699 |
| Equation | 0.914 | 0.832–0.996 | <0.001 | 5730 | 1 | 0.715 |
Sp: specificity; Equation: 0.075×minimum creatinine clearance (ml/min/1.73m2)+0.132×minimum platelets (thousands/mm3); CI: confidence interval, S: sensitivity.
Most deaths (89%) were caused by multi-organ failure, and the mean number of organs that failed among non-survivors was 4.1±1.1.
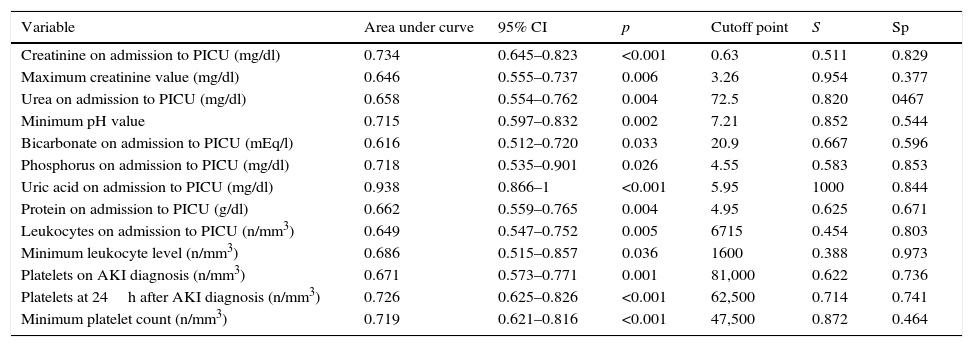
The capacity of analytical parameters to predict mortality is shown in Table 5. The value of uric acid on admission was the most relevant variable.
Capacity of analytical parameters to predict mortality, according to the univariate model.
| Variable | Area under curve | 95% CI | p | Cutoff point | S | Sp |
|---|---|---|---|---|---|---|
| Creatinine on admission to PICU (mg/dl) | 0.734 | 0.645–0.823 | <0.001 | 0.63 | 0.511 | 0.829 |
| Maximum creatinine value (mg/dl) | 0.646 | 0.555–0.737 | 0.006 | 3.26 | 0.954 | 0.377 |
| Urea on admission to PICU (mg/dl) | 0.658 | 0.554–0.762 | 0.004 | 72.5 | 0.820 | 0467 |
| Minimum pH value | 0.715 | 0.597–0.832 | 0.002 | 7.21 | 0.852 | 0.544 |
| Bicarbonate on admission to PICU (mEq/l) | 0.616 | 0.512–0.720 | 0.033 | 20.9 | 0.667 | 0.596 |
| Phosphorus on admission to PICU (mg/dl) | 0.718 | 0.535–0.901 | 0.026 | 4.55 | 0.583 | 0.853 |
| Uric acid on admission to PICU (mg/dl) | 0.938 | 0.866–1 | <0.001 | 5.95 | 1000 | 0.844 |
| Protein on admission to PICU (g/dl) | 0.662 | 0.559–0.765 | 0.004 | 4.95 | 0.625 | 0.671 |
| Leukocytes on admission to PICU (n/mm3) | 0.649 | 0.547–0.752 | 0.005 | 6715 | 0.454 | 0.803 |
| Minimum leukocyte level (n/mm3) | 0.686 | 0.515–0.857 | 0.036 | 1600 | 0.388 | 0.973 |
| Platelets on AKI diagnosis (n/mm3) | 0.671 | 0.573–0.771 | 0.001 | 81,000 | 0.622 | 0.736 |
| Platelets at 24h after AKI diagnosis (n/mm3) | 0.726 | 0.625–0.826 | <0.001 | 62,500 | 0.714 | 0.741 |
| Minimum platelet count (n/mm3) | 0.719 | 0.621–0.816 | <0.001 | 47,500 | 0.872 | 0.464 |
Sp: specificity; AKI: acute kidney injury; CI: confidence interval; S: sensitivity; PICU: Paediatric Intensive Care Unit.
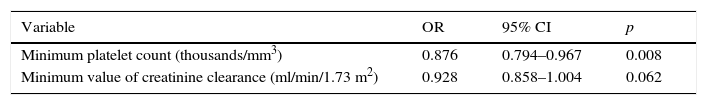
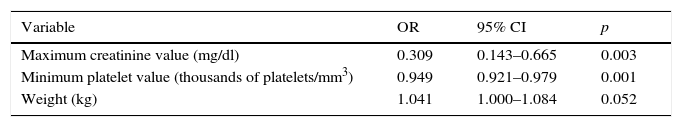
In the multivariate logistic regression study, the minimum platelet value, the maximum creatinine value, and the weight remained in the final model (Table 6). Both the platelet and creatinine values acted as factors protecting against mortality, so that for each additional 1mg/dl of creatinine the risk of death was reduced by 0.309, and for each additional 1000platelets/mm3 the risk was reduced by 0.949.
Multivariate analysis for mortality. Lower in creatinine and platelet values are associated with a higher risk of mortality.
| Variable | OR | 95% CI | p |
|---|---|---|---|
| Maximum creatinine value (mg/dl) | 0.309 | 0.143–0.665 | 0.003 |
| Minimum platelet value (thousands of platelets/mm3) | 0.949 | 0.921–0.979 | 0.001 |
| Weight (kg) | 1.041 | 1.000–1.084 | 0.052 |
CI: confidence interval; OR: odds ratio.
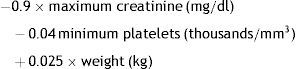
The equation obtained to predict mortality during admission was:
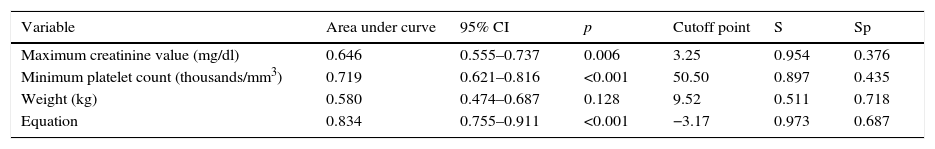
Weight is a minor factor in the equation, but a more significant factor in the univariate analysis. In the equation, greater weight slightly increases the risk of death, whereas in the univariate analysis the opposite occurred. The cutoff point for this equation is negative, with a value of −3.17, so that values below this point predict survival and values above this point predict mortality. Table 7 shows the AUCs with their respective cutoff points.
Capacity of maximum change in platelets and creatinine clearance, weight, and the study equation to predict mortality, according to the multivariate model. Lower creatinine and platelet values are associated with higher risk of mortality.
| Variable | Area under curve | 95% CI | p | Cutoff point | S | Sp |
|---|---|---|---|---|---|---|
| Maximum creatinine value (mg/dl) | 0.646 | 0.555–0.737 | 0.006 | 3.25 | 0.954 | 0.376 |
| Minimum platelet count (thousands/mm3) | 0.719 | 0.621–0.816 | <0.001 | 50.50 | 0.897 | 0.435 |
| Weight (kg) | 0.580 | 0.474–0.687 | 0.128 | 9.52 | 0.511 | 0.718 |
| Equation | 0.834 | 0.755–0.911 | <0.001 | −3.17 | 0.973 | 0.687 |
Sp: specificity; Equation: −0.9×maximum creatinine (mg/dl)−0.04×minimum platelets (thousands/mm3)+0.025×weight (kg); CI: confidence interval; S: sensitivity.
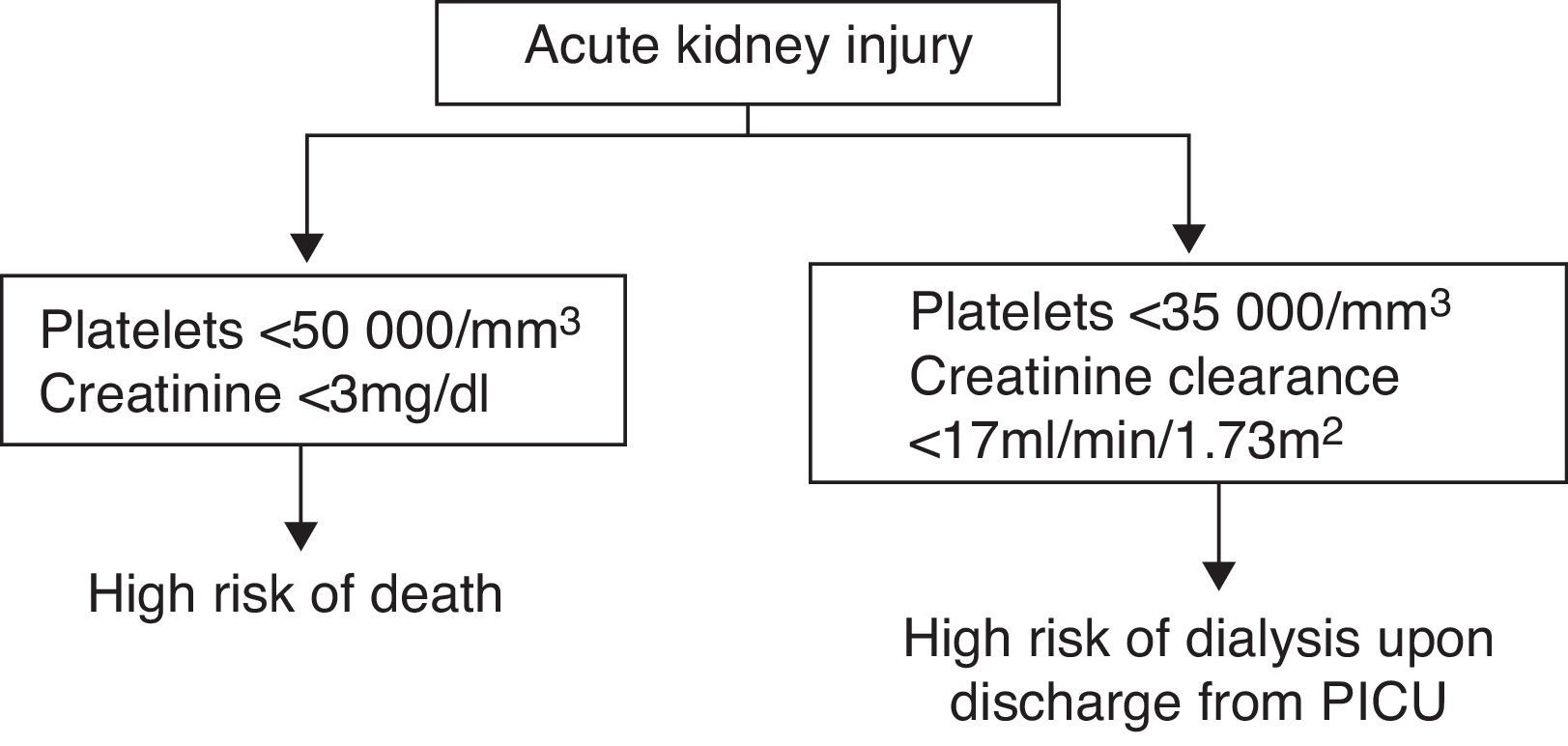
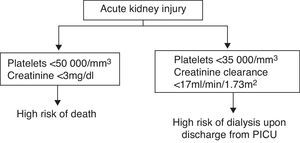
As the equations created might not be of practical use in clinical practice, a simple algorithm was devised to indicate which patients have a high risk of mortality or need for dialysis on discharge from the PICU (Fig. 1).
DiscussionThe incidence of AKI in childhood is still unclear, since each study has included different types of patients and used different diagnostic criteria.15 AKI incidence is greater among newborns. Between 3.4 and 24% develop AKI.16,17 A prospective study with critical paediatric patients, including non-premature newborns older than 3 days, reported an AKI incidence of 4.5%, which is more than twice that of our study, probably due to the inclusion of patients younger than one week of age.1
The epidemiology of AKI has changed due to therapeutic advances and a growing trend to present secondary to other pathologies.10,18–21 In our study, the most frequent aetiologies were heart surgery, septic processes and nephrologic causes.
Patients undergoing additional surgery are at high risk of AKI.22–24 Severe sepsis and septic shock are risk factors for AKI. However, studies report a lower percentage of AKI secondary to sepsis than that found in our study.10,18,25
With regard to nephrologic causes, our results show that the haemolytic uraemic syndrome, even though infrequent in Spain,26 is a major cause of AKI.25,27,28
AKI significantly increases the morbidity and mortality of critically ill patients.10,15 Paediatric AKI is almost always present in the context of organ failure.19 In our study, 86% of patients presented some organ failure other than kidney failure during treatment, with an average of almost 3 dysfunctions per patient.
A large proportion of children presenting AKI recover kidney function during their stay in the PICU. In our study, 15% of survivors required dialysis on discharge from the PICU, although the development of kidney function in the long term was not analysed. We have not found any studies analysing the risk factors for need for dialysis on discharge from the PICU, and only some studies in adults have investigated the predictive factors for kidney recovery among critically ill patients with AKI.29 Our results show that thrombocytopenia was a good predictor of poor evolution of AKI, whereas a major decrease in creatinine clearance was not an independent predictor, but was valuable as part of an equation in which both variables were present. From the data from our sample, 100% of patients with values above the cutoff point of the equation will not need dialysis on discharge from the PICU (Table 4).
Mortality was 32.4%, similar to the 27% and 32% reported in other prospective studies in critically ill children.2,10 These values are lower than those reported in adult Intensive Care Units.30,31 In other paediatric studies, most non-survivors were found to present a severe underlying condition32,33 and a relationship between multi-organ failure and mortality,19,30 which is consistent with our findings.
A finding of interest is that the probability of death calculated with PRISM II undervalued the actual risk of death. This scenario has already been described in several studies.34,35 A more recent prospective work showed that clinical severity scales (PRISM, PIM and PELOD) undervalued mortality in children treated with continuous techniques. Of these 3, PRISM had the highest predictive value.
Analysing the capacity of analytical parameters to predict mortality showed that serum uric acid at admission was the most relevant parameter in the univariate analysis. However, it did not remain a mortality risk in the multivariate analysis, leading us to believe that its predictive capacity depends on other factors.
In the multivariate study, the minimum value of platelets, the maximum change in creatinine, and patient weight remained in the final model, although the latter was of minor importance. The equation was highly predictive of mortality, with a sensitivity of 97% and a specificity of 67%. Our results show that thrombocytopenia was a good predictor of mortality, whereas higher values of creatinine were associated with a greater survival rate. The association of higher creatinine values with a better prognosis reinforces the theory that AKI mortality among children is not related to kidney failure itself, but mainly to the triggering cause and the existence of multi-organ failure.27,28,33 Thus, low mortality rates are observed in isolated AKI without organ failure where the creatinine value may be very high. Conversely, mortality increases when AKI, even with not too high creatinine values, occurs in the context of multiple organ failure.21 This fact coincides with the results of studies among critical children treated with extrarenal clearance techniques.3 In support of this hypothesis, in our study mortality is lower in cases of renal aetiology (Table 1). In contrast, other studies in critically ill children have found a relationship between increased creatinine and higher severity on the RIFLE scale, based on serum creatinine values, with mortality.9,36
In our sample, thrombocytopenia was the most important risk factor for poor prognosis. Most studies have analysed the impact on prognosis of values below 150,000–100,000platelets/mm3. Others stress the diagnostic relevance of the relative decrease of platelets.37 Thrombocytopenia has been described as the main risk factor for the development of AKI among children.1
There are several limitations to our study: the definition used for AKI did not originally include the pRIFLE criteria, since at the time the study was designed the criteria had not yet been published. We have retrospectively classified our patients following the pRIFLE criteria, based on the maximum values of blood creatinine. Most patients were classified in the Failure group, although the criteria based on oliguria or anuria was not considered.
The second limitation is that a significant period has elapsed between data collection and processing and publication. This leads us to consider the study conclusions with more caution when applying them to the current situation. Recently, the publication of studies where data collection, as in our case, occurred 10 years before publication has been defended.38 Factors such as difficulties involved in gathering and analysing data in multi-centre studies, changes in professional, teaching and investigative responsibilities of authors, or failure to agree on the text of the article justify the delay in publication. Investigators have a responsibility to publish the results of studies quickly, but when external circumstances delay publication, we must make the necessary efforts for data to be finally published.
The third limitation is the improvement which has taken place in creatinine measurement techniques, resulting in lower values than some years ago, and, consequently, the calculation formulas of creatinine clearance have changed.39,40
Lastly, our study has only analysed the evolution of AKI during the stay at the PICU. It is important to conduct studies analysing whether a recovery or deterioration of kidney function occurs after discharge from the PICU.
Our research constitutes one of the biggest prospective studies conducted so far on AKI in critically ill children with the participation of a significant number of Spanish PICUs, so its results are representative of the reality in our country at the time of the study. This data is a good starting point to undertake comparative studies over time on AKI in critically ill children.
To conclude, our results confirm the existence of high morbidity and mortality in critically ill children with AKI. Platelet count and creatinine clearance values were good predictors of the need for dialysis on discharge from the PICU. Platelet count and serum creatinine were mortality markers in paediatric AKI.
Conflict of interestThe authors state there is no conflict of interest.
We would like to thank all the medical and nursing personnel of the various PICUs participating in the study, for their invaluable collaboration with data collection.
Grupo de Estudio del Fallo Renal Agudo de la Sociedad Española de Cuidados Intensivos Pediátricos: María Carmen Martínez Ferriz, Montserrat Antón Gamero, Jesús López-Herce Cid, Cinta Téllez González, Yolanda López Fernández, José Alberto Medina Villanueva, María del Pilar Azcón González de Aguilar, José Luis Vázquez Martínez, Joseba Landa Maya, Federico Martinón Torres, Martí Pons Odena, Miguel Herrera, Amelia Martínez de Azagra, José Domingo López Castilla, Juan A. García Hernández, Manuel González Ripoll, Antonio Gómez Calzado, Esther Ocete Hita, Angel Hernández Borges, Teresa Gili Bigata.
Please cite this article as: Pol PT, Galán CR, Villanueva JAM, Martinez-Camblor P, López-Herce J, en representación del Grupo de Estudio del Fallo Renal Agudo de la Sociedad Española de Cuidados Intensivos Pediátricos. Daño renal agudo grave en niños críticos: epidemiología y factores pronósticos. An Pediatr (Barc). 2015;83:367–375.
Los miembros del Grupo de Estudio del Fallo Renal Agudo de la Sociedad Española de Cuidados Intensivos Pediátricos se presentan en el Appendix A.