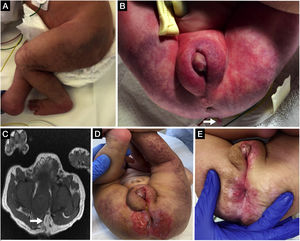
A newborn aged 18 h with normal prenatal ultrasound scans and a history of maternal gestational diabetes and preeclampsia was referred for assessment of an extensive “vascular lesion”. The patient had labioscrotal folds containing testes and a micropenis with interscrotal hypospadias. The anus was displaced anteriorly and mildly stenotic, but surrounded by sphincter tissue. Vascular anomalies were present in the lower extremities, perineum and lumbosacral region, which was compatible with segmental haemangioma (Fig. 1A), in addition to a lumbosacral skin tag (Fig. 1B). The suspicion of LUMBAR syndrome was confirmed by magnetic resonance imaging, which showed a tethered cord, lipomyeloschisis and hydrosyringomyelia (Fig. 1C). The perineal haemangioma ulcerated at 1 month post birth and required treatment with propranolol (Fig. 1D), with a favourable response (Fig. 1E).
Segmental infantile haemangioma in the perineal and lumbosacral regions extending to the lower extremities (A) and lumbosacral skin tag (B, arrow). Magnetic resonance image evincing the presence of lipomyeloschisis (C, arrow). Ulcerated perineal haemangioma (D) that responded well to treatment with propranolol (E).
Infantile haemangiomas are the most common benign vascular tumours in children (2%–10%) and usually present as isolated cutaneous lesions, although they may occur in the context of different syndromes.1 The acronym LUMBAR refers to the presence of segmental infantile haemangioma in the lower body associated with other cutaneous defects, urogenital anomalies, myelopathy, bone deformities, anorectal malformations and renal and arterial anomalies.2
The detection of segmental haemangiomas or haemangiomas larger than 2.5 cm in the lower body requires differential diagnosis with spinal cord, genitourinary and anorectal anomalies to prevent irreversible sequelae and ensure appropriate multidisciplinary management.3