A retrospective study was conducted in the Neonatal Intensive Care Unit of a tertiary hospital to determine the incidence of early hyponatraemia (first 48h of life) in preterm infants. Risk and protection factors in this condition were also examined as a starting point for a change in the medical action when prescribing intravenous fluids.
Material and methodsThe study included a sample of 256 premature babies (gestational age: 235–366) admitted to the Neonatal Intensive Care Unit of a tertiary hospital between January 2016 and June 2018. The number of patients receiving intravenous sodium in different intervals during the first 48h of life was determined, as well as the number of those with hyponatraemia of any type (<135mmol/l), and moderate-severe (<130mmol/l). An analysis was made of the relationship between early hyponatraemia and weight/gestational age, antenatal steroids exposure, respiratory pathology, early sepsis, and perinatal asphyxia.
ResultsHyponatraemia occurred in 81 patients, 31.64% of the total (up to 50% in <30 weeks of gestational age), and was moderate-severe (<130mmol/l) in 17.3% of the cases. The period of time with the most cases of hyponatraemia was in the first 12h of life (22.64%). Weight (P=.034), gestational age (P<.001) and respiratory disease (P<.001) were found to be risk factors and, in a multivariate analysis, the latter was independently related to early hyponatremia (P<.01, OR=5.24, 95% CI: 2.79–9.84). Antenatal betamethasone exposure did not show to be a protection factor.
ConclusionAccording to the results of this study, it is considered an advantage to provide sodium in the intravenous fluids prescribed during the first days of life, particularly in preterm infants of lower gestational age and with respiratory disease involvement.
Estudio retrospectivo en la unidad de cuidados intensivos neonatales de un hospital de tercer nivel sobre la incidencia de hiponatremia precoz (primeras 48horas de vida) en prematuros. Buscamos factores de riesgo y de protección para esa alteración, como punto de partida para un cambio en la actuación médica al prescribir fluidos intravenosos.
Material y métodosMuestra de 256 prematuros (edad gestacional: 235-366) ingresados en la unidad de cuidados intensivos neonatales de nuestro hospital, entre enero de 2016 y junio de 2018. Se determinó qué pacientes recibieron aportes intravenosos de sodio en distintos intervalos de las primeras 48horas de vida y cuántos padecieron hiponatremia de cualquier tipo (<135mmol/l) y moderada-grave (<130mmol/l). Se estudió la relación entre hiponatremia precoz y peso/edad gestacional, administración de corticoides prenatales, enfermedad respiratoria, sepsis precoz y asfixia perinatal.
ResultadosPadecieron hiponatremia 81 pacientes, 31,64% del total (hasta un 50% en <30 semanas de edad gestacional), siendo moderada-grave (<130mmol/l) en un 17,3% de los casos. El periodo de tiempo con más casos de hiponatremia fue el de las primeras 12horas de vida (22,64%). Demostraron ser factores de riesgo el peso (p=0,034), la edad gestacional (p<0,001) y el padecimiento de enfermedad respiratoria (p<0,001) y, en el análisis multivariable, este último se mostró relacionado de forma independiente con la hiponatremia precoz (p<0,01; OR=5,24; IC 95%: 2,79-9,84). La administración de betametasona prenatal no demostró proteger.
ConclusiónSegún nuestros resultados creemos conveniente aportar sodio en los fluidos intravenosos prescritos los primeros días de vida, particularmente en prematuros de menos edad gestacional y en afectos de enfermedad respiratoria.
In recent years, emphasis has been placed on the importance of ensuring an adequate sodium (Na) intake in preterm newborns, especially from week 2 post birth, to prevent late-onset hyponatraemia.1,2 Recent guidelines have also started to recommend the addition of sodium to the intravenous fluids administered to hospitalised newborns in the first days of life, especially preterm newborns,3,4 with the aim of maintaining serum sodium levels within the normal range (135–145mmol/l). At present, there is widespread consensus that sodium supplementation in preterm infants starting from week 2 post birth as needed to achieve adequate serum levels is associated with an adequate growth velocity and weight gain and improved cognitive outcomes.2,4,5 It is also generally acknowledged that it is important to maintain an adequate sodium serum level in the first few days of life,2 as this is the main determinant of blood osmolality and, given the particularities of homeostasis in newborns, especially those born preterm.6,7 While most neonatologists agree on restricting water intake in the first 2 days of life to allow a reduction in the extracellular fluid, there is less agreement when it comes to the administration of sodium in this early stage of transition to extrauterine life. Fluid restriction alone may suffice to maintain normal sodium levels, but preterm newborns, due to their particular physiology (accelerated renal maturation with abnormal glomerular morphology,8 poor response to aldosterone6,9 and ADH6 and elevation of natriuretic peptides6,10), eliminate larger amounts of sodium in the urine compared to term infants, and therefore serum levels of sodium can drop below the normal range. Despite recent recommendations,2,3 in everyday practice many neonatal units seldom add sodium to the intravenous fluids prepared for preterm newborns in days 1 and 2 post birth. Oral intake, which is small or non-existent, also fails to contribute to achieving the recommended intake. The aim of our study was to identify the risk factors for early-onset hyponatraemia in newborns delivered before 37 weeks’ gestation so that they can be taken into account when it comes to planning supplementation with this electrolyte. The ultimate goal of the study was to shift our everyday practice in the prescription of intravenous fluid therapy, which is needed by many of the patients in neonatal units, especially those with lower weight and gestational age.
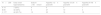
Material and methodsWe conducted a retrospective observational study in the neonatal unit of our hospital between January 2016 and June 2018. Having obtained the approval of the clinical research ethics committee of our hospital, and adhering to institutional regulations regarding access to health records and to current law on personal data protection, we reviewed the records of 263 preterm newborns hospitalised during the study period: every newborn delivered before 36 weeks’ gestation and newborns delivered between weeks 360 and 37 of gestation if they had any morbidity. We excluded newborns transferred from other hospitals, those whose records lacked laboratory data or in who testing had been performed in different laboratory, and those that died within 2 days of birth. The final sample included 256 patients delivered between 235 and 366 weeks’ gestation, which we divided into 3 groups: A (<300 weeks gestational age), B (300–336 weeks) and C (340–366 weeks). Table 1 summarises the demographic characteristics of the sample and the use of antenatal corticosteroid therapy (betamethasone) for lung maturation. The initial volumes of fluids and electrolytes administered to these patients adhered to the recommendations of the Sociedad Española de Neonatología (Spanish Society of Neonatology).11 In brief, newborns were given 60–70cc/kg/day in days 1 and 2 of life, although in preterm newborns, especially those delivered before 30 weeks’ gestation, the dose on day 2 could be higher (80–100cc/kg); when it came to sodium supplementation, save to correct an inadequate serum level, preterm newborns were not given intravenous sodium on day 1 of life, and those receiving intravenous fluids (for fluid replacement or parenteral nutrition) were given 1–2mEq/kg starting from day 2. Table 1 also shows the percentage of patients given intravenous sodium in the first 12h, between 13 and 24h and between 25 and 48h post birth.
Demographic data, absolute frequency and percentage of patients treated with antenatal betamethasone and absolute frequency and percentage of patients that received intravenous sodium supplementation in each of the 3 time intervals.
| Total sample=256 | Group A (<30 w): 14 | Group B (30–336 w): 65 | Group C (340–366 w): 177 |
|---|---|---|---|
| Weight, mean±SD (g) | 1072±283.5 | 1794.9±364.8 | 2287.14±387.7 |
| Sex (M/F) | 10/4 | 33/32 | 96/81 |
| Antenatal betamethasone | 11 (78.6%) | 53 (81.53%) | 55 (31.07%) |
| Caesarean/vaginal birth | 13/1 | 51/14 | 84/93 |
| Na supplementation first 12h post birth | 5 (35.7%) | 11 (16.9%) | 8 (4.5%) |
| Na supplementation 13–24h post birth | 11 (78.6%) | 25 (38.5%) | 14 (7.9%) |
| Na supplementation 25–48h post birth | 14 (100%) | 41 (63.1%) | 23 (13%) |
| % weight loss, mean±SD | 10.07%±2.9 | 9.19%±4.3 | 6.2%±2.7 |
F, female; M, male; SD, standard deviation; w, weeks of gestational age.
We determined the incidence of hyponatraemia (Na<135 mmol/l) and/or moderate-to-severe hyponatremia (Na<130mmol/l) in these 3 time intervals in the 3 gestational age groups under study. We analysed the association of early-onset hyponatraemia with gestational age, birth weight, delivery of antenatal corticosteroid therapy, presence of respiratory disease (type I respiratory failure, transient tachypnoea, pulmonary air leak or pulmonary haemorrhage) and other perinatal diseases such as perinatal asphyxia or early-onset sepsis.
Statistical analysisWe summarised qualitative variables as frequency and percentage distributions, and quantitative variables as mean and standard deviation in case of a normal distribution and otherwise as median and interquartile range.
We analysed the association between continuous and qualitative variables using the Student t test for independent samples after assessing the homogeneity of variance with the Levene test if the variables were normally distributed, and otherwise using the Mann–Whitney U test.
We analysed the association between qualitative variables using the chi square test or the Fisher exact test as applicable.
Lastly, following the univariate analysis of potential variables and risk factors at play in the development of hyponatraemia, we performed a multivariate logistic regression analysis with the significant factors to assess the influence of each of the factors in the overall situation.
We performed all the analyses with the software SPSS Statistics version 24, and set an alpha level of significance of 0.05 for all tests.
ResultsDescriptive analysisAs can be seen in Table 1, group A (≤30 weeks) had 14 patients, group B (300–336 weeks) 65 and group C (340–366 weeks) 177. Overall, 9.3% of the sample received sodium supplementation in the first 12h post birth (group A, 35.7%; group B, 17%; group C, 4.5%); 19.5% received sodium between 13 and 24h post birth (group A, 78.6%; group B, 33.5%; group C, 8%) and 30.4% received it from day 2 of life (group A, 100%; group B, 63.1%; group C, 13%).
Hyponatraemia (serum sodium <135mmol/l) was documented in 81 patients, or 31.64% of the sample (group A, 50%; group B, 49%; group C, 23.7%) and was moderate to severe (<130mmol/l) in 17.3% of cases: 4 patients in group A, 5 in group B and 12 in group C (Table 2).
Incidence of early-onset hyponatremia (<48h post birth) in the 3 gestational age groups and different time intervals. A: <30 w; B 300–336 w; C 340–366 w.
| N=256 | Early onset hyponatraemia | Sodium <130mmol/l | HypoNa <12h post birth | HypoNa 12–24h post birth | HypoNa 24–48h post birth |
|---|---|---|---|---|---|
| A 14 | 7 (50%) | 4 | 6 | 5 | 1 |
| B 65 | 32 (49%) | 5 | 27 | 10 | 4 |
| C 177 | 42 (23.7%) | 12 | 23 | 18 | 16 |
The time interval with the highest incidence of hyponatraemia was the first 12h post birth (22.64% in preterm newborns). In this interval, only 9.3% of the sample received intravenous sodium, although this percentage rose to 35.7% when it came to newborns delivered before 30 weeks’ gestation (Tables 1 and 2). We ought to highlight that 32 preterm newborns (12.5%) had sodium levels below normal in the first 3h post birth. We reviewed the health records of the mothers of these 32 patients to try to find data on the sodium serum levels before delivery, but they had not been documented in any case.
Only 2 patients in the sample developed hypernatraemia (maximum, 148mmol/l), in both cases between 24 and 48h post birth.
A total of 102 patients had respiratory problems (group A, 13 [92.8%]; group B: 47 [72.3%]; group C, 43 [27.7%]) (Table 3). Table 3 presents the distribution by respiratory problem. Of these patients, 52 (69.1% of the total) had hyponatremia.
Distribution of patients by gestational age and respiratory illness, presence of early-onset sepsis and perinatal asphyxia.
| Group A=14 | Group B=65 | Group C=167 | |
|---|---|---|---|
| Respiratory distress | 13 (92.8%) | 47 (72.3%) | 43 (25.74%) |
| ARDS | 9 | 30 | 7 |
| Transient tachypnoea | 4 | 21 | 36 |
| Air leak | 1 | 3 | 5 |
| Pulmonary haemorrhage | 2 | 0 | 0 |
| Early-onset sepsis | 3 (21.4%) | 4 (5.3%) | 0 (0%) |
| Perinatal asphyxia | 0 (0%) | 1 (1.3%) | 3 (1.8%) |
ARDS, acute respiratory distress syndrome; w, weeks of gestational age.
Seven patients received a diagnosis of early-onset sepsis (Table 3): 3 (21.4%) in group A, 4 (5.3%) in group B and 0 in group C. Three of them had early-onset hyponatraemia.
As for the diagnosis of perinatal asphyxia (Table 3), there were 0 cases in group A, 1 case (1.3%) in group B and 3 cases (1.8%) in group C. All of these patients had early-onset hyponatraemia.
Risk factorsWe assessed the association of early-onset hyponatraemia with the following factors (Table 4):
Risk factors for early-onset hyponatraemia in preterm newborns.
| Univariate analysisP, OR (CI) | Multivariate analysisP, OR (CI) | |
|---|---|---|
| Gestational age | P<.001 | |
| Birth weight | P=.034 | |
| No antenatal corticosteroids | P=.072 | |
| Respiratory distress | P<.001; 6.2 (3.5–11.0) | P<.01; 5.24 (2.79–9.84) |
| Early-onset sepsis | P=.683 | |
| Perinatal asphyxia | Not applicable |
CI, confidence interval; OR, odds ratio.
Gestational age. Patients with early-onset hyponatraemia had a lower gestational age compared to patients that did not develop it (P<.01).
Weight. Preterm infants with early-onset hyponatraemia had lower weights compared to those that did not develop it (1967 g vs 2135.9g) (P=.034).
Antenatal corticosteroid therapy. We did not find an association between non-administration of antenatal corticosteroid therapy and hyponatraemia (P=.072). Taking into account that antenatal corticosteroid therapy was more frequent in preterm newborns with lower gestational ages, we did a stratified analysis by gestational age group and also found no association.
Respiratory distress. We found a strong association between the presence of respiratory distress and early-onset hyponatraemia (P<.01).
Early-onset sepsis: we did not find an association (P=.683).
Perinatal asphyxia: all patients with perinatal asphyxia had early-onset hyponatraemia, and the asphyxia was moderate to severe in 3 out of these 4 patients.
Considering that respiratory distress in preterm newborns is strongly associated with a lower gestational age, we used multivariate analysis to assess which of the 2 risk factors (respiratory distress or gestational age) bore more weight in the incidence of early-onset hyponatraemia. We found that respiratory distress was most strongly associated with hyponatraemia independently of gestational age (P<.01), with an odds ratio of 5.24 (95% confidence interval, 2.79–9.84).
When we analysed the association between the detection of hyponatraemia and intravenous sodium administration, we found a statistically significant result. In other words, patients with low sodium serum levels received sodium supplementation more frequently in the first 48h post birth. This was the case in every gestational age group and every time interval under study, and the difference was always statistically significant (P<.001).
DiscussionOur study revealed that early-onset hyponatraemia (first 48h post birth) occurred in as many as 50% of preterm newborns with the lowest gestational ages and birth weights, and that it was moderate to severe in up to 28.6% of this group of most vulnerable patients. Although it is well known that in the first 2 days of life there is an acute contraction of the extracellular compartment that manifests with diuresis and results in a weight loss of 7%–10%, the physiological process is more complex in preterm newborns, in who from the very first hours of life, in addition to very high insensible water losses through a poorly keratinised stratum corneum, diuresis and natriuresis can be significantly greater from birth compared to term newborns.9,12,13 Thus, the excretion of sodium in the urine in extremely preterm newborns can occur as early as the first 2 days of life reaching levels of up to 5.75mEq/1.73m2, or a fractional excretion of sodium (FENa) of up to 12.5%.4,12 There are several reasons for this particular pattern in the sodium homeostasis in preterm newborns: renal immaturity affecting reabsorption in the distal tubules, high concentrations of aldosterone but a poor response to it and high levels of natriuretic peptides. For all these reasons, despite the general recommendation of restricting the volume of administered fluid, it may be necessary to administer more water in the solutions used for fluid replacement or parenteral nutrition and to add sodium to these solutions. In older, critically ill infants there is a tendency to avoid use of hypotonic saline solutions to prevent syndrome of inappropriate ADH secretion (SIADH), which is a frequent problem in this population. In newborns, taking into account the stages of physiological maturation in fluid management, it had been common practice until recently to refrain from adding sodium during the stage known as transition to extrauterine life, whose end is marked by the maximum weight loss or at least 2 days post birth. By reviewing health records, we wanted to emphasise that in preterm newborns, the lower the gestational age and the weight, the more important it is to consider that fluid restriction in the first day of life may not be advisable and that the usual fluid volume may not suffice to maintain sodium serum levels in the normal range. In recent years, the European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) and other authors have recommended supplementation with sodium of intravenous fluids from the first days of life (with addition of up to 3mEq/kg of sodium in preterm newborns with very low birth weight or delivered before 28 weeks’ gestation).3,4 However, this approach has not yet become widespread and many authors still recommend against sodium supplementation until the weight loss peaks.12 A protocol for a future Cochrane review has been developed to determine the outcomes of supplementation with different doses of sodium in the first few weeks of life.13
The aim of our study was to identify the risk factors associated most strongly with early-onset hyponatraemia. We found 3 main factors: gestational age and weight, both inversely associated with the probability of having hyponatraemia in the first 48h post birth, and respiratory distress, which exhibited a direct association. Since respiratory problems are strongly associated with gestational age, we did a multivariate analysis that showed that respiratory illness was the strongest independent risk factor for early-onset hyponatraemia.
In our sample, other potentially relevant factors, such as neonatal sepsis, were not associated with an increased risk, although due to the low number of patients with early-onset sepsis, we could not evaluate this factor with sufficient power. On the other hand, perinatal asphyxia, in every case with hypoxic-ischaemic encephalopathy of at least moderate severity, was significantly associated with the development of moderate to severe hyponatraemia: the 4 preterm newborns that developed it had sodium levels of less than 130mmol/l. Hypoxic-ischaemic encephalopathy usually manifests with SIADH and therefore with this electrolyte imbalance.14,15 As was the case of sepsis, so few patients were affected by perinatal asphyxia that we were unable to obtain statistically significant results.
The administration of betamethasone to pregnant women with the goal of accelerating lung maturation also has an effect on skin maturation, reducing excessive transcutaneous fluid loss, and in renal maturation, inducing an increase in diuresis and a reducing sodium excretion in the urine.7,16 Therefore, this antenatal corticosteroid therapy has been proposed as a prophylactic measure to protect against hyponatraemia in preterm infants. We did not observe this effect in our study.
On the other hand, as a secondary outcome, we found that patients that developed hyponatraemia were the patient that most frequently received intravenous sodium supplementation (Tables 1 and 2). Thus, in the group with lower gestational age, 35.7% of patients (n=5) received sodium in the first 12h of life and up to 50% had hyponatraemia in this period. Of the 5 patients that received sodium supplementation, only 1 received it before developing hyponatraemia, while in the rest of cases supplementation was used as a corrective measure. We observed the same pattern in all other groups: patients did not receive prophylactic supplementation but were given sodium as treatment for low serum levels.
When it came to the time interval with the highest incidence of hyponatraemia, we found that it corresponded to the first 12h post birth, which can be attributed to the very infrequent delivery of sodium during this interval, compared to subsequent intervals in which it was administered to correct deficient levels. We ought to highlight that in the first 3h post birth, when the internal milieu of the newborn is most similar to that of the mother, up to 12.5% of the sample (32 preterm newborns) had sodium levels below the normal range: 2/3 of these newborns had been delivered before 34 weeks’ gestation and 65% had respiratory distress. It is possible that the mothers of these patients had hyponatraemia due to pregnancy complications or disease and/or their fluid and electrolyte intake, but the retrospective design of our study did not allow us to establish the cause, despite our review of maternal obstetric records.
We were unable to analyse the potential association of sodium serum levels and weight loss in the first 48h post birth, since the severity of illness in extremely preterm patients made daily and reliable weighing unfeasible in many of them. However, the maximum weight loss by the end of the transition period (4–5 days post birth) was within the normal range (Table 1). Although the deleterious impact of late-onset hyponatraemia on weight in preterm infants is a known fact, this was not the subject of our study, as we limited our analysis to the first 2 days of life.
We want to emphasise the importance of appropriately adjusting the administration of fluids not only in terms of total volume, but also in terms of osmolarity, mainly to be determined by the amount of sodium. As occurs in other stages of life, respiratory illness can lead to the development of hyponatraemia, which in some cases can result in cytotoxic cellular oedema due to hypoosmolality.6,16 These cases are managed not only by restricting fluids, but also with administration of fluids with a higher sodium content. The involved mechanisms may be different in preterm newborns due to the immaturity of the kidneys, the poor response to ADH and the excessive natriuresis, but the outcome is similar. It is very important to assess the fluid and electrolyte balance frequently, several times a day, to make the appropriate adjustments to the intravenous fluids delivered in the first days of life.
Despite the limitations of a retrospective study, it is reasonable to conclude that in the population of preterm newborns, especially extremely and moderate preterm, sodium should be included at a dose of at least 1–3mEq/kg in the intravenous fluids or parenteral nutrition solutions from the first hours of life, as recommended by Bischoff et al. and Jochum et al. (ESPGHAN/ESPEN/ESPR Guidelines).3,4 This is particularly the case in patient with respiratory morbidity.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Pérez-Piaya Moreno MR, Miranda Alcalde B, Cárdenas Rebollo JM, Riaza Gómez M, Carnicer H, Romera Modamio G. Factores de riesgo para el desarrollo de hiponatremia precoz en el prematuro. Revisión de nuestra práctica en administración de sodio en los primeros días de vida. An Pediatr (Barc). 2020;92:359–364.