The creation of paediatric palliative care units (PPCU) could optimise the management of children with palliative focus after admission to a paediatric intensive care unit (PICU). This study describes the clinical and epidemiological characteristics of children referred from PICU to the PPCU of the Autonomous Community of Madrid (CAM). The overall treatment, relapses, re-admissions, and deaths, if occurred, are described.
Patients and methodA retrospective review was performed using the medical records from children transferred from the CAM paediatric intensive care units to the paediatric palliative care unit (1 March 2008–31 January 2015).
ResultsA total of 41 patients were included (26 male/15 female) with a median age of 33 months (range 1–228). In the follow by the PPCU follow-up, the main approaches were respiratory (invasive ventilation with tracheostomy tube 8/41), nutritional (gastrostomy in 20/41), and pharmacological (anti-epileptics in 29/41 and 34/41 on antibiotic treatment). Hospital re-admission was required by 11/41 patients, with no re-admissions to PICU. Of the 13/41 patients who died, 9/13 were at home, with all of them accompanied by the primary caregivers and family, and only 1/9 with the presence of the home team.
ConclusionsThe palliative approach at home is feasible in children, and the integration of PPCU could optimise the comprehensive care of previously critically ill children. It is necessary to achieve an optimal domiciliary care, and not just because of patient death. More observational, multicentre and prospective studies are needed to confirm these findings.
La creación de Unidades de Cuidados Paliativos Pediátricos (UCPP) podría optimizar el manejo de niños que tras ingreso en la unidad de cuidados intensivos pediátricos (UCIP) requieren enfoque paliativo. Este trabajo describe las características clínico-epidemiológicas de pacientes derivados por este hecho a la UCPP de la Comunidad Autónoma de Madrid (CAM). Se detallan el tratamiento global requerido, las reagudizaciones, los ingresos hospitalarios y las condiciones del fallecimiento, si se produjo.
Pacientes y métodoEstudio retrospectivo mediante revisión de historias clínicas de pacientes derivados desde las diferentes UCIP de la CAM a la UCPP (1 de marzo del 2008-31 de enero del 2015).
ResultadosSe incluye a 41 pacientes (26 varones/15 mujeres, mediana de edad de 33 meses, rango de 1-228). En seguimiento por la UCPP son los abordajes principales el respiratorio (ventilación invasiva con traqueostomía 8/41), nutricional (20/41 gastrostomía) y farmacológico (29/41 anticomiciales y 34/41antibioterapia). El tiempo de seguimiento fue de 232 días (rango 1-1.164). Requieren ingreso hospitalario 11/41, sin reingresos en UCIP. Fallecen 13/41 pacientes de los cuales 9/13 lo hacen en domicilio, todos acompañados por los cuidadores principales y solo en 1/9 con presencia del equipo domiciliario.
ConclusionesEl enfoque paliativo domiciliario de niños con ingreso en intensivos y dependientes de tecnología es posible. Se requiere hospitalización domiciliaria que no deriva en todos los casos en el fallecimiento del paciente. La integración de UCPP podría así optimizar el cuidado integral de pacientes previamente críticos, siendo necesarios trabajos observacionales, prospectivos y multicéntricos para confirmar esto.
New therapeutic approaches and technological advances have succeeded in reducing mortality in paediatric intensive care units (PICUs). This decline in mortality does not entail a full recovery to the state prior to admission in every case.1,2 The associated morbidity and potential dependency of children on technologies that temporarily or permanently replace a vital function may shorten life expectancy by years without the expectation of death in the short-term. This fact may influence the approach to management in the PICU, increase the use of health care resources and sometimes hinder the discharge home of the patient.3–5
The goal of intensive care treatment needs to be adjusted in this group of patients. It should no longer be to cure, but to tailor treatment to the needs of the patient and uphold the patient's right to individualised care (what does the patient need at this moment?).6,7 Taking into account the emerging needs of the patient sometimes leads to the initiation of a palliative approach that requires the collaboration of paediatric palliative care units (PPCUs).8 These units could adapt the management of these children, facilitating discharge from hospital and their followup at home until they improve or die.9–11 Furthermore, this approach optimises and reduces the use of health care and financial resources.
Thus, paediatric palliative care involves the active and comprehensive care of the body, mind and spirit of the child, and includes services to the family. It aims to improve the quality of care and of life in paediatric patients with terminal or fatal illness and their families through a holistic approach, upholding their right to dignity and autonomy with the delivery of continuous and individualised care.
This article describes the epidemiological and clinical characteristics of patients referred after a stay in one of the PICUs of the Autonomous Community of Madrid to the regional PPCU based in the Hospital Infantil Universitario Niño Jesús. The primary objective of the study was to determine the characteristics of patients referred to the PPCU from the PICU during the period under study. The secondary objectives were to describe the overall management of these patients, analyse exacerbations and hospital admissions, and describe the place and circumstances of death in cases where it occurred.
Materials and methodsWe conducted a retrospective study approved by the Ethics Committee of the Hospital Infantil Universitario Niño Jesús. We reviewed the medical records of patients referred from the different PICUs of the Autonomous Community of Madrid to its PPCU between March 1, 2008 and January 31, 2015 (the unit started its operations in March 2008). We collected data on the following:
- –
Referring hospital, reason for admission to PICU (infection, metabolic or mitochondrial disorder, preterm birth, heart disease, unintentional injury and congenital or prenatally diagnosed disease), age in months, sex and nationality (Spanish, European or other). We classified patients based on the categories established by the Association for Children with Life-threatening or Terminal Conditions and their Families (ACT)12 (Table 1).
Table 1.Categories of patients eligible for palliative care based on the criteria of the Association for Children with Life-threatening or Terminal Conditions and their Families (ACT).
Group 1 Children with life-threatening conditions for which curative treatment is feasible but can fail, where access to palliative care may be necessary alongside curative treatment and/or when treatment fails (children with cancer) Group 2 Children with conditions where premature death is inevitable but there may be long periods of intensive treatment aimed at prolonging life and allowing participation in normal activities (cystic fibrosis, Duchenne muscular dystrophy, HIV infection) Group 3 Children with progressive conditions without curative treatment options, where treatment is exclusively palliative and may commonly extend over many years (spinal muscular atrophy, adrenoleukodystrophy) Group 4 Children with irreversible but non-progressive conditions associated with complex health care needs, that may lead to health complications and with increased likelihood of premature death (severe cerebral palsy, syndromes with multiple congenital anomalies, sequelae of severe disease) - –
Care in the PICU (yes or no): haemodynamic (need for volume expansion with physiologic saline or colloids at doses of 20mL/kg or greater and/or need for inotropic support), respiratory (aspiration of secretions, nebuliser and oxygen therapy/non-invasive ventilation/invasive ventilation) and nutritional support.
- –
Type of PPCU followup, 3 levels:
- 1.
Level I: patient makes scheduled outpatient visits to the PPCU.
- 2.
Level II: scheduled home visits, without care 24h a day/7 days a week.
- 3.
Level III: home-based hospital care, scheduled visits, and facilitation of necessary treatments. Phone consultations and home visits, as needed, available 24h a day/7 days a week.
- 1.
- –
Achievement of discharge to PPCU (yes or no).
- –
Treatment and followup by PPCU (yes or no): gastrostomy, laxative use, spontaneous urination, intermittent urinary catheter, permanent urinary catheter, parenteral delivery of medication at any point, centrally-inserted catheter at any point, peripherally-inserted catheter at any point, anticonvulsant drugs, number of anticonvulsant drugs, infections during followup, oral or intravenous antibiotherapy during followup, oral opioids, subcutaneous opioids, intravenous opioids, opioid rotation, neuropathic pain medication and corticosteroid therapy.
- –
Exacerbations and/or disease progression (yes or no).
- –
Hospital admission during PPCU followup (yes or no).
- –
Death, place of death.
- –
End-of-life care (yes or no): oral benzodiazepines, subcutaneous benzodiazepines, intravenous benzodiazepines, oral opioids, subcutaneous opioids, intravenous opioids, opioid rotation, neuropathic pain medication and corticosteroid therapy.
We made a descriptive analysis of the answers using SPSS 16.0 for Windows. To analyse the results, and given the number of patients included, we performed nonparametric statistical tests. We compared quantitative variables by means of the Mann–Whitney U test, and qualitative variables with the Fisher exact test.
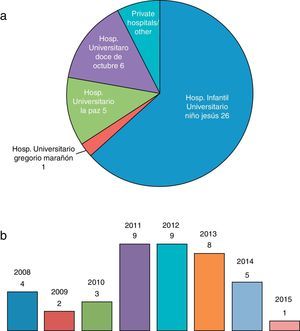
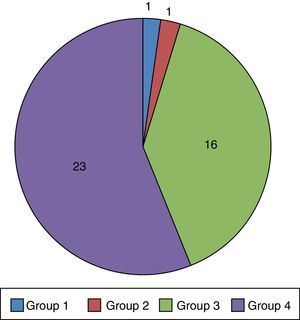
ResultsEpidemiological characteristics and characteristics of management at the Paediatric Palliative Care UnitThe study included 41 patients (26 male/15 female), of who 26/41 were referred from the PICU of the Hospital Infantil Universitario Niño Jesús (Fig. 1a). Referrals were most frequent in the 2011–2015 period (Fig. 1b). The median age was 33 months (range, 1–228 months, ±70.9), with 37/41 patients of Spanish nationality. Fig. 2 presents the distribution of patients by ACT group. The reason for admission in the PICU was infection in 22/41 patients and metabolic abnormalities in 8/41. The rest of the patients were admitted for various causes that could not be grouped.
At the PICU, 5/41 patients experienced haemodynamic changes. All patients required respiratory care (aspiration of secretions, nebuliser treatment and oxygen therapy), with 8/41 undergoing non-invasive ventilation and 8/41 invasive mechanical ventilation requiring tracheostomy in all 8. Nutritional support was provided through nasogastric feeding (NGF) in 30/41, and discontinued prior to discharge from hospital in 2/30.
Home care delivered by the Paediatric Palliative Care UnitIt was possible to discharge all patients home under the supervision of the PPCU, with a median of 232 days of followup (range, 1–1164, days ±389.5). The main caregivers were the mother and father in 26/41 of cases, the mother alone in 10/41, and a specialised facility with custody of the child in 2/41. Of all the included patients, 11/41 transitioned to level I palliative care during the period under study and 10/41 were discharged from the unit. The respiratory support that had been initiated in the PICU was maintained in all patients, with 6 of the 8 patients treated with invasive mechanical ventilation continuing this modality. Twenty-eight patients were referred to the PPCU with a nasogastric tube; the tube was eventually removed in 8, while the other 20 underwent gastrostomy tube placement.
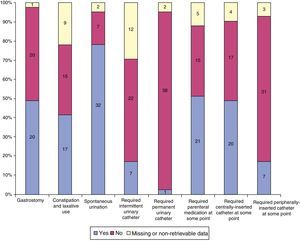
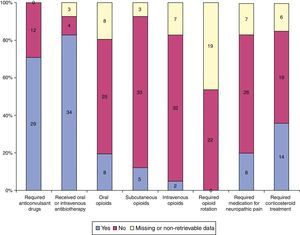
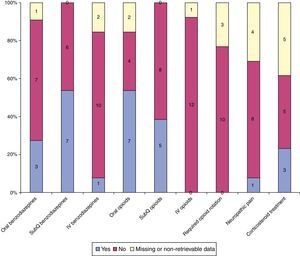
Of all children that received hospital-level care from the PPCU at home, 34/41 experienced exacerbations or had infections, 11/34 required hospital admission for those reasons, and 4/41 for other, end-of-life-related reasons. Fig. 3 describes the need for medical intervention and Fig. 4 the medications received during the followup.
Summary of the pharmacological treatment received by patients during the home-based followup. Patients for which data were missing or not retrievable are represented in yellow. The number of patients for the “yes”, “no” and “missing or non-retrievable data” categories in each column is listed vertically.
During the period under study, 13/41 children died, 9 of them at home and accompanied by their parents and family. Of the 13 that died, 2 had a tracheostomy. The palliative care team was present at the time of death in only 1 case. Fig. 5 summarises the pharmacological care provided at the end of life. The duration of home-based hospital care was shorter in patients who died compared to those who did not (174±180 days versus 456±431.2 days; P=.008).
DiscussionThis is the first study conducted in Spain that describes the children that are discharged from hospital under the supervision of a PPCU after being in critical condition.13,14 We reviewed the cases of patients referred from the different PICUs of the Autonomous Community of Madrid to its PPCU following the opening of the latter in March 2008. We found that respiratory, nutritional and pharmacological management were the most frequent complex needs in these patients.1,15–17 The duration of followup was prolonged, without a predominance of cases ending in death, a near absence of hospital admissions and no readmissions to critical care. Furthermore, in cases that ended in death, the patient most frequently died at home accompanied by the main caregivers and family, without the presence of the palliative care team.1,7,9,18,19
At present, paediatric palliative care is a relatively new field.1,18 Initially it was conceived as an approach specific to the end of life, but it currently allows the treatment of medically complex patients not only in hospital, but also at home.20 It is well known that the development of new technologies and therapeutic approaches has resulted in an increased ability to cure disease associated with a drastic decline in mortality, but also with an increase in the number of children who never return to their previous health status, whose life expectancy is reduced, and whose discharge from the PICU or hospital may be deferred or delayed.1,2,4,8,9,11,15,21,22
In our study, we found that a majority of the patients (39/41) belonged to groups 3 and 4 of the ACT classification (Table 1, Fig. 2), and had most frequently been referred to the PPCU from the hospital where this unit is based (Fig. 1a). We also observed that there was a decline in the number of referred patients in 2014. We cannot determine the reason for this decline with certainty, and many factors may have contributed to it, including epidemiological factors or the establishment of new inpatient units for children with special needs that would allow discharge from PICU as an intermediate step preceding the discharge home. Taking into account the ACT classification and the characteristics of the patients under study, we ought to highlight several aspects.
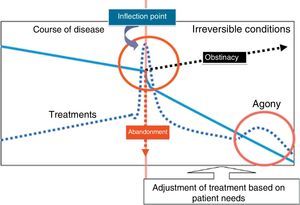
In group 3 of the ACT classification, we found patients with chronic disease that are currently incurable and who required admission to the PICU due to disease progression or an acute event.23 This hospitalisation could represent a temporary increase in medical needs or, at times, a clinical inflection point. This “inflection point” may be a source of dilemmas for the intensive care team, not only as regards admission to the PICU but also in subsequent clinical decision making.6 Based on our observations, intensive care providers may interpret this inflection point as an indication for considering referral to the PPCU to initiate the palliative approach24 (Fig. 6).
Identification of the inflection point in the course of disease in critically ill patients. The identification of the inflection does not warrant increasing the offer of treatment (obstinacy) nor treatment withdrawal (abandonment), instead, treatment should be adjusted progressively, with initiation of palliative care.
On the other hand, group 4 of the ACT classification comprises children with severe nonprogressive illnesses and complex medical needs. This category includes the archetypal PICU patients: previously healthy children who experience a critical event that does not lead to death, but produces sequelae.1 These children usually require prolonged stays and are likely to become dependent on technology to replace or complement lost or impaired vital functions.9 On analysing the treatment received by these patients, as would be expected, respiratory and nutritional support were a frequent feature in their histories.19,21,25,26 A palliative approach may allow discharge not only from the PICU, but more importantly from hospital. Such a development, which may pose both medical and ethical challenges, may be optimised by referral to or consultation with the PPCU.
When we analysed the care received by the children under study, we found that all required respiratory support in the intensive care unit and also during followup by the PPCU.3,19 We also found an increased respiratory complexity in half of the patients, with 8 requiring placement of a tracheostomy tube for mechanical ventilation prior to discharge, which was eventually removed in 2. This aspect, the discontinuation of complex medical care once the patient is transferred to followup by palliative services, has been previously described in the literature and should be investigated further in future research.27
It is known that, overall, the development of home-based care units may be beneficial to critical patients, their caregivers and, given the optimisation of resources, the health care system.5,15,28 The aforementioned “palliative approach” allows the individualisation of care and facilitates the transition of the patient to the home. In many cases, following discharge from not only the PICU but also from hospital, children face a series of hurdles that can be anticipated and resolved with the implementation of a holistic and patient-centred approach.10,21,26
Our analysis of the care provided by the PPCU showed that the complex needs of patients beyond respiratory support or the need for gastrostomy tube placement did not so much involve interventions for compensating function loss or impairment (Fig. 3) as it did the need for multiple drugs, delivered by enteral or parenteral routes (Figs. 3 and 4). In our experience, there is an adjustment period following the discharge home that requires close monitoring until the main caregivers are appropriately trained on the problems that the child is likely to experience.26 The establishment of an adequate care network and the availability of telephone support 24h a day, 7 days a week seem to be essential tools to this end.22
As for exacerbations, we ought to highlight two findings. The first is that none of the patients required readmission to the PICU. This despite the fact that these were patients who in some cases required complex care in terms of technology, equipment or medication.1,4,29 Ongoing care delivery allows an actual therapeutic fit: patients receive treatment based on what they actually need at present, as opposed to what they have experienced at a past point. The second is that we found that exacerbations, which were most frequently due to infection, were mostly treated at home, too, even in cases where drugs had to be delivered parenterally.1,18,30 The number of admissions due to exacerbations would probably have been greater if home-based care had not been available around the clock, but we could not assess the impact of this factor because there was no patient cohort that we could compare this to. We were also unable to retrieve the necessary data to assess the association of the duration of followup by the PPCU and the timing of admission due to exacerbation. Based on the experience of this unit, the longer the duration of followup, the more time caregivers have had to adjust and the more training they have received, the more they have the skills and resources required to manage these situations at home.22,26,29
Our analysis of the end of life, consistent with the existing literature, showed that not all patients discharged from intensive care units to palliative care die within a short period of time.9,20 In our study, the followup lasted more than 3 years in some cases, and some patients were even discharged from the PPCU or moved to a lower level of care. The latter does not mean that patients were cured, but rather reflected partial improvement in some cases and clinical stabilisation in others, so that patients did not require home-based hospital care but rather a periodic followup.
We found that approximately 1 in 4 patients died. The duration of followup was shorter in deceased patients compared to those who survived, which may suggest that once a patient reaches a certain degree of clinical stability, usually at 5–6 months after discharge from the PICU, the probability of death in the short-term decreases. Only 4 of the patients that died did so in the hospital, and of the 9 that died at home, all of them accompanied by their main caregivers, only 1 required the presence of the palliative care team.17 In all other cases, end-of-life symptoms were managed by the main caregivers, which was possible thanks to their knowledge of the patient and the directions received by telephone or in person from the PPCU.10,22,30,31 It seems that this approach to care may reduce hospitalisation at the end of life. Death will take place in the home, if appropriate for the child, based on the acquired knowledge of the caregivers and if the patient and/or the main caregivers have expressed this wish.26,29 This circumstance facilitates coping and grieving in families, who go on to require less social and psychological support.11,20,32
There are significant limitations to this study. We performed a retrospective review in which aspects of interest that were not included in the data collection were a source of bias. For instance, we did not collect data regarding the timing of patient referral to palliative care, the number of days spent in the PICU prior to referral, and the time elapsed between discharge from the PICU and discharge to the home.1 It would have been interesting to collect data on the reason for referral to palliative care, and whether it was made with the aim of allowing the patient to die at home or to achieve discharge from hospital. These aspects should be investigated in future works, since our findings, based on the number of deaths and the days of followup by the PPCU, suggest that the latter was the prevailing reason.33 In addition, there was no previous cohort of patients with which we could make a comparison in order to assess the impact of this approach. Also, and in relation to the institution that the PPCU of the Autonomous Community of Madrid is based in, we found that most referrals were made from the Hospital Infantil Universitario Niño Jesús, which may have biased the results as regards patient characteristics. The analysis of home-based care seems to suffer from fewer methodological flaws, but these data should also be interpreted with caution. We had no data on the psychological, social or spiritual needs34,35 of patients and caregivers, factors that probably influence the care received at home, its complexity, and the decision-making process.36 Furthermore, we could not make a comparative analysis of these factors allowing us to establish, beyond mere description, the complexity of the cared delivered to address them.
In conclusion, we believe that PPCU practices like those described in this study could facilitate the discharge and home-based followup of critical patients in whom both would be otherwise difficult.1,15 The creation and integration of these units would allow the interdisciplinary management of the three major complexities usually found in these children (respiratory support, nutrition and pharmacological treatment).9 Management by the PPCU allows the progressive adjustment of care, minimising hospital admissions and preventing readmission to the PICU. Similarly, end-of-life care becomes a natural progression of management that can be implemented in the home with minimal involvement of the health care system. Once palliative care has been introduced more widely in Spain, it would be interesting to conduct prospective and multicentre studies to establish with certainty not only the strengths but also the weaknesses and opportunities for improvement of this novel therapeutic approach.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank the children and their families, who are the ones that care for the person beyond the ill individual. Also, the paediatric intensive care units of the Autonomous Community of Madrid for perceiving the palliative care model as an opportunity for improvement. Lastly, the health care team of the Paediatric Palliative Care Unit of the Autonomous Community of Madrid, whose members are aware that everything starts with change.
Please cite this article as: García-Salido A, Santos-Herranz P, Puertas-Martín V, García-Teresa MA, Martino-Alba R, Serrano-González A. Estudio retrospectivo de pacientes derivados de cuidados intensivos pediátricos a cuidados paliativos: por qué y para qué. An Pediatr (Barc). 2018;88:3–11.