The increase in survival of children with severe diseases has led to the rise of children with chronic diseases, sometimes with lifelong disabilities. In 2008, a unit for the specific care of medically complex children (MCC) was created in Hospital La Paz.
ObjectivesTo describe the work and care activities of this Unit.
Patients and methodsAn analysis was performed on all discharge reports of the Unit between January 2014 and July 2016.
ResultsThe MCC Unit has 6 beds and a daily outpatient clinic. A total of 1.027 patients have been treated since the creation of the unit, with 243 from 2014. The median age was 24.2 months (IQ: 10.21–84.25). The large majority (92.59%) have multiple diseases, the most frequent chronic conditions observed were neurological (76.95%), gastrointestinal (63.78%), and respiratory diseases (61.72%). More than two-thirds (69.54%) of MCC are dependent on technology, 53.49% on respiratory support, and 35.80% on nutritional support. Hospital admission rates have increased annually. There have been 403 admissions since 2014, of which 8.93% were re-admissions within 30 days of hospital discharge. The median stay during 2014–2016 was 6 days (IQ: 3–14). The occupancy rate has been above 100% for this period. Currently, 210 patients remain on follow-up (86.42%), and 11 children (4.53%) were discharged to their referral hospitals. The mortality rate is 9.05% (22 deaths). The main condition of these 22 patients was neurological (9 patients). Infectious diseases were the leading cause of death.
ConclusionMCC should be treated in specialised units in tertiary or high-level hospitals.
El incremento de la supervivencia de niños con enfermedades graves ha supuesto el aumento de niños con patología crónica altamente compleja, en ocasiones con discapacidades de por vida. En el año 2008 se creó una unidad para la atención específica de los niños con patología crónica compleja (NPCC) en el Hospital La Paz.
ObjetivosDescribir el funcionamiento y la actividad asistencial de esta unidad.
Pacientes y métodosSe analizaron todos los informes de alta de la unidad entre enero de 2014 y julio de 2016.
ResultadosLa unidad dispone de consulta y 6 camas de hospitalización. Se han atendido 1.027 pacientes, 243 desde 2014. La mediana de edad fue de 24,2 meses (IC: 10,21-84,25). Un 92,59% presentaron pluripatología, siendo las condiciones crónicas más frecuentemente observadas las neurológicas (76,95%), gastrointestinales (63,78%) y respiratorias (61,72%). Un 69,54% de los NPCC fueron dependientes de tecnología, el 53,49% de soporte respiratorio y el 35,80% nutricional. El número de ingresos ha aumentado anualmente, hasta 403 desde 2014, con un 8,93% de reingresos. La mediana de la estancia fue de 6 días (IC: 3-14). La tasa de ocupación fue superior al 100% en este período. En la actualidad se mantienen en seguimiento 210 pacientes (86,42%), 11 niños han sido dados de alta a sus hospitales de referencia y 22 han fallecido (9,05%). De estos 22 pacientes, la principal condición fue neurológica, y la principal causa desencadenante del fallecimiento fue infecciosa.
ConclusiónLa unidad de NPCC ha incrementado su actividad en estos años, poniendo de manifiesto la necesidad de crear estas unidades en los hospitales terciarios.
In the last half century, improvements in paediatric care have succeeded in reducing childhood mortality and increasing survival in children with severe diseases.1 This has resulted in an increase in the number of children with chronic disease, at time with lifelong disabilities, who are more medically fragile and complex.2,3 This increase in chronic patients demands a shift in the approach to the development of paediatric treatment plans, which should aim to deliver comprehensive, multidisciplinary and coordinated care. The care of chronic patients is the main task of health care systems in the developed world.2–4
Children with special health care needs (CSHCNs) are those presenting with, or at higher risk of, a chronic physical, developmental, behavioural or emotional condition that consequently require health and related services of a type or amount beyond that required by the general paediatric population.5 Within this group there is a smaller subset, that of medically complex children (MCC), or children with complex chronic conditions (CCCs). The best definition of a child with a CCC is that of a patient with a health condition that would normally be expected to last at least 12 months (unless the patient dies) with involvement of different organ systems or involvement of a single system that is sufficiently severe to require specialised paediatric care and probably periods of hospitalisation in a tertiary care centre.6 Although in countries like the United States CSHNCs amount to only 13–18% of the total of children that use the health care system, some studies report that they generate more than 80% of the total health care costs in the paediatric population.7 This substantial proportion of the total costs is mainly due to these children requiring a greater number of hospitalizations, more frequent admission to intensive care units (ICUs), longer lengths of stay, more technological support, and more specialised services involving multiple specialty clinicians.5,8–14
There is evidence that this subset is at higher risk than the rest of the paediatric population of potentially preventable hospital admissions and/or events, and also at higher risk of being subject to medical errors.6,8,15–17 Many hospitalizations could be avoided by improving care in this group of patients.5,8 In recent years, programmes for the care of patients with chronic complex conditions have been developed, mainly in the United States, to address their needs and improve their management, providing coordinated care.8 There is evidence that the creation of specific units for the care of MCC significantly decreases overall health care costs in this group of children with high use of health care resources.10,18
At present, the Spanish health care system does not have specific care pathways for MCC, which hinders delivery of continued, coordinated and holistic care in this population. In 2008, a unit for the management of complex conditions was created in the Hospital de la Paz, the first of its kind in the country. Our purpose was to describe the operations and health care delivery in this unit, which we consider a model that is both feasible and necessary in other tertiary hospitals and regions of Spain.
Materials and methodsWe conducted a retrospective descriptive study of the infrastructures and resources employed in creating the MCC unit in the Hospital Infantil La Paz in 2008, and analysed the patients that received care from the time a patient register was created for the unit (January 2014). We reviewed all the discharge summaries of patients managed in this unit between January 2014 and July 2016, creating a specific database for the collection of data. We excluded patients that did not fit the definition of MCC. Medically complex children were defined as children meeting either of these 2 criteria: (a) presence of 2 or more complex health conditions that are either chronic or expected to have a long duration (>12 months), or (b) presence of one complex health condition that results in technology dependence and/or requires specialty care, including patients with complex psychological, behavioural or social conditions.6 Technology dependence is defined as the daily need of support from a medical device to replace or compensate for the loss of a vital function.19
We used the chronic condition categories defined by Feudtner based on the ICD-10-CM: respiratory, renal, gastrointestinal, metabolic, hematologic, congenital or genetic, malignancy, cardiovascular, neuromuscular and neonatal. We also included the conditions of transplantation and technology dependence reviewed by Feudtner.18
We conducted the statistical analysis with the IBM SPSS Statistics 23.0 software, with the help of the Section of Biostatistics of the Research Institute of the Hospital La Paz. The project was approved by the Research Ethics Committee of the hospital.
ResultsInfrastructureThe MCC unit is located in an inpatient mother-child ward comprising 17 rooms. Six of these rooms correspond to the MCC unit. The rooms are equipped with ECG monitors, pulse oximeters and conventional oxygen, and are fitted for the installation of non-invasive ventilation and high-flow oxygen systems.
Organisation and human resourcesThe medical team is composed of 4 paediatricians qualified to care for these patients, along with a senior unit coordinator. The nursing staff also has special training and skills in the management of these children, and the nurse to patient ratio is 1:4. There is also a link nurse in charge of coordinating the transfer of patients back to their homes and communication with primary care, and who collaborates with clinicians in training parents and facilitating access to technological devices.
The MCC unit works in collaboration with other paediatric subspecialties to facilitate the continuity of care and coordinates care with the hospital outpatient clinics, the emergency department and community-based services (primary care). The MCC team also handles consultations between paediatric specialties for complex surgical patients, and each of its members performs other specific functions depending on their professional profile. To improve the coordination of care, a daily meeting is held where the current condition of hospitalised children is reviewed, and is attended by different paediatricians with specialties in other fields depending on the current patients. The unit also schedules multidisciplinary meetings to establish treatment goals for each patient, requirements for discharge, the need for palliative care, etc.
From the opening of the unit, continuing care is offered at an outpatient clinic for children with CCCs, both in the form of scheduled visits and on demand, which allows the delivery of urgent care to patients with acute problems. At first the clinic opened one day a week, but given the increase in the number of patients, it has been functioning daily since 2014, staffed by one of the clinicians of the team.
Managed conditions and patientsBetween 2008 and July 2016, the unit has managed a total of 1.027 patients. A register was created in January 2014 that keeps detailed information on these patients. Since then, the unit has managed 290 patients, of who only 243 met the criteria for MCC. Of the latter, 124 (51.02%) were male. Their median age was 24.2 months (interquartile range [IQR], 10.21–84.25). Of the total, 198 came from the Autonomous Community of Madrid, while 45 (18.44%) came from other autonomous communities. At the time of this writing, 210 of the patients (86.42%) remain in followup, 11 (4.53%) have been discharged to their referring hospitals, and 22 have died (9.05%).
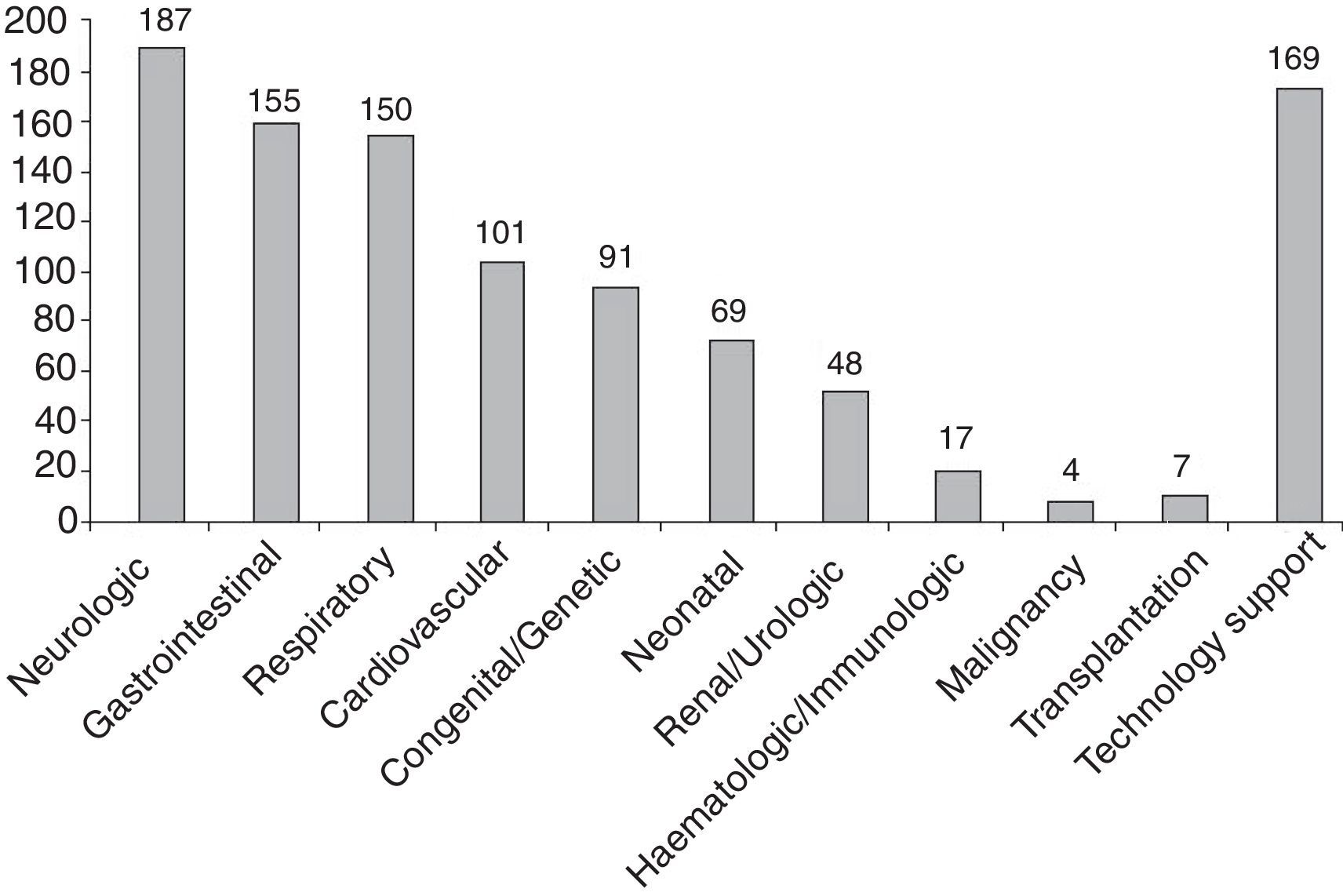
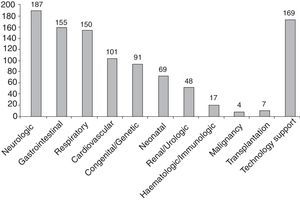
Of the included patients, 92.59% (225/243) had multimorbidity, defined as the presence of 2 or more chronic conditions in different categories. The median number of chronic condition categories per patient was 3, with a maximum of 7 categories in 7 patients. The most prevalent chronic conditions were neurologic, gastrointestinal and respiratory (Fig. 1). One hundred percent of the patients managed in the unit had 6 or more diagnoses documented in the discharge or visit summaries.
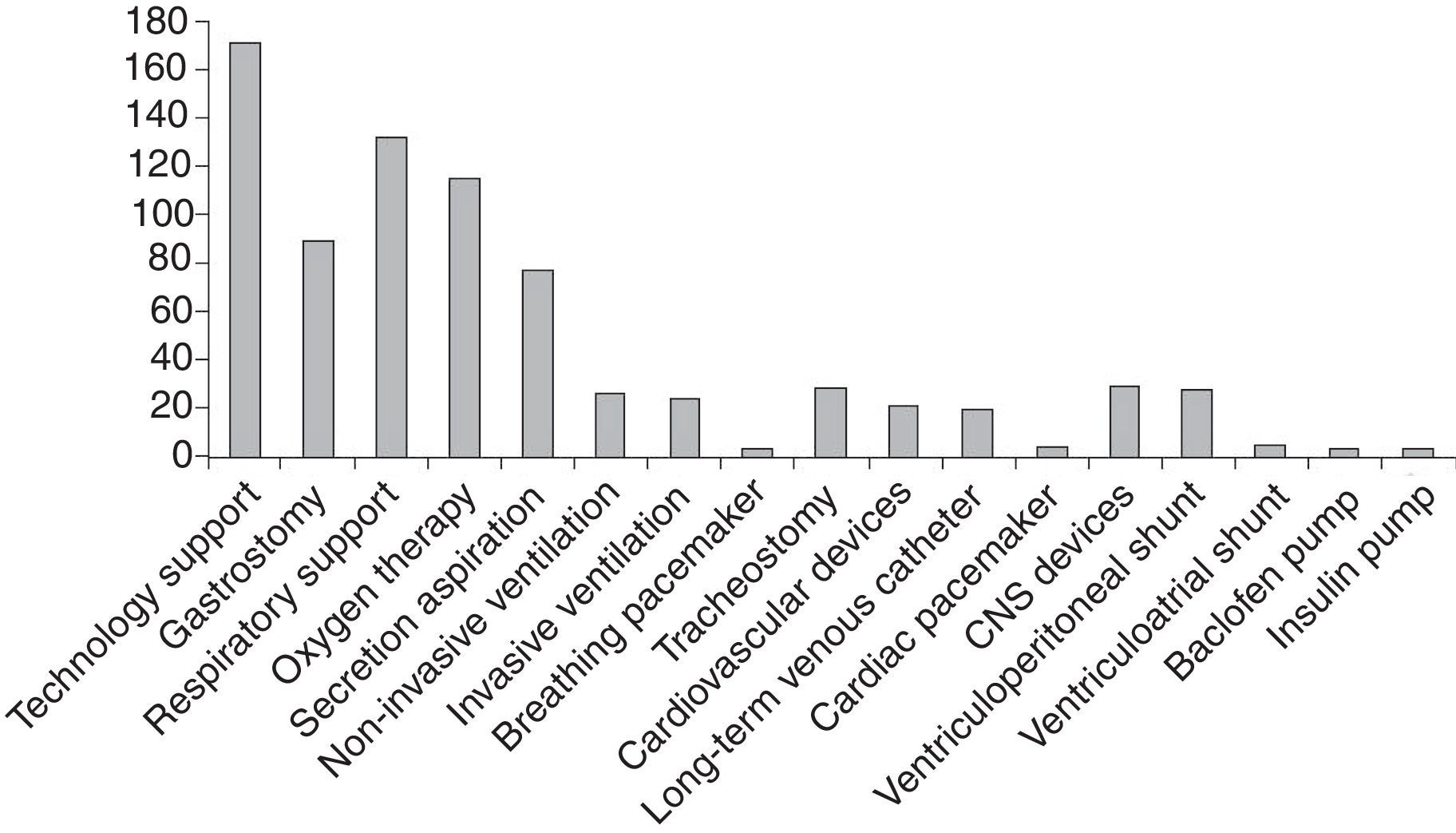
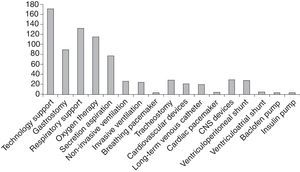
Of all managed patients, 169 (69.54%) were dependent on technology, most frequently on respiratory support (53.49%), followed by nutritional support (35.80%) (Fig. 2).
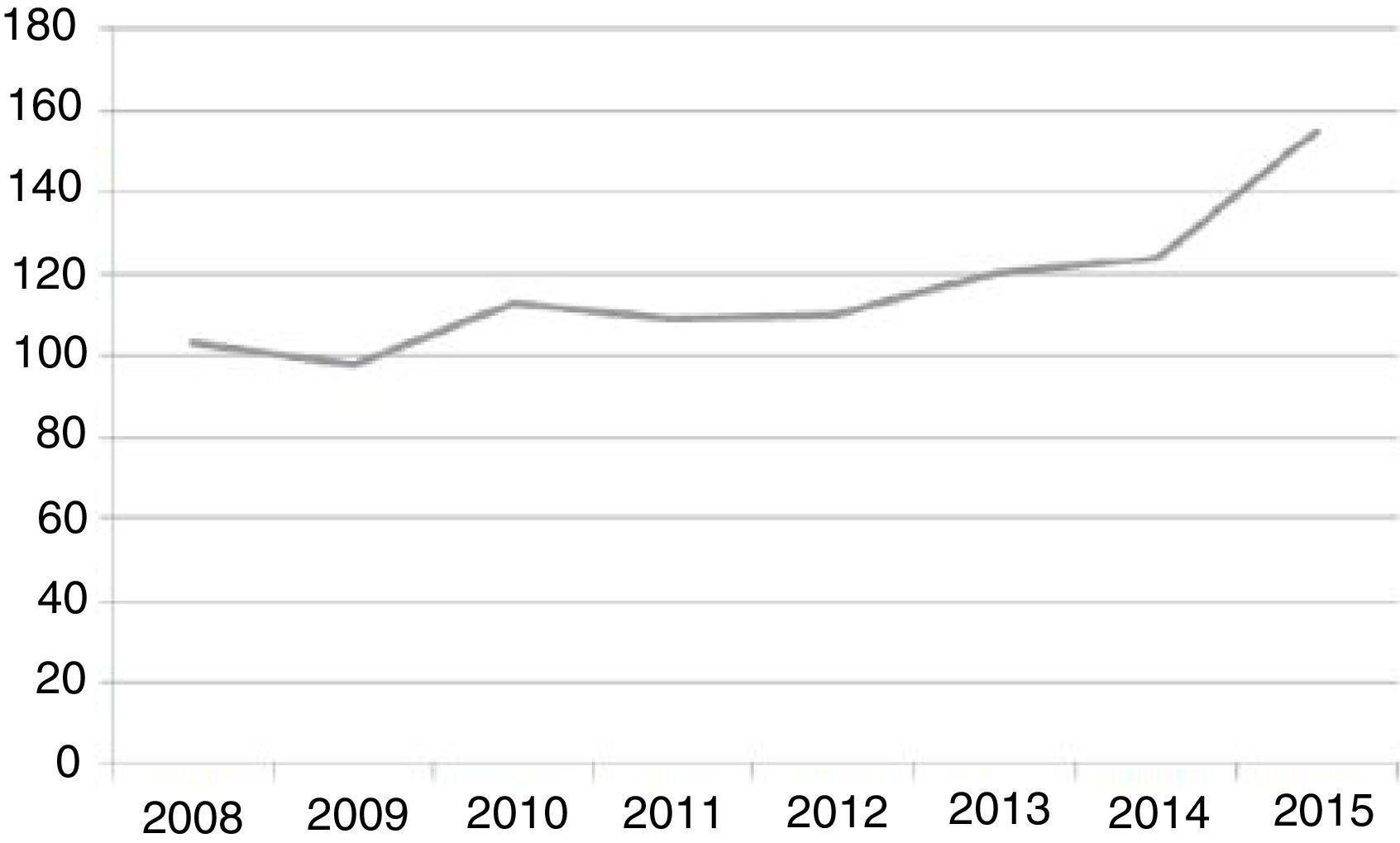
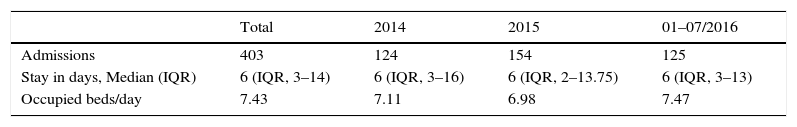
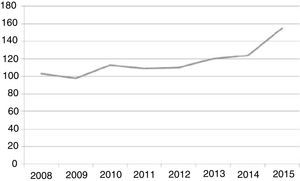
Since the inpatient unit opened, it has admitted a mean 116.37 (±17.43) patients per year, with a progressive increase in time, reaching 154 admissions in 2015, and 125 from January to July 2016 (Fig. 3). Of the 403 admissions from January 2014 to July 2016, 36 (8.93%) were readmissions that occurred within 30 days of hospital discharge. The median length of stay was 25 days in 2008–2010, although there was a significant reduction in the 2014–2016 period, with a median length of stay of 6 days (IQR, 3–14 days). The number of admissions has been increasing progressively. Considering that the unit has a total of 6 beds, unit occupancy has exceeded 100% in the 2014-July 2016 period (see Table 1).
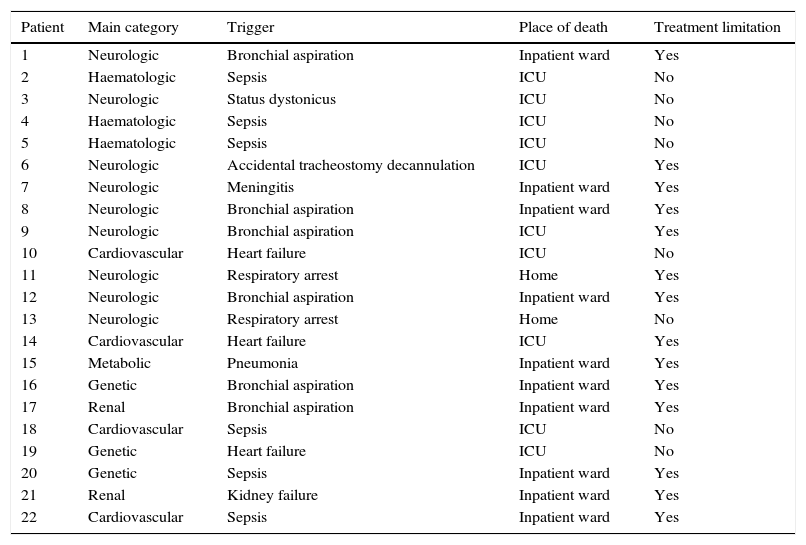
MortalitySince 2008, 67 patients have died in the unit, including 22 since 2014. In the latter 22, the most frequent main chronic condition was neurologic, in 9 patients, followed by haematologic, cardiovascular and genetic conditions (Table 2). Infection was the most frequent cause of death, in 11 patients, with a predominance of aspiration pneumonia, which occurred in 8 cases (mainly in patients with neurologic illness). The place of death was the inpatient ward in 10 cases and the ICU in another 10. Only 2 patients died at home (Table 2). In 14 patients, decisions to withdraw or withhold medical treatment were made based on the course of the disease.
Characteristics of patients that died in MCC unit.
| Patient | Main category | Trigger | Place of death | Treatment limitation |
|---|---|---|---|---|
| 1 | Neurologic | Bronchial aspiration | Inpatient ward | Yes |
| 2 | Haematologic | Sepsis | ICU | No |
| 3 | Neurologic | Status dystonicus | ICU | No |
| 4 | Haematologic | Sepsis | ICU | No |
| 5 | Haematologic | Sepsis | ICU | No |
| 6 | Neurologic | Accidental tracheostomy decannulation | ICU | Yes |
| 7 | Neurologic | Meningitis | Inpatient ward | Yes |
| 8 | Neurologic | Bronchial aspiration | Inpatient ward | Yes |
| 9 | Neurologic | Bronchial aspiration | ICU | Yes |
| 10 | Cardiovascular | Heart failure | ICU | No |
| 11 | Neurologic | Respiratory arrest | Home | Yes |
| 12 | Neurologic | Bronchial aspiration | Inpatient ward | Yes |
| 13 | Neurologic | Respiratory arrest | Home | No |
| 14 | Cardiovascular | Heart failure | ICU | Yes |
| 15 | Metabolic | Pneumonia | Inpatient ward | Yes |
| 16 | Genetic | Bronchial aspiration | Inpatient ward | Yes |
| 17 | Renal | Bronchial aspiration | Inpatient ward | Yes |
| 18 | Cardiovascular | Sepsis | ICU | No |
| 19 | Genetic | Heart failure | ICU | No |
| 20 | Genetic | Sepsis | Inpatient ward | Yes |
| 21 | Renal | Kidney failure | Inpatient ward | Yes |
| 22 | Cardiovascular | Sepsis | Inpatient ward | Yes |
The MCC unit of the Hospital Infantil La Paz has met a growing need in modern inpatient paediatric care in tertiary specialty hospitals. This unit was created in response to the increase in the number of chronic patients that has resulted from the development and expansion of neonatal care, paediatric intensive care and specialty paediatric and surgical services offered at the Hospital La Paz. Although there are no data on the number of children with special health care needs or CCCs in Spain, the fact is that this population is growing in every health care facility, and especially in tertiary care hospitals.4 Since its opening, our unit has offered care to more than 1.000 patients residing in and out of its catchment area, transferred from other hospitals in the Autonomous Community of Madrid and from other autonomous communities that do not have the necessary infrastructure or human resources to care for these patients. In the years that have passed, its level of activity has been increasing, and at present exceeds its capacity, with a level of occupancy of more than 100%, which reflects the current health care needs of these patients. This is a young unit that is still growing and will undoubtedly expand in subsequent years, as observed in other countries.8,12
A high percentage of patients had multimorbidity (92.59%), exceeding the proportions reported by similar units in other countries (41% in the study of Berry et al.8). This may be due to differences in admission criteria between units, as the considerable growth of paediatric subspecialties may have led to the development of specific medical services devoted to the comprehensive management and followup of patients with certain severe chronic diseases, so that the coordinating role of a unit for CCC would be more relevant in patients with diseases involving different organ systems and requiring management by different clinical specialties. The coordination of care is an essential role of paediatric hospitalists, and has demonstrated significant benefits in the optimisation of resources.6,19 It involves treatment planning and diagnostic testing, coordination of the care delivered by subspecialists, the establishment of common goals to be pursued during the hospital stay, the development and revision of care plans, and the establishment of discharge criteria. In recent years, documents have been developed to facilitate patient care and reduce medical errors during hospitalisation (such as clinical care plans and specific progress notes such as “hand-off” documents).20
The most frequent chronic condition category in the patients managed in the unit was the neurologic category, within which the most frequent conditions were infantile cerebral palsy or severe early-onset epileptic encephalopathies. Due to the high frequency of comorbidities in these patients (95.18% with multimorbidity), whether gastrointestinal (swallowing disorder, gastroesophageal reflux, changes in bowel movements …), orthopaedic (hip dislocation, scoliosis, …), respiratory (restrictive lung disease, bronchial aspiration, obstructive apnoeas, …) or involving other systems, they require a comprehensive approach to management, always respecting the contribution of each specialist.21 Gastrointestinal and respiratory conditions are usually associated with a different primary chronic condition. Patients with cardiovascular conditions, who were fourth in frequency in our study (41.56%), constitute an important subset, as most of them have severe congenital heart diseases with involvement of other organs or systems and/or technology dependence (94.05% and 58.41% of our patients, respectively).22,23
The mean length of stay in our unit has decreased significantly after a few years of activity and skill building, and currently equals the lengths reported by similar units.12 Improvements in staff training, increased human and material resources, the work of the link nurse, coordination with primary care facilities and other hospitals, the use of new technologies and above all the continuation of care in hospital-based outpatient clinics are some of the factors that contributed to this decrease. It has been estimated that the creation of MCC units reduces the mean annual inpatient care costs by $1766 per patient per month,15 although we do not have data from our unit to corroborate this figure.
An important aspect that we did not analyse and that could be the subject of future research was the most frequent reasons for admission in MCC. These patients are more likely to experience intercurrent events, such as infections, respiratory exacerbations, nutritional problems and complications related to supportive technology requiring hospitalisation.8,22–24 Another aspect that is just as worthy of investigation is determining the main reasons for hospital readmission. Although readmission only amounted to 8.93% of admissions in our patients, consistent with other studies,15,25 they are considered a marker of inadequate quality of care, as their prevention improves patient quality of life and reduces health care costs.8 However, in MCC the need for readmission cannot always be prevented due to exacerbations of the underlying disease, often due to infections common in childhood. In particularly complex patients, the opportunity to spend time at home improves quality of life, even if it entails relatively frequent readmissions, and therefore readmissions should not be always be interpreted in a negative light.
In many hospitals, these patients are admitted directly to the ICU, as they often require monitoring and treatment measures beyond the usual capabilities and resources of inpatient wards. These patients increase the demand for ICU beds, overcrowding these units while their resources are underutilised, or else they are admitted to inpatient wards that are ill-prepared to face the challenges that they pose. The creation of units with qualified personnel makes it possible for these patients, when their condition allows, to stay in the inpatient ward, with the consequent reduction in health care costs and increased availability of ICU beds for other critical patients. In addition, hospitalisation always has a negative impact, as it increases stress in patients and their families, so it is important to make it possible for parents to be with the patient around the clock.26,27 It may be difficult for highly specialised intensive care and monitoring units to address other aspects of the comprehensive management required by children with CCCs. In addition to the necessary coordination of care, such aspects may involve skill training of family members, the maintenance of sleep-wake cycles or management of the stress that may result from sharing the space with other children in critical condition.
Medical errors are frequent enough to be the third leading cause of death in some countries.28 The greater number of treatments, frequent changes in management and the potential lack of updated summary reports make MCC a population particularly at risk of being subject to more frequent medical errors.9,16–19,29 They are also at higher risk of experiencing adverse events resulting from drug interactions and the off-label use of medications.15 There is evidence that the creation of units to coordinate the care of these children and the use of specific documentation (e.g. hand-off templates) are associated with a reduction in medical errors.17,20
The proportion of technology-dependent patients was higher than the one described by Simon et al.,12 with 46.50% of our patients requiring oxygen therapy, 35.80% a gastrostomy, 18.93% mechanical ventilation, 11.11% a CSF shunt and 10.69% a tracheostomy. The need for mechanical ventilation was associated with higher mortality, longer lengths of stay, increased health care costs and increased need of home-based care.30 Among the deceased patients, 9 (40.09%) had needed mechanical ventilation.
Supporting families through the entire course of disease is of the essence, including, in some cases, the death and mourning of the child (9.05% of the patients). Some patients have irreversible diseases that require the establishment of care plans, with consideration of eventual withdrawal or withholding of treatment. In 73.68% (14/19) of the patients with irreversible diseases that died, such a plan had been established in agreement with the parents; 10 of these patients died in a room in the inpatient ward, a setting that is usually quieter and affords greater privacy and the required dignity; 4 children had been followed up by the palliative care unit of the Hospital Niño Jesús de Madrid, so they received care in coordination with that unit. Another 15 children are currently being followed up by the palliative care unit at Hospital Niño Jesús.
There are telemedicine projects that offer new options for the assessment and treatment of patients with chronic disease, benefitting patients, parents, relatives and caregivers.31,32 One of the objectives of our unit is the implementation of an online home-based support platform, which is in the latest stages of development and we expect to launch in the months to follow, improving the care of our patients.
On account of all of the above, we consider that these patients need to be managed by paediatricians specifically dedicated to chronic complex patients and in specialised units located in tertiary or high level-of-care hospitals. We believe that units for the management of patients with complex chronic conditions need to be developed and run in other tertiary care facilities throughout Spain.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Climent Alcalá FJ, García Fernández de Villalta M, Escosa García L, Rodríguez Alonso A, Albajara Velasco LA. Unidad de niños con patología crónica compleja. Un modelo necesario en nuestros hospitales. An Pediatr (Barc). 2018;88:12–18.