Prevention is an essential aspect in paediatric poisonings, especially when recurrent episodes are detected. The aims of this article are to detect the recurrence rate for suspected poisoning in emergency consultations, as well as to identify the cases in which specific preventive measures are indicated, and to determine whether the creation of a specific item for recurrent episodes in the computerised medical records system facilitates its detection.
Material and methodsA retrospective study was conducted on patients less than 18 years of age treated in the emergency room due to suspected poisoning during 2013 and 2014. Patients were divided according to the presence or absence of previous episodes. From January 2014, a specific item is present in the computerised medical records of the poisoned patient, where the history of previous episodes is registered. The preventive measures used between both groups were compared.
ResultsA total of 731 consultations were recorded for suspected poisoning. A history of previous episodes was detected in 9% of cases. Medical injury reports and follow-up in outpatient clinics were more often performed in patients with recurrent episodes than in patients without them (28.8% vs 18.0%, P=.034, and 65.2% vs. 18.8%, P<.001, respectively). In 2013, the recurrence rate was 5.9% vs 12% in 2014 (P=.004).
ConclusionsThe recurrence rate observed is significant. Although preventive measures are more frequently indicated in these patients, their application is low. The creation of a specific item for recurrent episodes in a computerised medical records system facilitates their detection.
La prevención es fundamental en las intoxicaciones pediátricas, especialmente cuando se detectan episodios repetidos. Los objetivos de este trabajo son determinar la tasa de recurrencias en la consulta por sospecha de intoxicación, evaluar en qué casos se indican medidas preventivas específicas y conocer si la creación de un ítem para episodios previos en la historia informatizada facilita su detección.
Material y métodosEstudio retrospectivo. Se incluyen los pacientes <18 años atendidos en un servicio de urgencias por sospecha de intoxicación en 2013 y 2014; se dividen en 2 grupos según la existencia o no de consultas previas por el mismo motivo. Desde enero de 2014 este dato se registra sistemáticamente en el formulario de la anamnesis del episodio de urgencias para el paciente intoxicado mediante un ítem específico. Se comparan las medidas preventivas adoptadas entre ambos grupos.
ResultadosSe registraron 731 consultas por sospecha de intoxicación. En el 9% se detectaron antecedentes de episodios previos. En el grupo de pacientes con episodios repetidos se cumplimentó parte de lesiones y se realizó seguimiento con mayor frecuencia que en los pacientes sin episodios previos (28,8% vs 18,0%, p=0,034 y 65,2% vs 18,8%, p<0,001, respectivamente). En 2013 la tasa de recurrencia fue del 5,9%, y en 2014 del 12% (p=0,004).
ConclusionesEn un número considerable de pacientes atendidos por sospecha de intoxicación se detectan episodios previos. Aunque en estos pacientes se indican con más frecuencia medidas preventivas, su aplicación es baja. La creación de un ítem específico en la historia informatizada para episodios previos facilita su detección.
Poisoning is generally rare in the paediatric age group, generating approximately 0.3% of visits to paediatric emergency departments (PEDs) in Spain.1–5 However, this prevalence is not unimportant considering that it amounts to 1 visit per day in a PED that receives approximately 100000 visits a year.5 Episodes of poisoning are still a cause of morbidity and mortality both in children and adolescents and pose a significant economic burden,6 aspects that could be minimised if effective preventive measures were put in place.
The overall prevalence of poisoning has remained stable in the past 10 years,7 and exposure is most frequently unintentional.5,8 The Working Group on Poisoning of the Sociedad Española de Urgencias de Pediatría (Spanish Society of Paediatric Emergency Medicine) has reported that the prevalence of past episodes in children presenting with unintentional poisoning ranges between 1.4% and 3.1% (depending on whether they were exposed to household products or medicines, respectively),9 and therefore these patients constitute a high-risk subgroup for which preventive measures ought to be developed.4,10,11
Adolescents are another group of patients requiring specific prevention strategies. In this age group, exposure for recreational purposes and exposure with suicidal intent are more frequent, and carry a higher risk of recurrence.12,13 Thus, there is evidence that 6%–14% of adolescents that attempt suicide make another attempt in the first year of followup.13
At present, the prevention of paediatric poisoning includes measures with a general scope, such as health education for families,9–11 but situations with a sustained risk may call for the use of targeted interventions, such as the involvement of social services or legal authorities.14,15
Despite the importance of recurrent poisoning, few data have been published on its prevalence and the characteristics of its management.
The objectives of the study were to establish the rate of recurrence in patients visiting the emergency department with suspected poisoning, to assess the cases in which specific preventive measures are indicated, and to determine whether the introduction of a specific item on recurrent episodes in the electronic health record facilitates their detection.
Materials and methodsWe conducted a retrospective descriptive study between January 2013 and December 2014 in the PED of a tertiary care women's and children's hospital. We reviewed the electronic health records of all patients aged less than 18 years with a reason for visit or discharge diagnosis associated with exposure to a toxic substance. We classified patients based on whether they had a documented history of past episodes.
The data collection protocol included age, sex, type of substance involved (medicines, household products, alcohol and/or illegal drugs and other), reason for exposure (unintentional, recreational purpose and suicidal intent/abuse), previous episodes, need for treatment in the PED, patient destination at discharge, and specific preventive measures implemented based on reason for exposure (completion of injury report and/or patient followup in outpatient services).
To detect past episodes of suspected poisoning, we reviewed the electronic health records (EHRs) of the hospital and of the shared EHR system of the Institut Català for each patient. Since January 2014, the patient history form for emergency visits due to suspected poisoning in the hospital EHR database has a series of specific items, including a past history of poisoning.
The collected data were entered and processed in a Microsoft Access database created for the purpose. We tabulated quantitative and categorical variables. The data was subsequently analysed using the statistical software SPSS version 20.0 for Windows (IBM, Armonk, New York). We have described quantitative variables using the mean or median, and categorical variables using absolute frequencies and percentages. We performed tests to analyse the distribution of the data (Kolmogorov-Smirnov), and for the comparison of quantitative data (Student t, Mann–Whitney U) and qualitative data (chi square, contingency tables, Fisher exact test). We defined statistical significance as a P-value of less than 0.05.
The study was approved by the ethics committee of the hospital.
ResultsDuring the period under study, the PED received 196979 visits, of which 731 (0.4%) were for suspected poisoning. The median age of patients was 5.2 years (interquartile range, 2.2–15.0 years) and 54.8% were female. Medicines were involved in 49.2% of cases, household products in 24.2%, alcohol and/or illegal drugs in 20.0%, and other substances in 6.6%. The reason for exposure was unintentional in 60.9% of cases, recreational in 20.2% and suicidal intent or abuse in 18.9%. There was a history of past episodes in 9% of cases.
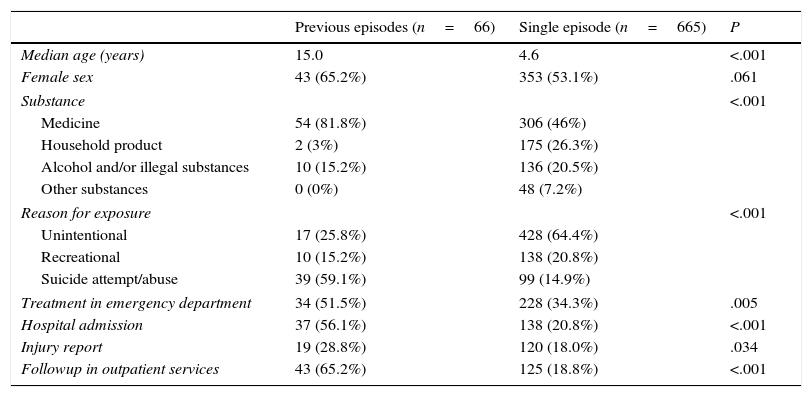
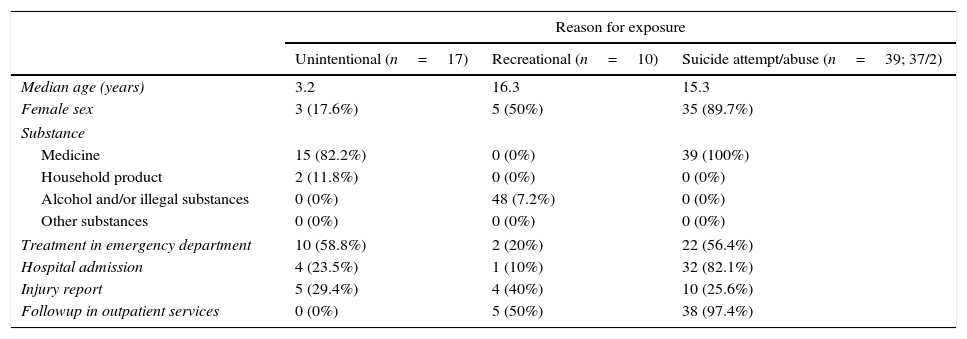
Of all patients, 35.8% required treatment at the PED and 23.9% were admitted to hospital. An injury report was filed for 19% of patients, while 23% were followed up in outpatient services. Table 1 presents the characteristics of the episodes based on whether a past history of poisoning episodes was identified. Table 2 summarises the characteristics of episodes in patients with a past history of poisoning by reason for exposure.
Characteristics of poisoning-related visits by past history of poisoning.
| Previous episodes (n=66) | Single episode (n=665) | P | |
|---|---|---|---|
| Median age (years) | 15.0 | 4.6 | <.001 |
| Female sex | 43 (65.2%) | 353 (53.1%) | .061 |
| Substance | <.001 | ||
| Medicine | 54 (81.8%) | 306 (46%) | |
| Household product | 2 (3%) | 175 (26.3%) | |
| Alcohol and/or illegal substances | 10 (15.2%) | 136 (20.5%) | |
| Other substances | 0 (0%) | 48 (7.2%) | |
| Reason for exposure | <.001 | ||
| Unintentional | 17 (25.8%) | 428 (64.4%) | |
| Recreational | 10 (15.2%) | 138 (20.8%) | |
| Suicide attempt/abuse | 39 (59.1%) | 99 (14.9%) | |
| Treatment in emergency department | 34 (51.5%) | 228 (34.3%) | .005 |
| Hospital admission | 37 (56.1%) | 138 (20.8%) | <.001 |
| Injury report | 19 (28.8%) | 120 (18.0%) | .034 |
| Followup in outpatient services | 43 (65.2%) | 125 (18.8%) | <.001 |
Characteristics of poisoning-related visits in patients with a past history of poisoning by reason for exposure.
| Reason for exposure | |||
|---|---|---|---|
| Unintentional (n=17) | Recreational (n=10) | Suicide attempt/abuse (n=39; 37/2) | |
| Median age (years) | 3.2 | 16.3 | 15.3 |
| Female sex | 3 (17.6%) | 5 (50%) | 35 (89.7%) |
| Substance | |||
| Medicine | 15 (82.2%) | 0 (0%) | 39 (100%) |
| Household product | 2 (11.8%) | 0 (0%) | 0 (0%) |
| Alcohol and/or illegal substances | 0 (0%) | 48 (7.2%) | 0 (0%) |
| Other substances | 0 (0%) | 0 (0%) | 0 (0%) |
| Treatment in emergency department | 10 (58.8%) | 2 (20%) | 22 (56.4%) |
| Hospital admission | 4 (23.5%) | 1 (10%) | 32 (82.1%) |
| Injury report | 5 (29.4%) | 4 (40%) | 10 (25.6%) |
| Followup in outpatient services | 0 (0%) | 5 (50%) | 38 (97.4%) |
In 2014, following the introduction of the specific item in the patient history in the emergency department records, a past history of poisoning episodes was detected in 12% of the patients that visited the PED with suspected poisoning, compared to 9% in 2013 (P=.004).
DiscussionThe incidence of recurrent poisoning episodes in paediatric patients is considerable, amounting to 9% of the total visits for suspected poisoning managed in the emergency department of our hospital during the 2 years under study. Most cases occurred in adolescents, and we found that the need for treatment in the PED and the need for hospital admission were more frequent compared to patients without past episodes of poisoning. These findings are probably related to the reason for exposure, which was intentional in nearly 2/3 of cases, the majority corresponding to patients that poisoned themselves with suicidal intent.
In adolescence, there is a surge of risk behaviours such as substance use, and individuals may experience the onset of psychiatric disorders. Both factors promote events of intentional self-poisoning that in many cases recur over time.12,13,16,17 The PED is the health care setting where adolescent patients that have abused substances, usually with acute problems secondary to this use, like acute intoxication or trauma, are most frequently managed. Therefore, paediatric emergency physicians play an important role in the detection of substance use in adolescents. In this context, performance of brief interventions during the visit and referral to specialty services are measures that have proven effective in the prevention of new episodes.18
The study also evinced the need to perform a thorough psychiatric evaluation and strict monitoring of adolescents that have deliberately ingested poison with suicidal intent. A study conducted in the same PED by Margarit et al. found that 65% of patients managed after a suicide attempt had a psychiatric history, 15% used substances regularly, and 17.4% had made previous attempts.13 Thus, the correct followup of these patients could reduce the risk of recurrence.
On the other hand, and in agreement with the findings of previous studies, we found that in the overall paediatric population, episodes of poisoning were most frequently unintentional, and that repeated episodes did also occur in this subset of patients. Unintentional poisoning happens most frequently in children aged less than 4 years and in the usual residence,11,19 and medicines are the most frequently involved substances.1,3,5,7–9 In recent years, evidence has emerged of the predominance of unintentional paediatric poisoning episodes associated with psychiatric drugs in Spain, exceeding the incidence of poisoning by analgesic and antipyretic drugs.8,20 This evinces an alarming accessibility of this type of drug in households, and suggests that it would be very helpful for the paediatrician in charge to be aware of the presence of psychiatric drugs in the household and to perform targeted preventive interventions in these families.
To present, the greatest efforts in the prevention of poisoning have focused in raising awareness in the community through health education. There is evidence that this strategy improves safety in the home and is associated with a reduction in the number of poisoning episodes.10,21 Furthermore, scientific societies have developed strategies for monitoring poisoning cases. Thus, in 2008 the Working Group on Poisoning of the Sociedad Española de Urgencias de Pediatría launched a toxicology surveillance system with the participation of every PED in Spain that has allowed raising awareness of changes in the epidemiology of paediatric poisoning cases, such as the increase in the incidence of alcohol poisoning1 and psychiatric drug overdose.20 Meanwhile, the Committee on Safety and the Prevention of Unintentional Injuries in Childhood of the Asociación Española de Pediatría (Spanish Association of Paediatrics) has recently published recommendations for the prevention of poisoning that paediatricians must convey to families.11
In spite of these measures, the prevalence of poisoning in the paediatric age group remains stable or tends to increase, and, as our study demonstrates, some patients present with recurrent episodes of poisoning. Targeted interventions are probably needed at the time of the emergency visit, when families are aware of the risk of such events and are more likely to implement recommendations. Emergency paediatricians need to allocate time to informing of preventive guidelines, orally as well as in written form, and to complete an official injury report.14,15,17 We must not forget that child abuse may be passed off as unintentional poisoning. Filing an official report is an act of notification that warns of a potential risk situation, especially when it comes to recurrent events in a single patient. Likewise, the detection in the PED of a past history of similar episodes reflects that the patient is at risk and requires the implementation of targeted interventions, such as involving the social work team at the hospital or local social services.
Our study demonstrates that the introduction of a specific item on previous episodes in the patient's electronic health record helps detect this type of history. It also shows, based on our findings, that the detection of recurrent episodes of poisoning was followed by the implementation of specific measures more frequently in these patients compared to patients without such history, although there is still room for improvement, especially when it comes to the filing of injury reports. Nevertheless, injury reports were completed in 10% more patients in this group, and we ought to emphasise that they should be filed for every case of poisoning. When it came to the followup after the emergency visit, we ought to highlight that every case of recurrent self-poisoning with suicidal intent resulted in the followup of the patient in the department of child psychiatry, and that followup of patients with recurrent recreational exposure with referral to social services, the department of psychiatry or the substance abuse unit improved significantly compared to patients without a documented past history of poisoning.
The main limitation of this study is its retrospective design, as some of the data collected for patients may not have been documented correctly in the emergency department discharge summary. This is demonstrated by the increase observed in the number of cases with a previous history of poisoning after a specific question on the subject was included in the patient history form. Although we attempted to minimise this limitation by reviewing the electronic health records of the hospital and the regional health database for Catalonia, it is possible that the number of patients that actually had repeated episodes in the early period was greater than we calculated. In addition, given that the study was conducted in a single centre with a high level of care that is the regional referral hospital for child psychiatry, the results may not be extrapolated to the general population, and the proportion of patients with previous episodes of poisoning and suicidal intent may have been overestimated.
In conclusion, our study shows that the rate of recurrence of poisoning episodes is considerable, and that the introduction of a specific item in the electronic health records facilitates its detection. Paediatric emergency physicians need not only treat acute episodes of poisoning appropriately, but also strive to provide education at the time that families and adolescents are most vulnerable, ensure the correct followup of the patient, and report potential risk situations to the legal authorities and social services.
Conflicts of interestThe authors have no conflicts of interest to declare
Please cite this article as: García González E, Trenchs Sainz de la Maza V, Martínez Sánchez L, Ferrer Bosch N, Luaces Cubells C. Episodios repetidos de intoxicación: signo de alarma de situaciones de riesgo. An Pediatr (Barc). 2017;87:284–288.