Poisoning is the fifth leading cause of death from unintentional injury in the WHO European region, while Spain is in the group with a lower rate. Most involuntary poisonings occur in young children in the home, due to unintentional ingestion of therapeutic drugs or household products stored in non-original containers and/or within reach of children.
In this article, the Committee on Safety and Non-Intentional Injury Prevention in Childhood of the Spanish Association of Paediatrics provides a series of legal and educational recommendations aimed at preventing such cases.
Las intoxicaciones constituyen la quinta causa de muerte por una lesión no intencionada en la región europea de la OMS, si bien España se encuentra en el grupo con una menor tasa. La mayoría de las intoxicaciones no voluntarias se dan en niños pequeños, en su casa, por la ingesta de medicamentos o productos del hogar. De estos últimos un porcentaje importante se almacena en recipientes no originales o al alcance de los niños.
En el presente artículo, el Comité de Seguridad y Prevención de Lesiones No Intencionadas en la Infancia de la Asociación Española de Pediatría proporciona una serie de recomendaciones tanto educativas como legales para prevenir este tipo de lesiones.
Death caused by unintentional poisoning is rare, and the rate has gone down drastically in the last 50 years.1 This is mainly due to the use of medication containers and household products with child-resistant locks and the existence of safer medications. Other reasons that explain this decrease are the greater safety of consumption products, prevention regulations, public education, legal provisions, the establishment of toxicology centres, improvement in medical assistance and the availability of new antidotes.2,3
Poisonings have more severe effects in children than in adults since they are smaller, have quicker metabolic rates and are less capable of fighting toxic chemical products.4
EpidemiologyPoisonings constitute the fifth cause of death due to unintentional injury in the WHO European region. Every year, 3000 children under the age of 14 die of acute intoxication. Most cases are caused by exposure to toxic substances in children under the age of 5, those under the age of 2 being especially vulnerable.5 Death by poisoning in children and adolescents shows an uneven distribution in Europe, with a risk up to 40 times higher in some countries. The highest rates were observed in Lithuania, Ireland and Estonia in boys, and Romania, Latvia and Lithuania in girls. Spain is among the group of countries with a lower mortality rate.5
More than 90% of these poisonings occur at home, and many commonly used household products may cause them, including medications, cleaning products, beauty products, alcohol, plants and pesticides.5
In spite of the decrease in mortality, visits to the paediatric emergency departments in Spain have not decreased6 and despite the low mortality rate, morbidity and the use of health care resources including outpatient treatment, transport, tests, emergency department costs and hospital admissions, are still important factors to be considered.
Unintentional poisonings seen at the paediatric emergency departments occur mainly due to the ingestion of medications and household products, especially in the kitchen or living room. The medications most frequently involved are psychiatric drugs (particularly benzodiazepines) and paracetamol. Up to 25% of unintentional poisonings caused by household products are due to the ingestion of substances stored in non-original containers, and up to 25% of families admitted that they stored these products within the reach of children. One-third of the families contact another service before visiting the hospital, where nearly half of the children seen receive some kind of treatment and are admitted for at least a couple of hours. The performance of tests, administration of treatment and hospital admission are the most frequent actions taken in the case of medication poisonings.7
The appearance of new products such as detergent capsules and their presentation in attractive colours have generated huge concern in the paediatric world due to the risks their ingestion generates, and this has led to calls for preventive measures affecting packaging, appearance, labelling and awareness-raising.8
Aside from accidental consumption of toxic substances, unintentional poisonings can also be caused by errors in the administration of medications. This accounts for 6% of poisonings recorded in the Spanish paediatric emergency departments. These poisonings are due to errors in the dose calculation of medications (particularly antipyretics and antihistamines) administered to children under the age of 12 months.9
Strategies that have proved effective in the prevention of unintentional poisoning- •
The safe storage of toxic substances eliminates the risk of poisoning to a greater extent than parent supervision, and constitutes an efficient method of preventing poisoning injuries.10–12 Studies on the way in which children access toxic substances indicate that the most vulnerable moment is when the substances are being used, and that safe packaging cannot compensate on its own for unsafe storage and use. This highlights the importance of improving the safety of medication storage and the method of administration in the household. These changes must be backed by regulations and awareness-raising measures implemented both by manufacturers and local authorities, with clear labelling (and clear administration instructions) on the container, coupled with improved parental supervision, child education, and advice from paediatricians.
- •
The law regarding child-proof containers reduces the incidence of poisoning,10,13,14 although the level of compliance affects efficiency,15 and the law will be more effective if supported by awareness-raising activities.16
- •
Toxicology centres can reduce healthcare costs considerably, provided the public is aware of their services.10,13 These institutions are only effective if parents are familiar with their services and know how to contact them. Awareness-raising activities will help to raise their profile.13
Almost all poisonings occur when parents or carers are at home but not paying attention. The most dangerous potentially toxic substances found in the home are medications, cleaning products, antifreeze, windshield washer fluid and pesticides.
The following products are commonly found in the home and are potentially hazardous4:
- •
All medications.
- •
Bathroom: cleaners, sprays, perfumes, colognes, hair sprays and mouthwashes.
- •
Household products: cleaners, polishers, solvents, and products containing bleach and acid.
- •
Garage or workplace: insecticides, kerosene, lighter fluid, turpentine, paint, glue, batteries, pneumatic fluid and antifreeze.
- •
Kitchen: detergents, bleach, softeners and pet products.
- •
Garden: fertilisers, pesticides, plants, mushrooms and berries.
- •
Storage of substances4,17:
- •
Recommend storing medicines, cleaning and laundry products, paints/varnishes and pesticides in their original containers in locked cupboards or drawers, out of the sight and reach of children.
- •
Emphasise dangers of storing any potentially toxic substance in a non-original container or in a container without identification and, particularly of storing it in attractive-looking containers or containers that may be confused with foods or drinks.
- •
Emphasise the need to install automatic safety latches on the doors to cupboards that are within children's reach and contain products that may be toxic.
- •
Ask parents to store remote controls, key rings, congratulations cards and musical books for children in a safe place. These devices and others may contain small button batteries that can cause injury if consumed.
- •
- •
Advise parents to, as far as possible, acquire containers with safety latches for storing medicines, and keep these out of the reach of children.4,17
- •
Advise parents to check the label every time a medicine is administered to a child, so as to administer the4,17 correct dosage. For liquid medicines, the dispenser included with the medicine should be used.
- •
Educate parents to never refer to the medicine as “sweets” or give them any other attractive name.
- •
Insist that parents discard unused medication.
- •
Discourage parents from taking medication in front of the children.
- •
Recommend the purchase of household products with safety fasteners and close them once they are used.4,17
- •
Consider the availability of a safety fastener when prescribing a medication.
- •
Advise parents to be particularly vigilant whenever there is a change in routine, such as holidays, grandparents’ visits or visits to the grandparents’ home and other special events.
- •
Find out which household products or plants are toxic. If unsure about a substance or plant, it should be kept out of children's reach.4,17
- •
Recommend keeping coal, wood or kerosene heaters in safe operating condition, and the same for smoke and carbon monoxide detectors.
- •
Advise parents to keep the phone number of the National Institute of Toxicology within easy reach.
- •
Advise parents to apply all these measures not only in their own home but also in other homes frequented by children, at the grandparents’ house.
Royal Legislative Decree 1/2007 and Royal Decree 1801/2003 make it mandatory to place safety fasterners on chemical product containers for the household, and not to use label designs that may attract children's curiosity. They must also include the instructions “Keep out of children's reach” and “In case of accident or danger to health, visit the doctor or call the National Institute of Toxicology (with the Institute's phone number.18)”
There is also a specific regulation for each type of product.
Royal Decree 3360/1983 sets out the mandatory safety measures in containers for products containing lye. It stipulates that caps or lids must be strong and secure enough to withstand normal handling. They should also have a child-proof opening device, and containers or labels with designs that may attract or awaken children's curiosity are not authorised.18
Royal Decree 770/1999 prohibits detergents and cleaners with a specific shape, smell, colour, appearance, presentation, labelling, volume or size, in order to prevent consumers, especially children, from confusing them with food products and putting them in their mouth, sucking them or consuming them. It details the safety profile of and design characteristics of containers and their opening devices, in order to ensure they do not attract the attention of children or cause confusion in adult consumers. However, there is no explicit reference to the need for child-proof opening devices.18
Royal Decree 1599/1997 (amended) lists the beauty products that should include the instruction “Keep out of reach of children.”
The legislation regarding medications, formulas and official preparations establishes that a special warning must be included indicating that the medication should be kept out of reach of children (Royal Decree 175/2001: art. 6, Regulation [EC] n° 1394/2007 of the European Parliament and Council: Annex III, Royal Decree 1345/2007: Annex III.)
In spite of the legislation, several aspects could obviously be improved.
Thus, the Committee on Safety and Prevention of Unintentional Injuries in Childhood considers that the following actions should be taken to prevent unintentional poisoning:
- •
Increase efforts through improvement in the application of laws and, particularly, regarding the safety caps of certain cleaning products and the appearance of new detergents for washers and dishwashers. In this regard, it urges the withdrawal of products that may clearly be confused with food products, in violation of Royal Decree 770/1999, since children may put them in their mouths, suck them and consume them.
- •
Develop European safety measure standards for containers and closure devices particularly for medications and household cleaning products.
The authors declare that there are no conflicts of interest.
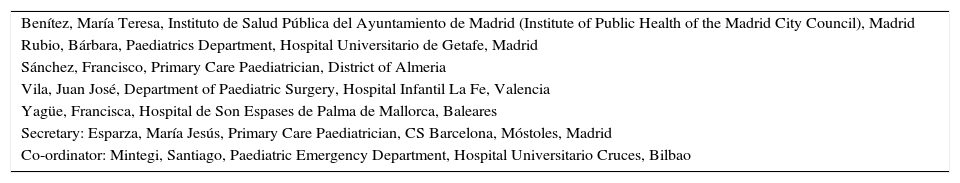
| Benítez, María Teresa, Instituto de Salud Pública del Ayuntamiento de Madrid (Institute of Public Health of the Madrid City Council), Madrid |
| Rubio, Bárbara, Paediatrics Department, Hospital Universitario de Getafe, Madrid |
| Sánchez, Francisco, Primary Care Paediatrician, District of Almeria |
| Vila, Juan José, Department of Paediatric Surgery, Hospital Infantil La Fe, Valencia |
| Yagüe, Francisca, Hospital de Son Espases de Palma de Mallorca, Baleares |
| Secretary: Esparza, María Jesús, Primary Care Paediatrician, CS Barcelona, Móstoles, Madrid |
| Co-ordinator: Mintegi, Santiago, Paediatric Emergency Department, Hospital Universitario Cruces, Bilbao |
Please cite this article as: Mintegi S, Esparza MJ, González JC, Rubio B, Sánchez F, Vila JJ, et al. Recomendaciones sobre la prevención de intoxicaciones. An Pediatr (Barc). 2015;83:440.e1–440.e5.
Members of the Committee on Safety and Prevention of Unintentional Injuries in Childhood of the Spanish Association of Paediatrics is presented in Annex I.