Congenital heart disease (CHD) is one of the most frequent congenital diseases. When expectant fathers and mothers are informed of a CHD during pregnancy, they have to confront a series of individual and interpersonal psychological changes. The aim of the study was to evaluate the psychological impact of a prenatal diagnosis of CHD on expectant parents. The sample included 214 participants, mothers and their partners (case group, 57 pregnant women carrying a foetus with CHD and their partners and control group, 50 pregnant women and their partners).
MethodAdministration of the BSI-18, the DAS and FACES-III following prenatal diagnosis.
ResultsMany parents (approximately 83.6%) went through stages of shock and denial in response to the diagnosis of disease that they had to confront and accept. At the individual level, 35.1% of fathers and 47.4% mothers had clinically significant scores of psychological distress. At the couple level, both fathers (77%) and mothers (82.4%) had expressed an idealized dyadic adjustment. Lastly, the perception of the family dynamic by 43.9% of fathers and 42.2% of mothers was in the mid range.
ConclusionThe results highlight the complexity of the initial stage that these couples were going through.
Las cardiopatías congénitas (CC) se encuentran entre las enfermedades congénitas más frecuentes. Cuando se informa a los padres y las madres del diagnóstico de una CC durante el embarazo, tienen que afrontar una serie de cambios psicológicos a nivel individual e interpersonal. El objetivo del estudio era evaluar el impacto psicológico que produce en los padres el diagnóstico de una CC en el periodo prenatal. La muestra incluyó 214 participantes, madres y sus parejas (grupo de casos: 57 gestantes con fetos diagnosticados de cardiopatía congénita y sus parejas, grupo control: 50 gestantes y sus parejas).
MétodoAdministración del BSI-18, el DAS y el FACES-III tras el diagnóstico prenatal.
ResultadosMuchos progenitores (alrededor del 83,6%) pasaron por fases de choque emocional y negación tras recibir el diagnóstico de una enfermedad que necesitaban afrontar y aceptar. A nivel individual, el 35,1% de los padres y el 47,4% de las madres tuvieron puntuaciones significativas en el malestar psicológico. A nivel de la pareja, tanto los padres (77%) como las madres (82,4%) presentaron un ajuste diádico idealizado. Por último, el 43,9% de los padres y el 42,2% de las madres reflejaron una dinámica familiar moderada.
ConclusiónLos resultados ilustran la complejidad de la etapa inicial que atravesaban las parejas participantes.
Congenital heart disease (CHD) is a major cause of infant mortality with an incidence of approximately 8 per 1000 live births.1,2 It is one of the most common types of congenital anomalies and accounts for 20% of stillbirths.3
Thanks to technological advances in foetal echocardiography, obstetrics and foetal medicine, cardiac anomalies are currently diagnosed with increased accuracy and detail in the prenatal period.4 Early diagnosis of cardiac anomalies provides families accurate information on the clinical condition of the foetus during pregnancy, the postnatal prognosis and even the surgical interventions that may be necessary.5
The birth of a child always involves a series of changes in the family structure, but if there is also a diagnosis of disease, the future parents face an unexpected, disturbing, unknown and disconcerting situation that they usually perceive negatively.6 This changes their expectations for the child and requires that they process the loss of the imagined healthy child.7,8,9 The diagnosis of CHD often leads to anxiety, disorientation, anguish and guilt. There are also often feelings of frustration, anger and despair, as well as a belief that the family has limited resources to cope with the situation.10,11
Several researchers have documented the impact of CHD in children, who in many cases face a lifetime of hospital admissions, medical visits and painful procedures. It is not only the children, however, that suffer the physiological and psychological consequences of CHD, as it also has an impact on family dynamics.12,13 Studies of parents of children with congenital adrenal hyperplasia due to 21-hydroxylase deficiency have evinced the dramatic psychological impact on families. Patients with this disease require lifelong treatment, and the recurrent hospitalizations and stressful situations can take a toll on the relationships of parents with one another and on family organization.14 Meanwhile, there is evidence suggesting that the reactions of families to cancer diagnoses in children change over time. The initial response is usually shock and panic, followed by feelings of depression, rage and guilt at the start of treatment.15 In these cases, too, the emotional impact of the diagnosis affected the daily life of parents in addition to family organization and functioning.16,17
Another study compared mothers of children with a prenatal diagnosis of CHD with mothers whose children had received the diagnosis after birth.18 The researchers found that the time of diagnosis can play an important role, as parents who are made aware of the problem in the prenatal stage can begin the process of confronting and accepting the situation at that point. In this way, parents can take a more active role in the planning of prenatal and postnatal care for the child, and they are better prepared for the birth and subsequent course of the disease.19
A wide range of studies on patients with CHD have shed light on the physical and biological aspects associated with cardiac anomalies and their clinical outcomes.20–24 However, researchers have only recently started to analyse family functioning and the ability of couples to cope with the diagnosis of CHD in their children.25 Despite this recent interest, few studies have examined differences in the perception of this experience based on sex.26,27
The aim of the study was to identify the difficulties experienced by parents that receive a prenatal diagnosis of severe CHD. To this end, we collected and analysed data on difficulties faced by parents at the individual, couple and family level in the initial stage following prenatal diagnosis of CHD compared to control couples. A secondary objective was to assess whether there were differences based on the parental role (father versus mother). We also collected data on psychological distress, dyadic adjustment and family dynamics for the purpose of determining which psychological interventions and forms of support would be appropriate for couples during this long process in the hospital.
MethodsWe conducted a multicentre prospective case-control study in 2 university hospitals in Barcelona, Spain (Hospital Vall d’Hebron and Hospital Sant Joan de Déu).
The study protocol, including the inclusion and exclusion criteria, are explained in detail in a previous publication (https://pubmed.ncbi.nlm.nih.gov/31506079/). Pregnant women past 20 weeks of gestation managed at the foetal medicine unit of a participating hospital on account of a diagnosis of foetal cardiac anomaly were eligible for inclusion as cases. We invited women carrying a healthy foetus and receiving outpatient care in the same hospitals to participate as controls. The study protocol was approved by the ethics committee of each participating hospital, and we obtained written informed consent from every participant.
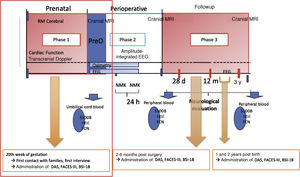
The study was conducted in the context of a larger project approved by the Clinical Research Ethics Committee of the Hospital Vall d’Hebron in Barcelona (CEIC PR [AMI] 307/2012). The larger project was structured in 4 phases, each with its own objectives and protocols. This article focuses on the primary objective of the first phase (Fig. 1).
All participants provided written consent for the storage and use of the obtained data for research purposes. Study sessions consisted of two parts. In the first part, the couple were informed of the study objectives and protocol and provided informed consent. The second part was devoted to data collection. Couples were interviewed together, followed by administration of individual questionnaires: the Brief Symptoms Inventory-18 (BSI-18), the Dyadic Adjustment Scale (DAS) and the Family Adaptability and Cohesion Evaluation Scale, version III (FACES-III).
Psychological assessment of parentsThe BSI-18 is a brief inventory of psychological symptoms designed to detect distress and the most frequent psychiatric symptoms in the general population and in health care users managed at the primary care level. It is also useful for detection of psychological distress associated with more serious psychiatric disorders, since somatization, depression and anxiety are frequently found in patients with these disorders. As the name implies, the BSI-18 consists of 18 items (6 regarding somatization, 6 regarding depression and 6 regarding anxiety), and the total score can range from 0 to 72. A Global Severity Index (GSI) greater than 63 indicates the presence of clinically significant manifestations.28
The Dyadic Adjustment Scale (DAS) is one of the instruments used most widely to assess the quality of couple relationships and adjustment.29 It is a multidimensional scale applicable to married couples and other couples of similar characteristics. The questionnaire comprises 32 items divided into 4 subscales (dyadic satisfaction, dyadic consensus, dyadic cohesion and affective expression) that yield an overall dyadic adjustment score, with a maximum possible score of 151 points and the normal range defined as 100–125.30
The Family Adaptability and Cohesion Evaluation Scale, version III (FACES III) is a 20-item instrument based on the circumplex model developed by Olson, Sprenkle and Russell in 1979.31,32 The FACES III assesses the 2 main dimensions of the circumplex model: cohesion (with 4 categories: disengaged, separated, connected and enmeshed) and adaptability (with 4 categories: rigid, structured, flexible and chaotic).33 The assessment is based on a distribution of 16 types of family dynamics and 3 types of family (balanced, mid-range and unbalanced).
We also collected data on sociodemographic characteristics (sex, age, place of residence, educational attainment, employment status, etc) and the diagnosis of the child.
The data were analysed with the software IBM SPSS Statistics for Windows, version 23.0 (released 2015; IBM Corp, Armonk, NY, USA). We performed a descriptive analysis, calculated frequencies and assessed correlations. We used the Spearman test to assess correlations and the Mann–Whitney U Student t tests to compare groups and mothers and fathers. We performed the same analysis for the results of the BSI-18, DAS and FACES III. We also performed multivariate analysis of the sociodemographic characteristics of the participants.
ResultsThe final sample consisted of 214 participants, or 107 couples (family units), of which 57 were family units that had received diagnoses of CHD during pregnancy (case group). The remaining 50 couples were included as controls (control group).
In the case group, the age of participants ranged from 20 to 46 years (mean, 33.06; SD, 5.66). When it came to educational attainment, 46.5% (n = 53) had university degrees, and only 2.6% (n = 3) had no formal education. As for marital status, 71.9% of the couples (n = 41) were married and 28.1% unmarried (n = 16). In terms of the type of pregnancy, 86% of couples (n = 49) had conceived spontaneously while 14% (n = 8) had undergone fertility treatment. Participants in the control group were aged 25–49 years except for one father who was 79 years old (mean, 34.66; SD, 6.48). In terms of educational attainment, 57% (n = 57) had university degrees. The distribution by marital status was 70% married (n = 35) and 30% unmarried (n = 15). As for the type of pregnancy, 92% (n = 46) had conceived spontaneously and 8% (n = 4) had undergone fertility treatment (Table 1).
Demographic characteristics of the study groups.
| Demographic characteristics | |||||
|---|---|---|---|---|---|
| Case group | Control group | ||||
| n | % | n | % | P | |
| Marital status | |||||
| Married | 41 | 71.9 | 35 | 70.0 | .826 |
| Not married | 16 | 28.1 | 15 | 30.0 | .826 |
| Educational attainment | |||||
| University degree | 53 | 46.5 | 57 | 57.0 | .125 |
| BUP | 1 | .9 | 1 | 1.0 | .926 |
| FP | 7 | 6.1 | 1 | 1.0 | .048 |
| EGB | 6 | 5.3 | 8 | 8.0 | .419 |
| Vocational training | 7 | 6.1 | 21 | 21.0 | .001 |
| High school | 7 | 6.1 | 4 | 4.0 | .479 |
| Middle school | 21 | 18.4 | 8 | 8.0 | .026 |
| Primary school | 9 | 7.9 | 0 | 0 | .004 |
| No formal education | 3 | 2.6 | 0 | 0 | .102 |
| Type of pregnancy | |||||
| Spontaneous conception | 49 | 86.0 | 46 | 92.0 | .324 |
| Fertility treatment | 8 | 14.0 | 4 | 8.0 | .324 |
| Place of residence | |||||
| Catalonia | 52 | 91.2 | 49 | 98.0 | .129 |
| Outside Catalonia | 5 | 8.8 | 1 | 2.0 | .129 |
| Employment status | |||||
| Currently employed | 88 | 77.2 | 100 | 100 | .000 |
| Not employed | 26 | 22.8 | 0 | 0 | .000 |
| Number of children | |||||
| None | 58 | 50.9 | 70 | 70 | .004 |
| At least 1 | 56 | 49.1 | 30 | 30 | .004 |
BUP, former pre-university secondary education; FP, former professional and vocational training; EGB, former compulsory elementary education.
P: comparison of differences of proportions.
The frequencies shown for the marital status, place of residence and pregnancy variables refer to participating couples (57 in the case group and 50 in the control group). The frequencies shown the educational attainment, employment status and number of children refer to individual participants (114 in the case group and 100 in the control group).
We obtained information on the CHDs from the health records. We analysed the most severe diseases with the greatest degree of neurological impairment: diagnosis of transposition of the great arteries in 28.1% (n =16) of the foetuses, ventricular septal defect (IC) in 15.8% (n = 9), tetralogy of Fallot (TOF) in 21.1% (n = 12), atrioventricular septal defect (AVSD) in 10.5% (n = 6).
Lastly, aortic arch hypoplasia/coarctation of the aorta was diagnosed in 24.6% of the foetuses (n = 14) (Table 2).
Congenital anomalies.
| Congenital anomalies (case group) | ||
|---|---|---|
| n | % | |
| TGA | 16 | 28.2 |
| IC | 9 | 15.8 |
| TF | 12 | 21.1 |
| AVSD | 6 | 10.5 |
| Aortic arch hypoplasia/coarctation of the aorta | 14 | 24.6 |
AVSD, atrioventricular septal defect; TF, tetralogy of Fallot; TGA, transposition of the great arteries; IC, Interventricular comunication
Prior to the multivariate analysis, we compared different variables in the case and control groups, which revealed that the groups were similar in terms of most of these variables (Table 1). This reassured us that differences in personal characteristics and circumstances would not affect their responses to the different tools used to assess parental reactions to the diagnosis. We performed a multivariate analysis of the sociodemographic characteristics of participants. We did not identify significant differences during the diagnosis phase. It seems that the demographic characteristics of the participants had no effect on how they responded to the diagnosis of their children.
Results of the BSI-18The intragroup comparisons showed that in both the case and control groups, mothers and fathers obtained similar scores in each subscale as well as the GSI, with a mean of 57.42 in fathers in the case group (SD, 10.315), 61.32 in mothers in the case group (SD, 8.765), 48.43 in fathers in the control group (SD, 7.805) and 52.71 in mothers in the control group (SD, 7.500) (Table 3).
Results of the BSI-18 results for fathers and mothers in the case and control groups.
| Case group | Control group | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fathers (n = 57) | Mothers (n = 57) | Fathers (n = 49) | Mothers (n = 51) | |||||||||||||
| Min | Max | Mean | SD | Min | Max | Mean | SD | Min | Max | Mean | SD | Min | Max | Mean | SD | |
| Som | 43 | 80 | 53.09 | 10.156 | 40 | 81 | 57.40 | 10.351 | 40 | 58 | 46.61 | 5.267 | 40 | 75 | 55.25 | 9.658 |
| Dep | 42 | 78 | 56.28 | 9.449 | 41 | 73 | 59.44 | 7.776 | 41 | 65 | 47.29 | 6.871 | 41 | 69 | 47.37 | 8.047 |
| Anx | 40 | 77 | 59.42 | 10.519 | 38 | 80 | 62.93 | 9.053 | 37 | 67 | 52.22 | 9.141 | 38 | 67 | 52.80 | 8.314 |
| GSI | 37 | 79 | 57.42 | 10.315 | 35 | 78 | 61.32 | 8.765 | 37 | 60 | 48.43 | 7805 | 35 | 69 | 52.71 | 7.500 |
Anx, anxiety; Dep, depression; GSI, global severity index; Som, Somatization; SD, standard deviation.
The analysis revealed clinically significant scores in 35.09% (n = 20) of fathers and 47.37% (n = 27) of mothers in the case group. In comparison, in the control group only 13.73% (n = 7) of mothers had clinically significant scores (Table 4).
Clinical scores for fathers and mothers in the case and control groups.
| Clinical scores | Case group | Control group | ||||||
|---|---|---|---|---|---|---|---|---|
| Fathers | Mothers | Fathers | Mothers | |||||
| n | % | n | % | n | % | n | % | |
| Somatization | 10 | 17.54 | 16 | 28.07 | – | – | 13 | 25.50 |
| Depression | 12 | 21.05 | 21 | 36.84 | 2 | 4.08 | 3 | 5.88 |
| Anxiety | 26 | 45.61 | 35 | 61.40 | 8 | 16.33 | 10 | 19.61 |
| GSI | 20 | 35.09 | 27 | 47.37 | – | – | 7 | 13.73 |
GSI, global severity index.
Within groups, there were significant differences between fathers and mothers in terms of psychological distress (P = .04 in the case group and P = .18 in the control group), somatization (P = .043 in the case group and P < .001 in the control group) and depression (P = .045 in the case group and P = .042 in the control group).
In the fathers in the case group, we found significant correlations between somatization and anxiety (P < .001), somatization and depression (P < .001) and anxiety and depression (P < .001). In the mothers in the case group, we found significant correlations between somatization and anxiety (P < .001) and between anxiety and depression (P < .001). The only correlation found in the control group, in both mothers and fathers, was between anxiety and depression (P < .001) (Table 5).
Correlation in the BSI results of the case and control groups and statistical significance.
| Correlation | Case group | Control group | ||||||
|---|---|---|---|---|---|---|---|---|
| Fathers | Mothers | Fathers | Mothers | |||||
| rho | P | rho | P | rho | P | rho | P | |
| Somatization-depression | .572** | .000 | .309* | .019 | .194 | .183 | .309* | .019 |
| Somatization-anxiety | .491** | .000 | .649** | .000 | .276 | .055 | .649** | .000 |
| Depression-anxiety | .749** | .000 | .660** | .000 | .734** | .000 | .660** | .000 |
Rho, Spearman's correlation coefficient.
We compared groups by means of the Mann-Whitney U test to determine whether there were statistically significant differences between them. We found significant differences in psychological distress (P < .001) and in the subscales measuring somatization (P = .002), depression (P < .001) and anxiety (P < .001).
Results of the DASThe intragroup results show that both mothers and fathers in both the case and control groups tended to perceive the degree of consensus within their relationships as satisfactory. In the case group, 63.3% (n = 36) of fathers and 66.5% (n = 38) of mothers expressed satisfaction with the degree of consensus with their partners. In the control group, the percentages were 73.4% (n = 36) of fathers and 67% (n = 32) of mothers.
The scores for dyadic satisfaction were high for both fathers and mothers in both groups. In the case group, 77% (n = 44) of the fathers and 82.4% (n = 47) of the mothers expressed satisfaction. In the control group, the percentages were 85.7% (n = 42) of fathers and 86.2% (n = 44) of mothers.
Participants in both groups had a positive perception of the degree of cohesion they experienced with their partners. In the case group, 89.4% (n = 51) of fathers and 85.8% (n = 49) of mothers had an idealized view of their cohesion with their respective partners. In the control group, 91.8% (n = 45) of fathers and 94% (n = 48) of mothers reported the same.
Participants in both groups also expressed positive views of their dyadic affective expression. Satisfaction with affective expression was expressed by 70.1% (n = 40) of both fathers and mothers in the case group and 67.4% (n = 33) of fathers and 68.6% (n = 35) of mothers in the control group (Table 6).
Results of the DAS for fathers and mothers in the case and control groups.
| Case group | Control group | |||||||
|---|---|---|---|---|---|---|---|---|
| Fathers | Mothers | Fathers | Mothers | |||||
| n | % | n | % | n | % | n | % | |
| Consensus | ||||||||
| Conflictive | – | – | 1 | 1.8 | – | – | – | – |
| Satisfactory | 36 | 63.3 | 38 | 66.5 | 36 | 73.4 | 32 | 62.7 |
| Idealized | 21 | 36.7 | 18 | 31.7 | 13 | 26.6 | 19 | 37.3 |
| Satisfaction | ||||||||
| Satisfactory | 13 | 23 | 10 | 17.6 | 7 | 14.3 | 7 | 13.8 |
| Idealized | 44 | 77 | 47 | 82.4 | 42 | 85.7 | 44 | 86.2 |
| Cohesion | ||||||||
| Conflictive | – | – | 1 | 1.8 | – | – | – | – |
| Satisfactory | 6 | 10.6 | 7 | 12.4 | 4 | 8.2 | 3 | 6 |
| Idealized | 51 | 89.4 | 49 | 85.8 | 45 | 91.8 | 48 | 94 |
| Affective exp. | ||||||||
| Conflictive | 1 | 1.8 | – | – | – | – | – | – |
| Satisfactory | 16 | 28.1 | 17 | 29.9 | 16 | 32.6 | 16 | 31.4 |
| Idealized | 40 | 70.1 | 40 | 70.1 | 33 | 67.4 | 35 | 68.6 |
Participants in both groups had idealized views of their relationships: 57.7% of fathers and 50.4% of mothers in the case group and 73.7% of fathers and 66.6% of mothers in the control group (Table 7).
The comparison of mothers and fathers within each group revealed significant differences between fathers and mothers in the control group in the perceived cohesion (P = .024).
In fathers in the case group, we found statistically significant correlations between consensus and cohesion (P < .001) and between consensus and affective expression (P < .001). In mothers in the case group, we found statistically significant correlations between consensus and satisfaction (P < .001) and between consensus and affective expression (P < .001). The correlations found in fathers in the control group were between consensus and cohesion (P = .000) and between satisfaction and affective expression (P < .001). In mothers in the control group, there were correlations between consensus and satisfaction (P = .004), consensus and cohesion (P < .001) and consensus and affective expression (P = .009) (Table 8).
Correlation between DAS subscales and statistical significance.
| Correlation | Case group | Control group | ||||||
|---|---|---|---|---|---|---|---|---|
| Fathers | Mothers | Fathers | Mothers | |||||
| rho | P | rho | P | rho | P | rho | P | |
| Consensus-Satisfaction | .311* | .018 | .471** | .000 | .269 | .062 | .396** | .004 |
| Consensus-Cohesion | .458** | .000 | .305* | .021 | .480** | .000 | .473** | .000 |
| Consensus-Affective exp. | .449** | .000 | .464** | .000 | .311* | .029 | .361** | .009 |
| Satisfaction-Cohesion | .287* | .031 | .138 | .305 | .209 | .150 | .252 | .075 |
| Satisfaction- Affective exp. | .217 | .105 | .325* | .014 | .489** | .000 | .271 | .054 |
| Cohesion- Affective exp. | .168 | .211 | .255 | .056 | .111 | .450 | .101 | .479 |
Rho: Spearman's correlation coefficient.
We found statistically significant differences between the case and control groups in the cohesion subscale of the DAS (P = .004).
Results of the FACES-IIIThe intergroup comparison shows that in the case group, the greatest proportion corresponded to fathers that perceived their family system as chaotically connected (29.8%; n = 17), followed by those that perceived the system as chaotically enmeshed (21.1%; n = 12). According to the circumplex model, these are midrange and unbalanced family systems. Mothers in the case group were most likely to perceive their families as chaotically enmeshed (22.8%; n = 13), followed in frequency by mothers perceiving the family as chaotically connected (21.1%; n = 12), systems considered midrange and unbalanced in the circumplex model. In the control group, fathers most frequently perceived the family as chaotically connected (49%; n = 24), a midrange family system in the grid. Mothers also most frequently perceived their families as chaotically connected (31.4%, n = 16), followed by chaotically enmeshed (19.6%; n = 10), systems placed in the midrange and unbalanced areas of the circumplex model (Table 9, Fig. 2).
Frequency distribution of the 16 types of family dynamics in the case and control groups.
| Family dynamics | Case group | Control group | ||||||
|---|---|---|---|---|---|---|---|---|
| Fathers (n = 57) | Mothers (n = 57) | Fathers (n = 49) | Mothers (n = 51) | |||||
| n | % | n | % | n | % | n | % | |
| Chaotically disengaged | 1 | 1 | 1 | 1.8 | 0 | 0 | 0 | 0 |
| Chaotically separated | 2 | 3.5 | 4 | 7 | 4 | 8.2 | 5 | 9.8 |
| Chaotically connected | 17 | 29.8 | 12 | 21.1 | 24 | 49 | 16 | 31.4 |
| Chaotically enmeshed | 12 | 21.1 | 13 | 22.8 | 3 | 6.1 | 10 | 19.6 |
| Flexibly disengaged | 0 | 0 | 0 | 0 | 1 | 2 | 0 | 0 |
| Flexibly separated | 6 | 10.5 | 4 | 7 | 3 | 6.1 | 6 | 11.8 |
| Flexibly connected | 6 | 10.5 | 8 | 14 | 6 | 12.2 | 6 | 11.8 |
| Flexibly enmeshed | 3 | 5.3 | 2 | 3.5 | 2 | 4.1 | 2 | 3.9 |
| Structurally disengaged | 0 | 0 | 1 | 1.8 | 0 | 0 | 0 | 0 |
| Structurally separated | 2 | 3.5 | 1 | 1.8 | 0 | 0 | 2 | 3.9 |
| Structurally connected | 3 | 5.3 | 4 | 7 | 5 | 10.2 | 3 | 5.9 |
| Structurally enmeshed | 0 | 0 | 2 | 3.5 | 1 | 2 | 1 | 2 |
| Rigidly separated | 3 | 5.3 | 3 | 5.3 | 0 | 0 | 0 | 0 |
| Rigidly enmeshed | 2 | 3.5 | 2 | 3.5 | 0 | 0 | 0 | 0 |
The comparative analysis did not find any significant differences based on sex in either group.
As can be seen in Table 10, most members in both groups perceived their family dynamics as mid-range.
Frequencies of the three types of family systems.
| Family system | Case group | Control group | ||||||
|---|---|---|---|---|---|---|---|---|
| Fathers (n = 57) | Mothers (n = 57) | Fathers (n = 49) | Mothers (n = 51) | |||||
| n | % | n | % | n | % | n | % | |
| Balanced | 17 | 29.8 | 17 | 28.1 | 14 | 28.5 | 17 | 33.4 |
| Mid-range | 25 | 43.9 | 24 | 42.2 | 32 | 65.3 | 24 | 47.1 |
| Unbalanced | 15 | 26.4 | 16 | 28.1 | 3 | 6.1 | 10 | 19.6 |
The intergroup comparison revealed significant differences in the perceived family dynamics between couples expecting a child with a CHD and couples expecting a healthy child (P = .029).
DiscussionThe findings of our study illustrate how mothers and fathers cope with the diagnosis of a serious illness like CHD in an expected child.
Several researchers have described parental reactions after being informed of the diagnosis of a child.34 Parents are forced to handle the transition to parenthood and the diagnosis of congenital heart disease in the child at the same time, in addition to medical, economic, social, family, emotional and other aspects related to the diagnosis.9 Previous studies16,17 have described the crisis that the diagnosis in the child causes in the family, marked by significant changes in the relationships between family members, especially between the partners in the couple and the child with the disease. Furthermore, marital cohesion may also be affected to the extent that all the attention focuses on the sick child, with a deleterious impact on the satisfaction in the couple and the achievement of shared goals.13,14 Families develop various coping strategies and adapt to the new situation with varying degrees of success.16
The results of the BSI-18 show that most parents in both groups had scores that were not clinically relevant. In other words, their GSI scores were below the clinical threshold of 63.28 This differed from the results of previous studies10,11 that found that parents, when confronted with a critical situation of this nature, tend to display high levels of anxiety due to fears concerning the potential consequences of the disease, and also tend to have high scores for psychological distress in response of these serious diagnoses. We did not find significant differences between the case and control groups. This might be due to the questionnaires having been administered immediately after couples had been informed of the diagnosis. The expectant parents were experiencing a moment of uncertainty and confusion, and perhaps they had not fully assimilated the information they had received. This is only to be expected, since the diagnosis is upsetting and places the family in uncharted territory, as they are not familiar with the processes they will undergo with their child and with the likely course of the congenital disease.10,11,15
We would also like to highlight that, while the results were not clinically significant, women in both the case and control groups were more likely to score higher on the GSI. Pregnant women frequently experience hormonal imbalances, which can affect both their physical state and their mood. The analysis showed significant differences between the subscales, but we found correlations in both mothers and fathers in both groups between anxiety and depression. Specifically, higher levels of depression were associated with lower levels of anxiety and vice versa. In addition, we found significant correlations between somatization and anxiety and between somatization and depression in fathers in the case group, so that higher levels of somatization were associated with lower levels of anxiety and depression, and vice versa. Thus, we may conclude that men and women respond and cope differently when confronted with the same stressor, in this case the diagnosis of CHD in an expected child.26
The results of the assessment of dyadic adjustment using the DAS questionnaire showed that most mothers and fathers in both the case and control groups had an idealized perception of the adjustment in their relationships, as most respondents had scores over 125.30 It is worth noting that in both groups, regardless of sex and of the correlation or differences between groups, the scores for the cohesion subscale were significantly higher compared to the rest of the subscales. We also ought to comment on the idealized view couples had of their relationships. This finding also differed from a previous study13 that focused specifically on the impact of these situations on the cohesion of couples, as they often have to focus their attention on the child and partners may end up neglecting one another. A possible explanation of these differences is that the relationships of the couples in our study may have been thriving because they were in the process of expanding their families. This implies a degree of harmony and an idealized relationship, which may remain intact despite the received diagnosis.
In both groups, the perceptions of parents as to their family dynamics fell into the midrange category. Applying Olson’s circumplex model, their family systems would be categorized as mid-range or unbalanced, as participants frequently scored into the chaotically connected and chaotically enmeshed family types. From this analysis, we can conclude that these expectant parents had a very positive perception of their own adaptability and family cohesion in the prenatal stage. In other words, they believed that they were willing and able to adapt to any changes that could arise in their family or social circle. These couples also tended to be at a stage in their life cycles at which the interests and goals of each partner complemented those of the other.
Thus, our findings confirmed some of our initial hypotheses. For example, there were significant differences based on sex within both the case and control groups, and there were differences between the groups in the overall level of psychological distress. When it came to dyadic adjustment, we only found significant differences between mothers and fathers in the control group, with no differences between groups. Our findings did not corroborate our hypothesis regarding family dynamics.
We ought to underscore that each individual copes with and comes to terms with the diagnosis of a severe disease in a child in a different way, with different processes and different mechanisms. Since families in this study were in the early stage after receiving the diagnosis, monitoring the changes in their perception of the disease and in psychological distress, dyadic adjustment and family dynamics would be of great interest. These families are at the start of a highly complex process in which the children will be hospitalized, separated from their families, and subjected to one or more risky surgical procedures that can have a range of consequences in their outcomes. These couples are not yet fully aware of all of this. Thus, it is important to provide expectant parents who have been given prenatal diagnoses of CHD with effective support and psychological guidance to help them understand the information they receive and the processes they are likely to experience with their child over the first days, weeks and months post birth. This will help them cope in the critical junctures they will encounter along the way and manage the situation in the best possible way as individuals, couples and families.
Another salient finding was that when the couples received the diagnosis, they all made the decision to continue with the pregnancy despite knowing that the child would have a chronic condition. The fact that they were able to accept the disease points to strengths and skills that may help them achieve a solid balance as individuals, couples and families going forward as the disease follows its course. These abilities may be an asset as they confront both the transition to parenthood and the diagnosis of CHD in their child.8
The results of the administered questionnaires provide a basic outline of the impact of the prenatal diagnosis CHD on the family. These results may be relevant for professionals seeking to offer effective psychological support and guidance to parents. This, in turn, can help parents in these situations to understand and accept the information they receive and improve their coping skills, their ability to manage the experiences associated with the disease and their quality of life.
From this point, we can continue to assess the evolution of the participants based on the outcomes of disease in their children, and to formulate new questions for future research and development of preventive and treatment strategies.
Conflict of interestsThe authors declare that they have no conflict of interest.
Please cite this article as: Salvador M, Vilaregut A, Moyano R, Ferrer Q, Gòmez O, Moratalla T, et al. Malestar psicológico, ajuste diádico y dinámica familiar tras el diagnóstico prenatal de cardiopatía congénita. An Pediatr (Barc). 2022;97:179–189.