Foetus in foetu (FIF) is a rare congenital malformation.1 It has an estimated incidence of 1:500,000 live births and about 200 cases have been published in the literature.2 Its aetiopathogenesis involves abnormal embryogenesis in a monochorionic diamnotic pregnancy in which one foetus becomes enclosed in the other.
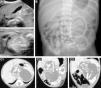
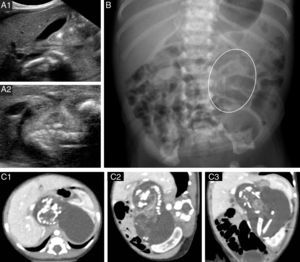
We present the case of a full-term male newborn with an abdominal mass detected by ultrasound at 25 weeks of gestation. The physical examination was unremarkable. He had elevated levels of ferritin, lactate dehydrogenase (LDH), ¿-human chorionic gonadotropin (¿-HCG) and alkaline phosphatase (AP), while test results were normal for the complete blood count, renal function, ¿-foetoprotein and carcinoembryonic antigen. Urine catecholamine values were normal. Abdominal ultrasonography revealed a well-delineated retroperitoneal lobulated solid mass surrounded by fluid that contained linear calcifications resembling bone structures (Fig. 1A). Abdominal radiography showed mature bone structures resembling long bones in the left flank (Fig. 1B). Computed tomography (CT) of the abdomen confirmed these findings and provided detailed information on the relationship of the mass with important vascular and visceral structures (Fig. 1C). The surgical exploration, performed at 5 days of life, revealed an encapsulated mass. Sectioning of this mass yielded a clear fluid and a foetiform mass with four limbs and a rudimentary umbilical cord measuring 8mm that extended into a membrane-like tissue that corresponded to the amnion (Fig. 2). The anatomopathological study described a foetiform structure covered in skin with arrhinia, anophthalmia, acrania, and rachischisis. A tongue, tooth buds, trachea, oesophagus, intestine, bladder, pancreatic and testicular tissue, adrenal gland, spinal cord with bone marrow, and pelvis were identified. Malignancy was ruled out. At 48h post-surgery, the patient had abdominal distension and elevated serum inflammatory markers, and radiography of the abdomen showed pneumatosis intestinalis. Necrotising enterocolitis was suspected and antibiotic therapy initiated. The surgical reintervention confirmed ischaemic necrosis of the terminal ileum extending to the ascending colon, secondary to the ligation of a branch of the superior mesenteric artery. Right hemicolectomy, distal ileostomy, and transverse colostomy were performed. The postoperative period was uneventful, and the levels of ferritin, LDH, ¿-HCG and AP normalised. Bowel reconstruction was performed 3 months later by end-to-end anastomosis, with no complications. The clinical outcome was excellent at 12 months, and the patient showed appropriate height and weight gains.
(A) Abdominal ultrasound. (B) Plain radiograph of the abdomen; the oval shape marks the location of the longitudinal bone structures. (C) Abdominal CT scan: well-delineated mass containing calcified structures that correspond to the long bones and vertebrae of the FIF; (C1) axial plane, (C2) sagittal plane; (C3) oblique plane.
(A) 3D reconstruction, volume-rendered left oblique view: (A1) Bone structure of the FIF; (A2) part of the left lobe of the liver was eliminated to better visualise the mass. Bone structures of the FIF, with the same density as the patient's bone structures. The image shows anterior and cranial displacement of the splenic vein (¥). Anterior and cranial displacement of the pancreas (not visible). The left kidney is pushed laterally and anteriorly (*) and the left renal vein (*) is elongated and in an anterior position. The coeliac artery (not shown) is elongated and displaced cranially over the mass. The inferior vena cava (#) and the superior mesenteric artery ($) are pushed laterally to the right. (B) Postoperative specimen: foetiform mass with umbilical cord.
FIF is a rare condition that is easily identified if its particular radiological features are known.3 It is hypothesised that it results from unequal division of the blastocoele in a monozygotic twin gestation, following which the smaller twin (the parasitic foetus or FIF) develops inside of the host foetus.1 The FIF usually has a fluid-filled capsule that corresponds to the amniotic sac and fluid. It has the appearance of a developing foetus with varying degrees of complexity. It may have developed structures of the nervous system or the gastrointestinal or urinary tracts and have well-differentiated long bones; the presence of vertebral bodies is pathognomonic; and the presence of a heart or brain is rare.4 In 80% of the described cases, the location of the FIF is the retroperitoneal region, but they can be found in the thorax, brain, scrotum, and even the oral cavity. Usually there is a single parasite twin, but cases of multiple FIF have been described.
The typical clinical presentation is a palpable mass, usually in the abdomen, but the initial presentation can consist of symptoms secondary to FIF development. Most cases of FIF are described during childhood.
The diagnosis of FIF is based on imaging studies. Prenatal ultrasound may identify a cystic mass with solid components or calcifications.5 After birth, plain radiography may reveal bone structures; while failure to detect such structures does not rule out the diagnosis, the presence of vertebral bodies is pathognomonic. CT offers a detailed view of the structures that compose the mass, its vascular anatomy, and its relationship with the surrounding organs, important information for surgical management. Magnetic resonance imaging is gaining importance due to its high tissue contrast and spatial resolution, and it does not require exposure to radiation or intravenous contrast.6 Some publications have described instances of elevated serum levels of ¿-foetoprotein and/or ¿-hCG in association with this disease.2
The main condition to consider in the differential diagnosis is highly differentiated teratoma. The presence of vertebral bodies in the FIF indicates that the parasitic foetus developed up to the primitive streak stage when the notochord forms, which is the precursor of the spinal cord. In comparison, teratoma forms by the uncontrolled growth of pluripotent cells without organogenesis or vertebral segmentation. Furthermore, unlike teratoma, FIF usually does not recur and it rarely becomes malignant.
While FIF is a benign disorder, the evolution of the mass can compromise surrounding structures, and surgical resection is therefore the first line of treatment. Likewise, monitoring the levels of serum ¿-HCG and ¿-foetoprotein and ultrasound follow-up of patients for two years are also recommended.2
Please cite this article as: Herranz Barbero A, Collazo Vallduriola I, Margarit Soler A, Muchart López J, Castañón García-Alix M. Diagnóstico prenatal de masa abdominal. Revisión del foetus in fetu. An Pediatr (Barc). 2015;82:101–103.