Severe premature constriction of the foetal ductus arteriosus is a rare condition that may result in serious foetal and neonatal morbidity. Its development is usually associated with maternal exposure to nonsteroidal anti-inflammatory drugs,1 a polyphenol-rich diet2 or a tortuous ductus arteriosus,3 although there are cases in which the cause is not identified (idiopathic constriction of the ductus arteriosus).4
Since this is an important phenomenon, we present the characteristics of the pregnant women diagnosed with premature intrauterine ductus arteriosus constriction in our department.
To that end, we performed a retrospective descriptive study by reviewing the medical records of the pregnant women who received care in the paediatric cardiology department of our hospital in the past three years (2011–2013) in whom echocardiography revealed the presence of premature constriction of the ductus arteriosus, and also of the subsequent evolution of the newborns.
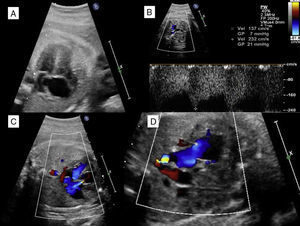
We found evidence of premature constriction of the ductus arteriosus in 7 pregnant women, all of who were diagnosed in the third trimester at a mean gestational age of 35.4 weeks. Table 1 shows the characteristics of the pregnant women. The outcomes were favourable when the triggering factor was removed (5/7). One of the foetuses had a severe restriction of blood flow through the ductus arteriosus with dilation and dysfunction of the right heart chambers and severe tricuspid regurgitation (Fig. 1) that persisted in the neonatal period and was observed to have normalised in subsequent follow-up office visits.
Characteristics of mothers and babies born with restricted blood flow through the ductus arteriosus.
| Gestational age | Possible trigger | Impact on foetal haemodynamics | Maternal disease | Ethnicity | Disease in the newborn |
|---|---|---|---|---|---|
| At diagnosis | |||||
| 35.4 | Grapes | Yes | No | Caucasian | No |
| 35.4 | Paracetamol | No | No | Caucasian | No |
| 32.0 | Acetylsalicylic acid | No | Antiphospholipid syndrome | Caucasian | No |
| 35.0 | Hydroxychloroquine | No | Lupus | Latin American | No |
| 35.0 | Diclofenac and ibuprofen | Yes | Low back pain | Caucasian | Dilatation of right heart chambers and tricuspid regurgitation ++ |
| 35.6 | No | No | No | Arabic | No |
| 36.4 | No | No | No | Caucasian | No |
Severe premature constriction of the ductus arteriosus. (A) Four-chamber view showing dilatation of the right heart chambers with the foramen ovale flap bulging into the left atrium. (B) Doppler of the ductus arteriosus revealing a continuous blood flow with increased systolic and diastolic flow velocities. (C) Severe tricuspid regurgitation. (D) Three-vessel view showing a reduced ductal diameter.
Premature constriction of the foetal ductus arteriosus has been well described in the literature, although there are few published articles on the subject, which may be due to underdiagnosis of this condition. It must be suspected, particularly in the third trimester, if foetal echocardiography reveals dilatation and dysfunction of the right ventricle, tricuspid regurgitation and increased flow velocity in the ductus arteriosus measured by Doppler in the absence of structural heart disease.4 Identifying the possible cause of the condition requires taking a detailed history with particular emphasis on the diet of the mother and any medications taken during pregnancy.5,6 In our series, the type of maternal exposure most frequently associated with this condition corresponded to nonsteroidal anti-inflammatory drugs, as described in the literature,1 although we found others such as exposure to hydroxychloroquine, which had not been described until now.
The early diagnosis of premature constriction of the foetal ductus arteriosus and the identification of its aetiology are essential in order to reverse or minimise haemodynamic alterations, as progression of this condition may lead to heart failure and foetal death.
Please cite this article as: Ayerza Casas A, Jiménez Montañés L, López Ramón M, Lerma Puertas D, García de la Calzada MD. Constricción precoz del ductus arterioso. An Pediatr (Barc). 2015;82:193–195.