Thousands of children and adolescents seek care each year in paediatric emergency departments in Spain following exposure to potentially toxic substances,1 adding to others that seek care in primary care or urgent care clinics and call the toxicologic emergency line of the Instituto Nacional de Toxicología (National Toxicology Institute) of Spain.
Broadly speaking, there are 5 types of toxic substance exposures in paediatric patients.1 Two are characteristic of young children, 2 of older children and adolescents, and the last one of any age. Each has its own epidemiological characteristics that affect both the management of episodes and their prevention.
The most frequent type managed in paediatric emergency departments is unintentional ingestion of medication (most frequently benzodiazepines) and dosing errors (especially involving paracetamol). It usually happens in the home and is most frequent in children about 2 years of age, while associated fatalities are most frequent in children younger than 1 year. Outcomes tend to be good, as the ingested amount is usually small and the delay in seeking medical care short. However, some substances are toxic in very small amounts. In the current issue of Anales de Pediatría, Colom et al. warn us of the enduring problem of unintentional poisoning with cough and cold medication.2 As the authors noted insightfully, these are drugs that have not been found to be useful in scientific research and, in some cases, can cause severe or even fatal poisoning. Paediatricians need to take this into account when prescribing these medications. It is important to remember, even as the associated mortality decreases, that poisonings constitute the fifth leading cause of death due to unintentional injury in the European region of the World Health Organization, although Spain is in the group of countries with the lowest frequencies.
The second type of poisoning corresponds to the unintentional ingestion of household chemicals (chiefly detergents and caustic substances) and cosmetic products. This type is more frequent in children aged less than 2 years. It very rarely results in a fatality, but the ingestion of some products can cause significant sequelae, especially at the level of the oesophagus. A substantial percentage of these poisonings involve products that are within reach of children or that are not kept in the original container (especially in cases of unintentional caustic ingestion in children aged more than 4 years). It is important to correct these habits in the storage of potentially toxic substances.
Although it is not included in either of the 2 types discussed above, unintentional ingestion of illicit drugs kept in the home by young children also deserves attention on account of the significant increase in the frequency of these events in recent years.3 Illicit drug use by parents or caregivers is directly associated with this increase, and its detection is one of the aspects that must be taken into account in the management of young children with altered level of consciousness. Serious consideration should also be given to discussing this issue with parents in the routine healthy child visits conducted in the first 2 years of life.
Older children and adolescents most frequently seek care for 2 other types of poisoning that are clearly distinct.
On one hand, recreational alcohol consumption by patients of either sex, usually in the street or in bars, experienced a significant increase in the first decade of this century, after which it stabilised.4 Alcohol use is accompanied by consumption of illicit drugs, chiefly cannabis, in up to 20% of patients that seek care in paediatric emergency services.
On the other hand, the frequency of intentional drug poisoning with suicidal intent is increasing alarmingly in the paediatric population. It is most frequent in girls who consume the drugs at home (most frequently benzodiazepines or paracetamol), although a high percentage ingest a combination of drugs. Many of these patients have made previous visits to the emergency department for the same reason, and in some cases they have never undergone a psychiatric evaluation. Although these poisonings are rarely fatal, approximately 90% of patients who make suicide attempts have psychiatric disorders, in most cases mood disorders. A previous suicide attempt is, along with the presence of a psychiatric disorder, a key risk factor for future suicide attempts. The case published in the current issue of Anales de Pediatría by Gonzalez-Lago et al. perfectly summarises the presentation of these patients, warning of the possibility of an insidious course.5 Delays in seeking care, typical of this type of poisonings, render gastrointestinal decontamination methods ineffective and make life support measures and antidotes the cornerstone of management in these patients. There has been a substantial increase worldwide in this type of poisonings during the SARS-CoV-2 pandemic. In Spain, paediatric emergency care encounters related to poisoning with suicidal intent increased during the lockdown period, but the steepest increase occurred in the second year of the pandemic. The characteristics of these poisonings have not changed, as during the pandemic there was also a majority of cases in female patients, who ingested drugs, chiefly benzodiazepines and analgesics, and one third of cases involving more than one drug. This underscores the importance of implementing urgent measures to promote, safeguard and care for the mental health of children and adolescents, including both universal measures and interventions targeting high-risk groups. Different agents should be involved in developing these measures, including institutions, mental health experts and paediatricians.
Last of all, the last type of poisoning corresponds to substance inhalation, mainly carbon monoxide, in the home, and at any age. Cases are usually associated with defective combustion systems and account for approximately 5% of encounters related to exposure to potentially toxic substances in paediatric emergency departments.
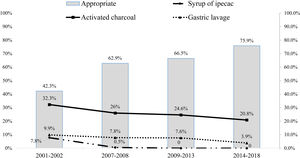
Overall, the management of these children and adolescents in paediatric emergency departments in Spain has markedly improved in recent decades. At present, gastrointestinal decontamination procedures and antidote administration are performed more appropriately (Fig. 1), which is probably related to the actions implemented by the members of the Toxicology Observatory of the Sociedad Española de Urgencias de Pediatría (Spanish Society of Paediatric Emergency Medicine). In a large proportion of cases, unintentional medication or household chemical ingestions in young children do not cause problems at the consumed amounts. This is the case of children that appear well, present no signs or symptoms associated with the ingestion, when the involved substance is clearly identified and is not one that would cause delayed toxicity. If all these conditions are met, an intervention is not generally needed, other than insisting on the importance of preventive measures. Parents and caregivers tend to be more receptive to guidance at such times compared to other visits to the paediatrician.
Poisonings are a significant public health problem in Spain. It is our collective responsibility as a society, including paediatricians, to develop strategies to reduce their impact on children and adolescents.