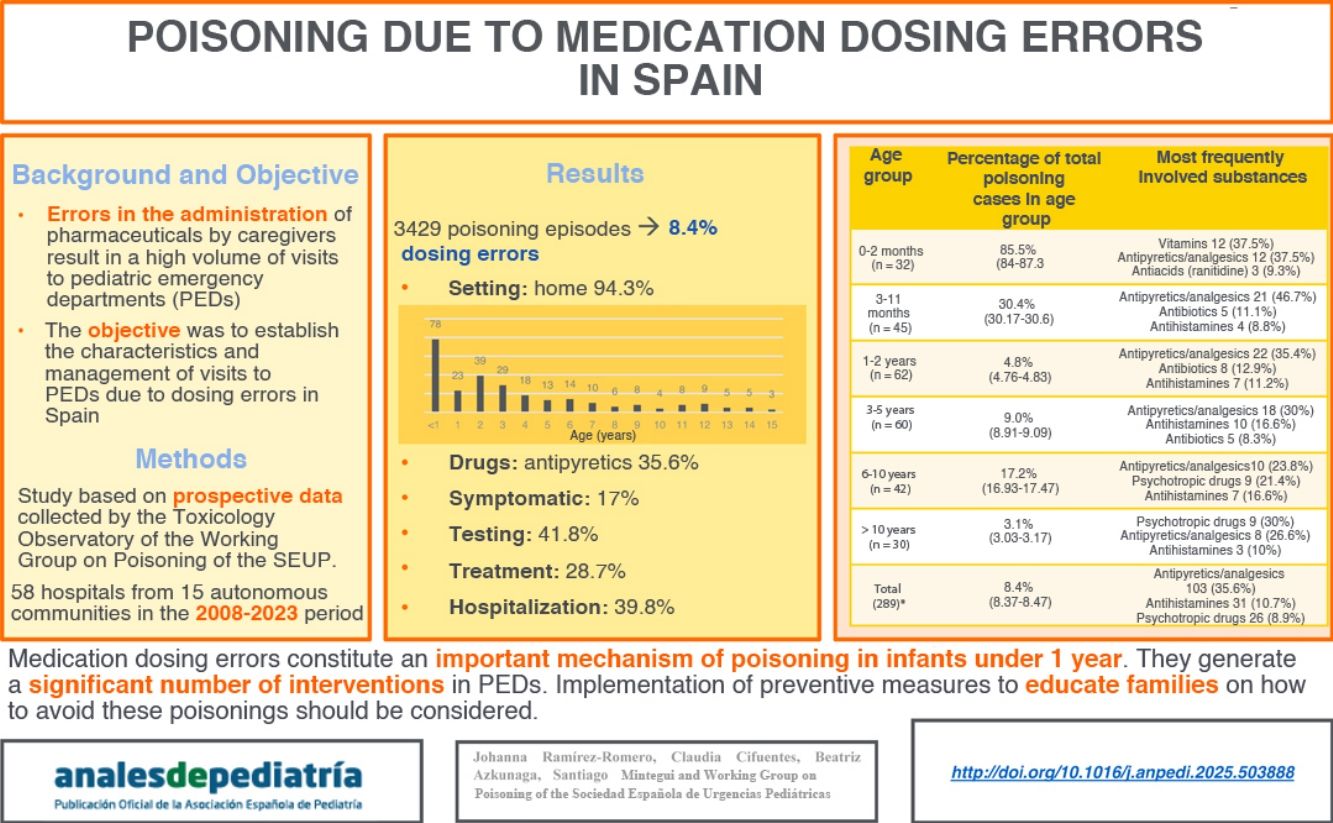
Dosage errors are a common mechanism of poisoning in childhood. The aim of this study was to analyze the characteristics and management of poisoning secondary to dosage errors in pediatric emergency departments (EDs) in Spain.
MethodologyStudy based on a prospective register of poisonings documented in 58 Spanish EDs participating in the Toxicology Surveillance Observatory of the Spanish Society of Paediatric Emergency Medicine (SEUP) between 2008 and 2023.
ResultsThe register documented 3429 episodes of exposure to toxic substances, of which 289 (8.4%) were medication dosing errors, with a vast majority occurring in the home setting. Seventy-eight (27.0%) occurred in children aged less than 1 year (amounting to 37.9% of poisonings in this age group and 85.0% of poisonings in infants aged less than 3 mo). Overall, the most commonly involved medications were antipyretics/analgesics (35.6%, mainly paracetamol), with significant differences depending on patient age. Forty-nine of the patients (17.0%) were symptomatic, 118 (41.8%) underwent additional testing, 83 (28.7%) received treatment, and 115 (39.8%) were admitted to the ED observation unit or to hospital. All had favorable outcomes.
ConclusionsMedication dosing errors constitute an important mechanism of poisoning, especially in children aged less than 1 year, leading to a significant number of interventions in EDs. Preventive measures aimed at educating families to avoid these poisonings should be considered.
Los errores de dosificación son un mecanismo de intoxicación relativamente frecuente en la infancia. El objetivo del estudio es analizar su tipología y manejo en los servicios de urgencias pediátricas (SUP) de España.
MetodologíaEstudio basado en el registro prospectivo de las consultas por intoxicaciones registradas en los 58 servicios de urgencias miembros del Observatorio de Toxicología del Grupo de Trabajo de Intoxicaciones de la Sociedad Española de Urgencias de Pediatría entre 2008 – 2023.
ResultadosSe registraron 3.429 episodios correspondientes a exposiciones a sustancias tóxicas, 289 (8.4%) por errores en la dosificación de un fármaco, la inmensa mayoría en domicilio. Setenta y ocho (27.0%) eran menores de 1 año (37.9% de las intoxicaciones en este grupo de edad y 85.0% de las intoxicaciones en menores de 3 meses). Globalmente, los fármacos más implicados fueron los antitérmicos/analgésicos (35.6%, sobre todo paracetamol), con diferencias significativas según la edad del paciente. Presentaron síntomas 49 (17.0%), se le realizó alguna prueba complementaria a 118 (41.8%), recibieron tratamiento 83 (28.7%) y 115 (39.8%) ingresaron en la Unidad de Observación de Urgencias o planta hospitalaria. Todos evolucionaron bien.
ConclusionesLos errores de dosificación de fármacos son un importante mecanismo de intoxicación sobre todo en menores de 1 año, generando un importante número de intervenciones en los SUP. Debe considerarse la articulación de medidas preventivas orientadas a la educación de las familias para evitar estas intoxicaciones.
Poisoning continues to be a major health problem in the pediatric population. Approximately one in every 250 to 300 patients who visit pediatric emergency departments (PEDs) do so following exposure to a potentially toxic substance.1
Pediatric patients are particularly vulnerable to exposure to toxic substances due to the immaturity of some organs, a lower body weight, and lower physiological reserves. The prognosis and outcome of these patients depend largely on the type of substance involved in the poisoning, the underlying mechanism and the management by health care providers.2 Therefore, knowing the typical characteristics of poisoning-related visits is essential to ensuring effective care in emergency departments.
In our region, ingestion of a pharmaceutical is the most frequent pattern of poisoning observed in PEDs, particularly among cases of unintentional poisoning in young children.3,4 Numerous studies in the literature describe the characteristics of unintentional poisonings due to the exploratory ingestion of pharmaceuticals by children, motivated by their innate curiosity.5–7 In addition, while less frequent than unintentional ingestions, errors in the administration of medication by parents or caregivers also result in a substantial number of visits to the PED.1,8 In fact, the United States poison centers receive more than 60 000 calls a year for out-of-hospital medication errors in children aged less than 6 years, which amounts to approximately one child every 8 min.9 In spite of this, there are no studies in the literature specifically analyzing cases of poisoning due to drug administration errors in Spain.
The aim of our study was to describe the characteristics and management of medication dosing errors managed in PEDs in Spain.
Material and methodsStudy designWe conducted a study based on a prospective register of the poisonings documented in 58 PEDs in Spain that participate in the Toxicology Observatory of the Working Group on Poisoning of the Sociedad Española de Urgencias de Pediatría (SEUP, Spanish Society of Pediatric Emergency Medicine) between 2008 and 2023.
Data collectionDuring the study period, we recorded the visits related to exposure to potentially toxic substances managed in the PEDs on the 13th day of each month from 2008 to December 2014, and, from January 2014, the 13th, 14th and 15th of each month using online questionnaires. At present, the Toxicology Observatory includes 58 PEDs from 15 autonomous communities in Spain. Of this total, thirty-two manage patients through age 13 years and eleven manage patients through age 17 years.
Participating PEDs reported the total number of visits and the details of all the visits related to exposure to potentially toxic substances for which they obtained informed consent made on the 13th of each month through December 2013 and, from January 2014, on the 13th, 14th and 15th of each month by completing the online questionnaire that could be accessed through the Google Drive platform. The data collection method has been described in a previous article in this journal.7 The questionnaires were completed by the physicians in charge of the patient after discharge from the PED in patients who did not require inpatient care and after hospital discharge in patients who required admission.
The questionnaire used to collect data on each patient included the following sections: date of the episode, sending hospital, age, sex, toxic substance, cause of poisoning, location and type of storage of the potentially toxic substance, history of similar episodes in the patient or other family members, prehospital assessment or treatment, person accompanying the patient to the PED, means of transport, time from exposure to the toxic substance to arrival at the PED, symptoms and signs, additional tests performed, treatment received at the PED, patient destination after discharge from PED and patient outcomes.
Appendix B lists the hospitals included in the study.
Statistical analysisThe statistical analysis was performed with the software IBM SPSS Statistics for Windows, version 24.0 (IBM Corp. Armonk, NY, USA). We summarized the data using the mean and standard deviation for quantitative variables and percentages for categorical variables. Quantitative variables were compared using the Student t test and categorical variables with the χ2 and Fisher exact tests. We considered P values of less than 0.05 statistically significant. The study was approved by the Clinical Research Ethics Committee of the Basque Country.
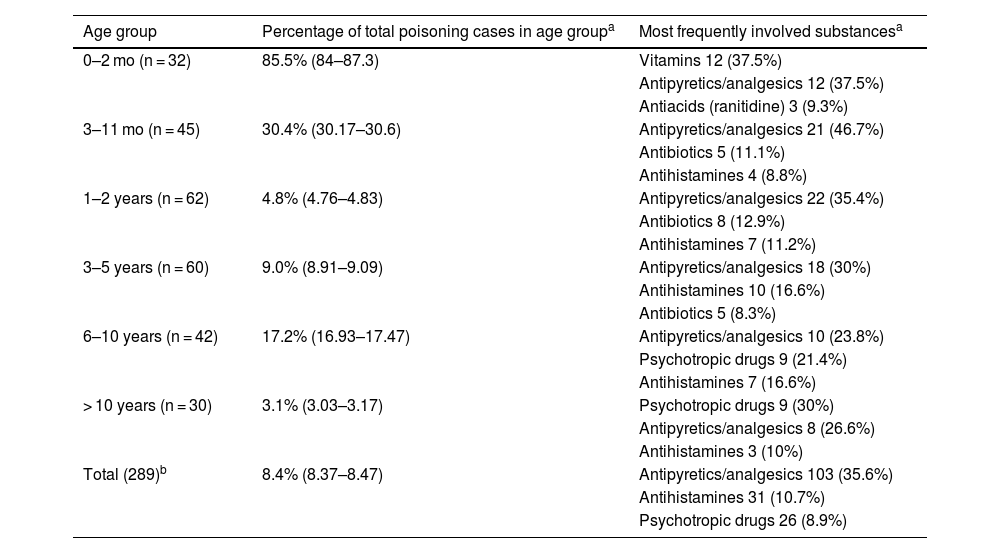
ResultsDurante the period under study, participating PEDs recorded 3429 episodes of exposure to potentially toxic substances, of which 289 (8.4%) resulted from error in the administration of a pharmaceutical. These errors were more frequent in infants aged less than 1 year. Seventy-eight of these episodes occurred in infants, accounting for 27% of the cases involving dosing errors. Thus, dosing errors resulted in 37.9% of poisonings recorded in infants under 1 year. In addition, 32 of the poisonings secondary to dosing errors occurred in infants aged less than 3 mo, amounting to 85.5% of the poisoning episodes recorded in this age group (Table 1).
Incidence of dosing errors relative to the total number of recorded poisonings and most frequently involved drugs, by age group.
| Age group | Percentage of total poisoning cases in age groupa | Most frequently involved substancesa |
|---|---|---|
| 0–2 mo (n = 32) | 85.5% (84–87.3) | Vitamins 12 (37.5%) |
| Antipyretics/analgesics 12 (37.5%) | ||
| Antiacids (ranitidine) 3 (9.3%) | ||
| 3–11 mo (n = 45) | 30.4% (30.17–30.6) | Antipyretics/analgesics 21 (46.7%) |
| Antibiotics 5 (11.1%) | ||
| Antihistamines 4 (8.8%) | ||
| 1–2 years (n = 62) | 4.8% (4.76–4.83) | Antipyretics/analgesics 22 (35.4%) |
| Antibiotics 8 (12.9%) | ||
| Antihistamines 7 (11.2%) | ||
| 3–5 years (n = 60) | 9.0% (8.91–9.09) | Antipyretics/analgesics 18 (30%) |
| Antihistamines 10 (16.6%) | ||
| Antibiotics 5 (8.3%) | ||
| 6–10 years (n = 42) | 17.2% (16.93–17.47) | Antipyretics/analgesics 10 (23.8%) |
| Psychotropic drugs 9 (21.4%) | ||
| Antihistamines 7 (16.6%) | ||
| > 10 years (n = 30) | 3.1% (3.03–3.17) | Psychotropic drugs 9 (30%) |
| Antipyretics/analgesics 8 (26.6%) | ||
| Antihistamines 3 (10%) | ||
| Total (289)b | 8.4% (8.37–8.47) | Antipyretics/analgesics 103 (35.6%) |
| Antihistamines 31 (10.7%) | ||
| Psychotropic drugs 26 (8.9%) |
Of the 289 poisoning cases, 160 occurred in boys (55.4%). In three cases (1.0%), it was not the first time that the child received the wrong dose of a pharmaceutical: of valproic acid in a patient aged 3 years, of metamizole in patient aged 4 years and of risperidone in a patient aged 12 years. In 18 cases (6.2%) there was a previous history of dosing error in another member of the family.
Overall, the most frequently involved drugs were antipyretics/analgesics (n = 10 [35.6%], of which 83 involved paracetamol), antihistamines (n = 31; 10.7%) psychotropics (n = 26; 8.9%), antibiotics (n = 21; 7.2%), vitamins (n = 20 [6.9%], of which 17 involved vitamin D), anticonvulsants (n = 13; 4.4%) and cold medicines (n = 11; 3.8%), followed by other drugs (n = 61; 21.1%). En three cases (1.0%) the error consisted in the administration of more than one drug (in every case, a combination of paracetamol and ibuprofen). We found significant differences in the distribution of involved drugs (P 0.04) in relation to patient age (Table 2). Although the most frequently involved drugs were antipyretics/analgesics, in infants under 2 mo, errors in the administration of vitamin D accounted for 40.0% of episodes, while 18 (70.0%) of the episodes involving psychotropic drugs occurred in children aged more than 6 years (Table 1).
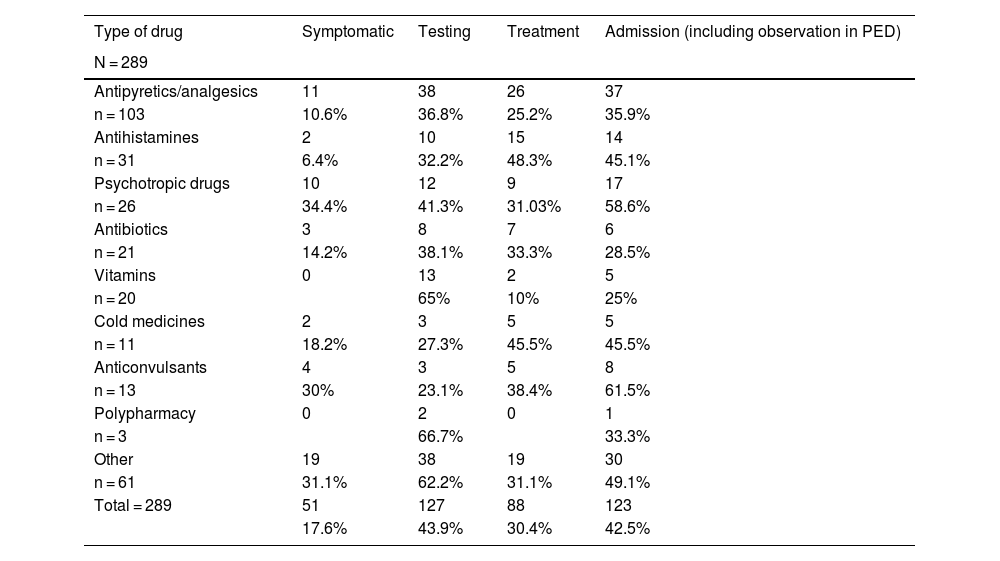
Presence of symptoms and management in the pediatric emergency department of visits due to dosing errors.
| Type of drug | Symptomatic | Testing | Treatment | Admission (including observation in PED) |
|---|---|---|---|---|
| N = 289 | ||||
| Antipyretics/analgesics | 11 | 38 | 26 | 37 |
| n = 103 | 10.6% | 36.8% | 25.2% | 35.9% |
| Antihistamines | 2 | 10 | 15 | 14 |
| n = 31 | 6.4% | 32.2% | 48.3% | 45.1% |
| Psychotropic drugs | 10 | 12 | 9 | 17 |
| n = 26 | 34.4% | 41.3% | 31.03% | 58.6% |
| Antibiotics | 3 | 8 | 7 | 6 |
| n = 21 | 14.2% | 38.1% | 33.3% | 28.5% |
| Vitamins | 0 | 13 | 2 | 5 |
| n = 20 | 65% | 10% | 25% | |
| Cold medicines | 2 | 3 | 5 | 5 |
| n = 11 | 18.2% | 27.3% | 45.5% | 45.5% |
| Anticonvulsants | 4 | 3 | 5 | 8 |
| n = 13 | 30% | 23.1% | 38.4% | 61.5% |
| Polypharmacy | 0 | 2 | 0 | 1 |
| n = 3 | 66.7% | 33.3% | ||
| Other | 19 | 38 | 19 | 30 |
| n = 61 | 31.1% | 62.2% | 31.1% | 49.1% |
| Total = 289 | 51 | 127 | 88 | 123 |
| 17.6% | 43.9% | 30.4% | 42.5% |
In a majority of cases, the exposure occurred in the home (n = 272; 94.3%), and in eight cases (2.7%) in health care facilities (sending hospital, primary care centers, dental clinics). In most cases, the child presented to the PED accompanied by a close relative (parents in 273 cases [94.5%], grandparents in 4 [1.4%]). The means of transport to the hospital was recorded in 269 of cases. In this subset of cases, the most frequent means of transport was a private vehicle (n = 255/269; 94.8%), followed by a patient transport vehicle (10/269; 3.7%). In 87 cases (30.6%), the patient had contact with other health care services prior to arrival to the PED (primary care pediatrician in 33 cases [11.4%], National Toxicology Institute in 30 [10.4%], emergency medical services in 18 [6.2%] and other type of resource in 6 [2.1%]). Of the patients who interacted with other services prior to arrival, only 13 (4.5%) received some form of prehospital treatment: activated charcoal (n = 10; 76.9%), naloxone (n = 1; 7.7%), normal saline infusion (n = 1; 7.7%) and oral dextrose (n = 1; 7.7%). More than half of the patients (n = 163; 56.4%) arrived to the PED within two hours of ingesting the wrong dose of the pharmaceutical.
Forty-nine patients were symptomatic (17.1%). The most frequent symptoms were neurologic (n = 23; 8.0%), followed by gastrointestinal symptoms (n = 13; 4.5%) and cardiovascular symptoms (n = 3; 1.0%), while the most frequent isolated symptom was somnolence (n = 10; 3.4%) followed by vomiting (n = 9; 3.1%). Diagnostic tests were performed in 118 cases (41.8%). In most instances (n = 62; 21%) they were nonspecific blood tests and electrocardiograms. In 12 patients, urine tests were performed to measure levels of pharmaceuticals and illicit drugs. In 42 (14.5%), tests were performed to measure serum levels of pharmaceuticals due to dosing errors, involving paracetamol in 39, valproic acid in two and alimemazine in one. In two patients (1.7%), the evaluation also included chest radiographs.
Eighty-three patients (28.7%) were treated in the PED. Fifty-three underwent gastrointestinal decontamination procedures (18.3%); 56 (19.4%) received a single dose of activated charcoal, delivered via feeding tube in 16 (28.6%), while 10 (3.5%) underwent gastric lavage (70% of these cases were managed between 2008 and 2014). Eleven patients (3.8%) received an antidote: eight (2.7%) received N-acetylcysteine, two (0.7%) biperiden and one (0.03%) naloxone.
Of the 289 episodes, 115 (39.8%) required stays of at least a few hours: 91 patients (31.5%) remained under observation in the PED, 20 (6.9%) were admitted to the inpatient ward, and 4 (1.4%) were admitted to the pediatric intensive care unit.
The interventions varied based on the substance involved in the episode (Table 2).
All patients had favorable outcomes, and there were no deaths.
DiscussionMedication dosing errors are the leading mechanism of poisoning in infants under 3 mo and continue to be an important mechanism until age 1 year. There are important differences in this type of poisonings based on the age of the child and the involved substance.3
Overall, in Spain, analgesics/antipyretics are the drugs involved most frequently in dosing errors and are usually administered by family members or caregivers. It is important to remember that paracetamol, the leading drug in this class, when administered repeatedly at doses exceeding the therapeutic range, e.g., in the context of febrile illness, can cause significant hepatotoxicity, and fatal cases have been reported in the pediatric population.10 The commercial distribution nationwide of formulations with different concentrations of a given active ingredient that is widely used for various conditions (e.g., paracetamol or ibuprofen) can contribute to the administration of an inappropriate dose.11
On the other hand, pharmaceuticals that are prescribed at very specific age ranges, such as vitamins in the first year of life, are also frequently involved in poisonings due to dosing errors. The one most frequently involved is vitamin D, whose continuous administration at doses above the established range can cause hypercalcemia and kidney injury.12
Both of these facts evince the need for health care professionals, during both the routine checkups of the healthy child program and pediatric visits due to acute diseases, to review with family members or caregivers any prescriptions for pharmaceuticals that they will be in charge of administering. This is all the more important considering that the vast majority of these episodes occur in the home.13
We consider knowledge of this type of poisoning essential in order to implement adequate preventive strategies. While the outcomes are generally favorable,4 more than 40% of the patients included in our study underwent some form of testing and were admitted to the observation unit of the PED or to hospital. The number that require admission to the pediatric intensive care unit was not negligible. On the other hand, our study shows that the development of symptoms or the need for testing or treatment after a dosing error is associated with the substance involved in the episode. Thus, dosing errors with psychotropic drugs were associated with the highest probability of developing symptoms, while dosing errors in the administration of vitamins were associated with a higher frequency of testing and dosing errors in the administration of cold medicines and antihistamines with a higher frequency of treatment. Thus, clinicians managing this type of poisonings must consider the type of drug involved in the episode from the outset, as it can help them estimate its potential severity.
The fact that some of the cases occurred in health care facilities warrants reflection on the importance of having specific measures in place in each organization to prevent this type of adverse event. It also highlights the importance of the ongoing training of health care professionals on pediatric poisonings,14 since, as our study demonstrated, some of these errors cause symptoms in patients and, depending on the drug involved, can cause severe poisoning, with a significant percentage of patients requiring admission, in some cases to the intensive care unit. The same could be said in regard to the approach to gastrointestinal decontamination. The fact that gastric lavage was performed in nearly 20.0% of patients managed with gastrointestinal decontamination is a reminder of the need to insist on ensuring the selection of the appropriate technique, for, while most episodes managed with gastric lavage clustered in the early years of the study (2008–2014), it is still being used with excessive frequency at present. It is worth noting that in general, in pediatric patients, as long as the involved substance is readily adsorbed, the indicated decontamination strategy is the administration of activated charcoal.14
There are several limitations to our study, chief of which is not having included the question of who administered the medication to the child in the register. While most events took place in the home, information of the involved caregiver could help finetune the design of preventive interventions.
To conclude, errors in the administration of medication are among the most frequent causes of pediatric poisoning in certain age groups, particularly in infants under three months. In addition, the involved pharmaceuticals vary with age throughout childhood, which should be taken into account in order to develop age-specific preventive measures.
CRediT authorship contribution statementJohanna Ramírez-Romero contributed to the concept and design of the study, supervised data collection, analyzed the data, wrote the initial draft of the manuscript and approved its final version.
Claudia Cifuentes and Beatriz Azkunaga revised the design, contributed to the analysis of the data and the critical revision of the manuscript.
Santiago Mintegi contributed to the concept and design of the study, supervised data collection, contributed to the analysis of the data and the critical revision of the manuscript and approved its final version.
The researchers included in the Appendix are members of the Working Group on Poisoning of the Sociedad Española de Urgencias de Pediatría and contributed the information on the poisoning episodes documented in their respective hospitals. All of them reviewed the final version of the manuscript.
FundingThis research did not receive any external funding.
HU Tajo: Hinojosa Mateo CM; H Quirón Bizkaia: Oliver P; HU Arnau de Vilanova: Pociello N; HU Basurto: Rodriguez Albarrán I; H Cabueñes: Rodriguez P, García A, Morán M; HU Carlos Haya: Oliva S; HU Navarra: Palacios M, Clerigué N; CH Jaén: Campo T; CAU Léon: Andrés AG, Muñiz M; CS Parc Taulí: Baena I, Bajja S; HU Cruces: Ramirez J; HU Doce de Octubre: Mesa S; HU Donostia: Muñoz JA. Muñoz MI; HU Dr. Peset: Rodriguez A; HU Francesc de Borja: Angelats CM, Vilaplana I; Fundació Sant Hospital de la Seu d’Urgell: Astete J; HU Fundación Alcorcón: Barasoain A; HU Gregorio Marañón: Vázquez P; H Infanta Cristina: Rodriguez MD; H Infanta Elena: Gómez C, Nuñez T; H Terrassa: Domenech F; H Laredo: Jorda A, Vega B; H Mendaro: Herrero L; HU Mutua Terrassa: Pizá A; HU Niño Jesús: Molina JC.; H Materno-Infantil Las Palmas de Gran Canaria: Mangione LH; H Materno-Infantil Badajoz: Ramiro L; C Asistencial Ávila: De Pedro S; H Montepríncipe, H Sanchinarro, H Torrelodones, H Puerta del Sur: González I; H Príncipe de Asturias: García MA; HU Puerta de Hierro: Benito C, Armero P; H Rey Juan Carlos: Sabrido G, Bello P; HU Río Hortega: Bullón I; H Sant Joan de Déu, Xarxa Hospitalaria i Universitaria de Manresa, Fundació Althaia: Botifoll E, Lobato Z; HU Sant Joan de Déu: Martínez Sánchez L, Luaces C, Algarrada L; H San Pedro: Martínez L; HU Salamanca: López J; H Virgen de la Salud: Aquino E; H Zumarraga: Pérez A; HU Politécnico La Fe: Señer R; H Mataró: Baena J; HU Marqués de Valdecilla, H Sierrallana: Peñalba A; H Gernika-Lumo: Alday A; H Miguel Servet: Campos C; HU Son Espases: López-Corominas V; C Asistencia Soria: Muñoz N; H Infantil La Paz: De Miguel B; Hospital C U Valencia: Khodayar P; H Severo Ochoa: Angulo AM; HU General de Villalba: Casado E; HU Santa Lucía: Ordoñez ME, HU Virgen del Rocío: Martínez I; Hospital Infanta Leonor: Angulo AN andHU Central de Asturias: Fernández R.
Appendix A lists the members of the Working Group of Poisoning of the Sociedad Española de Urgencias Pediátricas.
Meeting presentation: this study has been submitted for presentation at the XXIX Annual Meeting of the Sociedad Española de Urgencias de Pediatría, to be held between May 22–24, 2025.