Prematurity is associated with severe clinical conditions, long hospital stays, and uncertainty about patient outcomes. These circumstances lead to a stressful situation that may affect family functioning. The aim of this study was to study risk and protection factors affecting family functioning in preterm as compared to healthy term infants.
Population and methodsPreterm infants with and without pathological conditions (n=40) were recruited at 24 months post-conception age, together with a control group of healthy term newborn infants (n=31). Parents or usual caregivers responded to the Inventory of Family Protection Factors and Parental Stress scales. The results were compared using the Student's t test, unidirectional analysis of variance and the Tukey test.
ResultsParents of the control group attained higher scores than those of the preterm group for all the items studied; however, parents of preterm infants with pathological conditions perceived significantly less family resilience and more stress related to the upbringing of their child.
ConclusionsPrematurity itself is a risk factor for family dysfunction because it causes an elevated degree of parental stress and difficulties in the development of protection factors such as resilience.
La prematuridad se acompaña de patología severa, estancias prolongadas en el hospital e incertidumbre acerca del futuro de los pacientes. Estas circunstancias suponen un estrés que puede afectar al funcionamiento de la familia. El objetivo de este trabajo ha sido estudiar los factores de riesgo y de protección del funcionamiento familiar en prematuros comparados con neonatos sanos a término.
Población y métodosSe reclutó a prematuros que cursaron el periodo neonatal con y sin patología (n = 40) a los 24 meses de edad posconcepcional y un grupo control de nacidos a término sanos (n = 31) según datos de la historia clínica. El progenitor cuidador habitual respondió al Inventario de Factores de Protección Familiar y Escala de Estrés Parental. Los resultados se compararon mediante test de Student, análisis de variancia unidireccional y test de Tukey.
ResultadosLos padres del grupo control obtuvieron puntuaciones más elevadas que los de los prematuros en todos los parámetros estudiados. Los padres de prematuros sin patología se diferenciaron de los controles en 2 factores de resiliencia familiar: experiencias positivas y experiencias de compensación y en estrés, mientras que los padres de niños prematuros con patología percibieron significativamente menor resiliencia familiar y más estrés por la crianza de sus hijos.
ConclusionesLa prematuridad es un factor de riesgo para el funcionamiento familiar, ya que ocasiona un alto grado de estrés parental y dificulta el desarrollo de factores de protección como es la resiliencia.
The birth of a premature baby and his/her admission to hospital is an unexpected and traumatic event for the parents, which may affect family functioning.1 Some characteristics of premature babies, such as their difficulties interacting with the environment, their excessive nurturing demands, the acuteness of their pathology and uncertainty about their later development has been associated with parental stress and poor family functioning.2–5 However, in spite of these observations, some studies do not find the high level of stress that would be expected in families with premature children.6 We must point out that the negative effects of risk factors can be counteracted, at least partially, by certain protective factors, such as family resilience, which is defined as the internal and external resources of a family and their members.7 Thus, when a family experiences an adverse event such as the birth of a premature child, social support and resilience have been shown to be factors that protect them from the personal and social dysfunction of family and parents.8 Even though the family are the main setting for development and the first socialising agent during childhood, family functioning, risk factors and differences in stress and family load between families of healthy-term children and premature children have not been thoroughly studied.8,9
The purpose of this research was to analyse the differences between families of premature children with healthy development and without sequelae and families of healthy-term children two years after their birth, regarding both family dysfunction risk factors (parental stress) and protective factors (family resilience). Our hypothesis is that family dysfunction in premature-children families would be worse, expressing more stress and less resilience.
Patients and methodsDesignThis is a prospective, pilot study conducted at the Neurodevelopment office from the Neonatology Service of the Hospital Universitario y Politécnico La Fe (Valencia, Spain) for a period of 12 months (from June, 2012 to May, 2013), at the Beniopa Health Centre and at the Hospital Sant Francesc de Borja (Gandía).
The data collection was carried out when the patient attended a programmed visit 24 months after the birth (HUIP La Fe), or the Health Centre or Hospital (Gandía) for a routine check-up of the child. The Neurodevelopment office evaluates all premature babies of ≤28 weeks of gestation and performs the follow-up visits, a sequential assessment of all children born <1500g. In each case, the doctor in charge and/or the researchers informed the parents about the study and data confidentiality. The parent in charge of the upbringing of the child signed the consent and completed the questionnaires in an isolated setting.
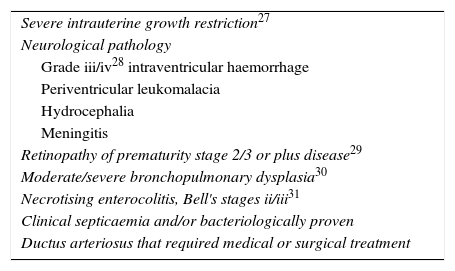
PopulationThe inclusion criteria were: (a) gestation age between 25+0 and 31+6; (b) admitted to the Neonatology Service (HUiP La Fe); (c) continuous follow-up visits according to protocol at the neonatal Neurodevelopment/Follow-up office until 24 months after birth; and (d) normal physical development and scales of development at the time of examination. The exclusion criteria included: (a) severe congenital malformations; (b) chromosomopathies; (c) persistent chronic pathology, sensory or neurocognitive deficits; (d) lack of informed consent; and (e) inability to understand Spanish. The study was performed comparing a premature-baby population with a control group comprising healthy-term newborns without pathologies. In addition, we performed a comparison within the group between premature babies who had a severe perinatal pathology (PCP) and the ones who had mild pathologies or no pathologies at all (PSP). The pathology that was taken into consideration for the inclusion in the PCP group is described in Table 1.
Pathology in <32-week-premature newborns identified as severe postnatal pathology (PP group) recruited to study the influence of perinatal pathology on the functioning of the family 24 months after birth.
| Severe intrauterine growth restriction27 |
| Neurological pathology |
| Grade iii/iv28 intraventricular haemorrhage |
| Periventricular leukomalacia |
| Hydrocephalia |
| Meningitis |
| Retinopathy of prematurity stage 2/3 or plus disease29 |
| Moderate/severe bronchopulmonary dysplasia30 |
| Necrotising enterocolitis, Bell's stages ii/iii31 |
| Clinical septicaemia and/or bacteriologically proven |
| Ductus arteriosus that required medical or surgical treatment |
Registry sheet1: perinatal data (gestation age, prenatal steroids, type of delivery, weight at birth, Apgar 1 and 5min)2; patient's severe pathology during admission and discharge (Table 1),3 and data from the progenitors (Table 2).
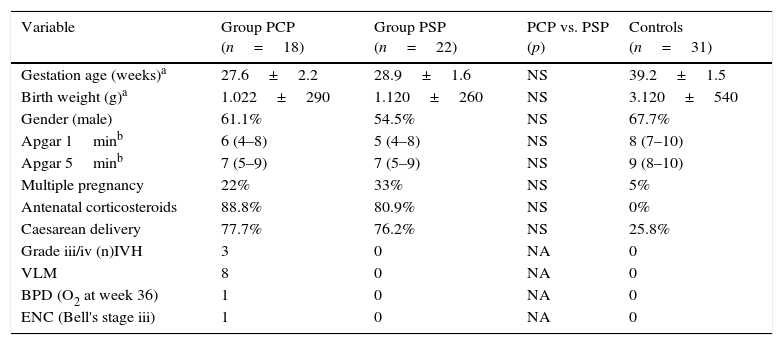
Characteristics of <32-week-premature newborns with postnatal pathology (PCP group) and without postnatal pathology (PSP group) recruited to study the influence of perinatal pathology on the functioning of the family. Healthy-term newborns are included as controls.
| Variable | Group PCP (n=18) | Group PSP (n=22) | PCP vs. PSP (p) | Controls (n=31) |
|---|---|---|---|---|
| Gestation age (weeks)a | 27.6±2.2 | 28.9±1.6 | NS | 39.2±1.5 |
| Birth weight (g)a | 1.022±290 | 1.120±260 | NS | 3.120±540 |
| Gender (male) | 61.1% | 54.5% | NS | 67.7% |
| Apgar 1minb | 6 (4–8) | 5 (4–8) | NS | 8 (7–10) |
| Apgar 5minb | 7 (5–9) | 7 (5–9) | NS | 9 (8–10) |
| Multiple pregnancy | 22% | 33% | NS | 5% |
| Antenatal corticosteroids | 88.8% | 80.9% | NS | 0% |
| Caesarean delivery | 77.7% | 76.2% | NS | 25.8% |
| Grade iii/iv (n)IVH | 3 | 0 | NA | 0 |
| VLM | 8 | 0 | NA | 0 |
| BPD (O2 at week 36) | 1 | 0 | NA | 0 |
| ENC (Bell's stage iii) | 1 | 0 | NA | 0 |
BPD: bronchopulmonary dysplasia; ENC: necrotising enterocolitis; IVH: intraventricular haemorrhage; VLM: periventricular leukomalacia; NA: not applicable; NS: non-significant.
Physical and neurological evaluation at the moment of recruitment: all patients were physically and neurologically examined at the time of their admission to the study.
Inventory of Family Protective Factors (family resilience)10: this measures the perception of a family in relation to the level of demands or stress factors and of protective factors (family resilience) that the family have experienced recently. It consists of four scales: (1) lower number of stress factors or positive experiences, which evaluates the perception of a family concerning whether they have experienced more positive events than problems associated with health, finance, family, friendships and work; (2) adaptive assessment, which measures a family's beliefs on the ability of their members to face problems with self-esteem, optimism, creativity and determination; (3) social support (items 9–12), which measures the perception of a family in relation to their ability to rely on people who support them, are concerned about them and protect them, and (4) compensation experiences (items 13–16), which measures the perception of a family in relation to their ability to face adversity, maintaining control and even coming out stronger. Cronbach's alpha was calculated for each of the four scales; this is an internal measurement for consistency that enables an estimate of the reliability of an instrument. The coefficients obtained for the four scales were 0.82, 0.78, 0.92 and 0.87, respectively, whereas the global one reached 0.88. All these coefficients can be considered as favourable, following the George and Mallery standards.11
Parental stress scale: we used the Spanish version12 of the Parental Stress scale,13 which measures the level of stress as a consequence of the parental role. It consists of a total of 17 items that make up two scales: (1) stress factors, which assess the level of stress fathers/mothers face in their parental role; (2) rewards, which measures the level of satisfaction that fathers/mothers experience in their parental role. Cronbach's alpha values were of 0.76 and 0.77, respectively.
StatisticsA descriptive statistic was performed for the perinatal and family parameters under study, including mean±standard deviation, or median and confidence intervals when the parameter required it. Biological parameters were compared using the Student's test when their distribution was normal, and non-parametric statistics were used when their distribution was not normal. In addition, the differences between the three groups were analysed (premature babies with pathologies, premature babies without pathologies and healthy-term babies) using the unidirectional analysis of variance and the Tukey test.
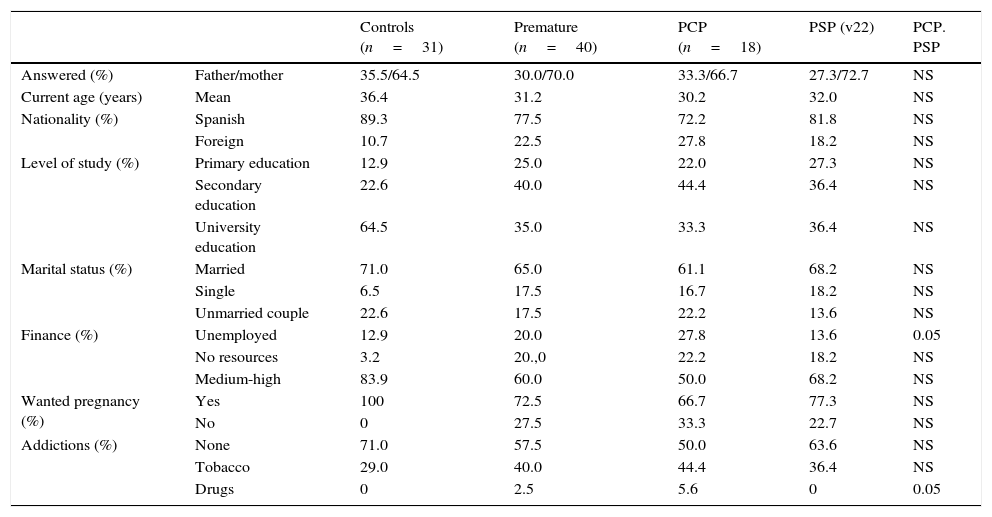
ResultsA total of 40 former premature children were recruited, of whom 18 had what is considered a severe pathology during their neonatal period (PCP group) and described in Table 1, whereas 22 did not have any pathology (PSP group). A total of 31 healthy 2-year-old preschool children was recruited as controls. The incidence of the pathology of the PCP and PSP group is described in Table 2. There were no significant differences in the most relevant variables related to perinatal factors, as shown in Table 2. There were also no differences related to the age of the parents between groups. The socio-economic characteristics of the parents are detailed in Table 3. The questionnaires were mostly answered by mothers, both for premature babies and for controls. In the group of healthy-term babies, a higher proportion of Spanish nationality progenitors was registered (89.3%) than in the group of premature babies without pathologies (81.8%) or with pathologies (72.2%). Parents with university degrees and of medium/high socio-economic status were also mostly among the group of healthy-term babies (64.5 and 83.9%). On the other hand, the percentage of unwanted pregnancies and addiction was higher within the groups of premature-baby parents (Table 3). There were no relevant differences in financial position between the parents of premature babies with and without pathologies. However, there was a higher level of on-and-off drug use within the PCP group (p<0.05).
Characteristics of parents of 32-week premature babies with severe postnatal pathologies (PCP) and without postnatal pathologies (PSP) and healthy-term babies recruited to study the influence of prematurity on the functioning of a family.
| Controls (n=31) | Premature (n=40) | PCP (n=18) | PSP (v22) | PCP. PSP | ||
|---|---|---|---|---|---|---|
| Answered (%) | Father/mother | 35.5/64.5 | 30.0/70.0 | 33.3/66.7 | 27.3/72.7 | NS |
| Current age (years) | Mean | 36.4 | 31.2 | 30.2 | 32.0 | NS |
| Nationality (%) | Spanish | 89.3 | 77.5 | 72.2 | 81.8 | NS |
| Foreign | 10.7 | 22.5 | 27.8 | 18.2 | NS | |
| Level of study (%) | Primary education | 12.9 | 25.0 | 22.0 | 27.3 | NS |
| Secondary education | 22.6 | 40.0 | 44.4 | 36.4 | NS | |
| University education | 64.5 | 35.0 | 33.3 | 36.4 | NS | |
| Marital status (%) | Married | 71.0 | 65.0 | 61.1 | 68.2 | NS |
| Single | 6.5 | 17.5 | 16.7 | 18.2 | NS | |
| Unmarried couple | 22.6 | 17.5 | 22.2 | 13.6 | NS | |
| Finance (%) | Unemployed | 12.9 | 20.0 | 27.8 | 13.6 | 0.05 |
| No resources | 3.2 | 20.,0 | 22.2 | 18.2 | NS | |
| Medium-high | 83.9 | 60.0 | 50.0 | 68.2 | NS | |
| Wanted pregnancy (%) | Yes | 100 | 72.5 | 66.7 | 77.3 | NS |
| No | 0 | 27.5 | 33.3 | 22.7 | NS | |
| Addictions (%) | None | 71.0 | 57.5 | 50.0 | 63.6 | NS |
| Tobacco | 29.0 | 40.0 | 44.4 | 36.4 | NS | |
| Drugs | 0 | 2.5 | 5.6 | 0 | 0.05 |
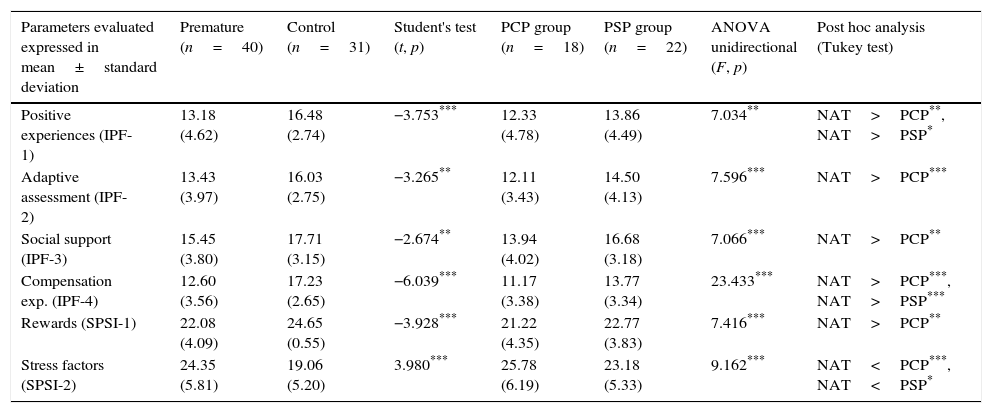
Table 4 shows that parents from the control group have significantly higher scores than parents from the group of premature babies in each family resilience factor: positive experiences, adaptive assessment, social support and compensation experiences (t=−3.753, p<0.001; t=−3.265, p<0.01; t=−2.674, p<0.01; t=−6.039, p<0.001). The differences were also statistically significant in relation to reward and stress perception. Parents of premature babies perceived fewer rewards and more stress than the ones from the control group (t=−3.928, p<0.001; t=3.980, p<0.001).
Analysis of descriptive and median differences of the results of the instruments: inventory of family protective factors (IFP)/family resilience, family stress scale (SPS) and Gratitude questionnaire (GQ-6) completed by the parents of <32-week premature newborns with severe postnatal pathology (PCP group) and without postnatal pathology (PSP group) recruited to study the influence of perinatal pathology on the functioning of the family 24 months after birth.
| Parameters evaluated expressed in mean±standard deviation | Premature (n=40) | Control (n=31) | Student's test (t, p) | PCP group (n=18) | PSP group (n=22) | ANOVA unidirectional (F, p) | Post hoc analysis (Tukey test) |
|---|---|---|---|---|---|---|---|
| Positive experiences (IPF-1) | 13.18 (4.62) | 16.48 (2.74) | −3.753*** | 12.33 (4.78) | 13.86 (4.49) | 7.034** | NAT>PCP**, NAT>PSP* |
| Adaptive assessment (IPF-2) | 13.43 (3.97) | 16.03 (2.75) | −3.265** | 12.11 (3.43) | 14.50 (4.13) | 7.596*** | NAT>PCP*** |
| Social support (IPF-3) | 15.45 (3.80) | 17.71 (3.15) | −2.674** | 13.94 (4.02) | 16.68 (3.18) | 7.066*** | NAT>PCP** |
| Compensation exp. (IPF-4) | 12.60 (3.56) | 17.23 (2.65) | −6.039*** | 11.17 (3.38) | 13.77 (3.34) | 23.433*** | NAT>PCP***, NAT>PSP*** |
| Rewards (SPSI-1) | 22.08 (4.09) | 24.65 (0.55) | −3.928*** | 21.22 (4.35) | 22.77 (3.83) | 7.416*** | NAT>PCP** |
| Stress factors (SPSI-2) | 24.35 (5.81) | 19.06 (5.20) | 3.980*** | 25.78 (6.19) | 23.18 (5.33) | 9.162*** | NAT<PCP***, NAT<PSP* |
Healthy-term newborns are included as controls. Analysis performed using the Student's test (premature group, control group), ANOVA unidirectional and Tukey test (PCP group, PSP group, control group).
NS: p>0.05.
The differences between premature babies and control group babies were also examined taking both premature groups (PCP and PSP) separately. The parents of healthy-term babies had significantly higher scores than the parents of premature babies with pathologies in every factor that measured family resilience, positive experiences, adaptive assessment, social support and compensation experiences, and there were statistically significant differences (F=7.034, p<0.01; F=7.596, p<0.001; F=7.066, p<0.01; F=23.433, p<0.001). In the case of parents of premature babies without pathologies, there were significant differences with healthy-term babies in just two family resilience factors, positive experiences and compensation experiences (F=7.034, p<0.01; F=23.433, p<0.001). On the other hand, parents of premature babies with pathologies perceived significantly fewer rewards, more stress and less gratitude for raising their children than parents of healthy-term babies (F=7.416, p<0.001; F=9.162, p<0.001; F=4.600, p<0.05). However, between the group of parents of premature babies without pathologies and healthy-term babies there were no significant differences in the perception of rewards, but there were in perceived stress, which was higher in the group of parents of premature babies without pathologies than in the group of parents of healthy-term babies.
DiscussionIn general, the survival rate for extreme premature babies has increased in the last few years.14,15 Nevertheless, intact survival has not changed significantly over the same period.16 Within the social setting, the family will have a preponderant role in respect to having a positive or negative influence on the premature baby's future. Therefore, depending on the characteristics of the family and its ability to face the situation that will derive from having a premature child, this social group will become a positive agent regarding the inclusion and development of the child when he/she becomes an adult or, on the contrary, it will become a negative factor that will hinder this process.17,18
The results of this study reflect that prematurity causes lower family functioning, since it generates greater stress and less resilience compared to a standard of normal healthy-term children at the age of two. However, parents of premature babies without pathologies are not different from control group parents in the perception of rewards for the raising of their children. These results seem to indicate that the satisfaction parents of relatively healthy premature babies perceive about their raising does not differ from that of parents of healthy-term babies at the age of two. However, in spite of that, the compensation experiences that the raising of the child provide do not behave as a sufficient protective factor capable of absorbing the parent's stress when facing prematurity. Our results are consistent with a few previous studies that have found a higher level of stress among premature-baby families than in those of healthy-term babies.17,18 A recent meta-analysis concluded that premature-baby parents only perceived slightly more stress than parents of healthy-term babies. The notion that premature-baby parents experience the same level of stress as the parents of healthy-term babies indicates that the parents’ social and cultural level, the family's social support, the birth weight or the baby's health can be factors that mediate prematurity and parental stress.2 Therefore, it would be particularly relevant in subsequent research studies to identify which aspects of prematurity induce parental stress and which parental factors are protective, in order to develop programmes that optimise these aspects. Some studies performed with premature-baby families have analysed the importance of promoting family resilience to overcome stress and successfully face the challenges these type of families encounter.19,20 Family resilience is developed when the family's protective factors such as resources, adaptive ability and social support are activated, and it is inhibited when risk factors are promoted, such as demands or stress. This is more a process than a result and can vary over time.21 By measuring resilience we can understand the interaction between demands and stress factors, and protective factors that a family experiences within a given situation. In our study, we found that premature-baby parents with pathologies showed a lower level of family resilience than parents from the control group. That is to say, they perceived that their family had more demands, more stress factors and fewer protective factors than the parents in the control group. It must be pointed out that parents of premature babies without pathologies did not differ from the control group in two family resilience factors, such as the perception of the ability the family has to adapt to adversity and the social support they received. During recent decades, various research studies have shown that perceived social support is one of the main resources people have when they suffer from stress in general22 and, particularly, it is an important resource for parents when they face prematurity.23 On the contrary, the lack of social support under stressful situations can increase vulnerability and psychological problems in parents and harm family functioning.24
There are several limitations to this study. As a limitation of this research study, we must point out it is a cross-sectional study with self-administered questionnaires, whereas in future research it would be preferable to perform longitudinal studies that could capture changes in these variables before and after a premature birth. In addition, in this research study, most of the parents who answered the questionnaires were mothers. However, the literature thoroughly documents that the role of the father constitutes a supportive and protective factor for the mother and for the functioning of the family.18 It would also be interesting to analyse the effect prematurity has both on parental roles and on marital roles, and on the way it affects the rest of the family members. Lastly, it is possible that other factors that were not taken into consideration in this study, such as the amount of time the baby is hospitalised, the parent's mental health or marital satisfaction, can contribute to the functioning of the families of premature children, so these variables should be studied in more depth in future studies.
Based on our study, we can conclude that prematurity, particularly when it is associated with perinatal pathologies and when it coexists with psychosocial-type risk factors, is a decisive factor for family dysfunction that significantly increases parental stress and limits the adoption of protective factors such as resilience. The coexistence of these factors must be taken into consideration by the professionals who assist these patients, who will need to take proactive measures to offer psychological support and regular assessments in neonatal follow-up consultations. These families would greatly benefit from well-designed interventions, whose objective should be to help them look for psychological, emotional and material support, teaching them to use their resources, both material and psychological, to successfully face the potential stress raising a premature child implies.25,26
FundingTo conduct this study, we received funding from the Maternal and Child Health Network (Red de Salud Materno Infantil y del Desarrollo, SAMID) from the Instituto Carlos III (RD12/0026/0012) granted to M. Vento.
Conflicts of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Escartí A, Boronat N, Llopis R, Torres R, Vento M. Estudio piloto sobre el estrés y la resiliencia familiar en recién nacidos prematuros. An Pediatr (Barc). 2016;84:3–9.